Safer Intubation Checklist.
Paediatric intensive care retrieval services
Whether you are a career paediatric anaesthetist or not, if you work in a centre without an on-site paediatric intensive care unit (PICU) it is likely that you will be called to assist if a critically ill child presents to your hospital.
Anaesthetic involvement is usually required to help stabilize critically ill babies and children and initiate intensive care prior to their transfer to a PICU. This can be a daunting task, especially if several years have passed since your last paediatric attachment, or your exposure to very sick children has been limited.
In general, paediatric intensive care transfer teams will undertake transfer of critically ill children to specialist centres. There will be an expectation, however, that you should start stabilizing the child prior to the transfer team’s arrival. Often the transfer team can offer excellent clinical advice and support prior to their arrival; many have websites that contain useful resources such as clinical guidelines, drug calculators, checklists and even apps that you can download that may prove invaluable.
An example of a checklist developed by the KIDS retrieval service for a ventilated child is shown in Figure 31.2[7].
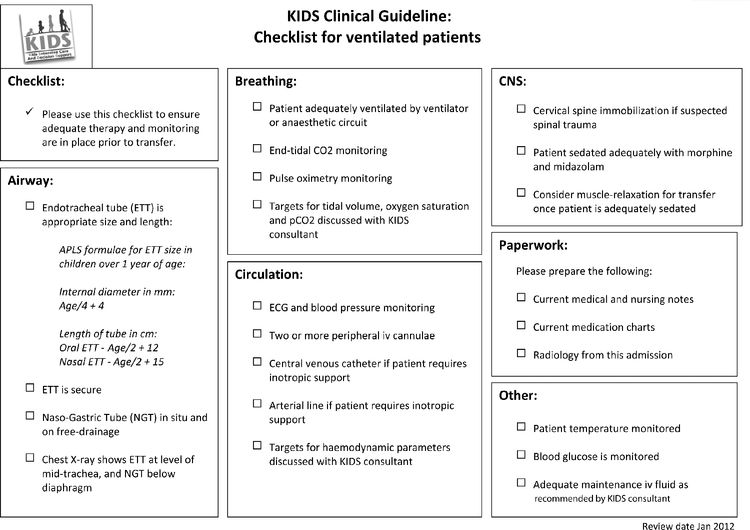
Checklist for ventilated patients.
Useful resources/websites
- www.kids.bch.nhs.uk
Kids Intensive Care and Decision Support
Birmingham Children’s Hospital
- www.cats.nhs.uk
Children’s Acute Transfer Service
Great Ormond Street Hospital
- http://www.strs.nhs.uk
South Thames Retrieval Service
Evelina Children’s Hospital, located at St Thomas’ Hospital
- http://www.sort.nhs.uk
Southampton Oxford Retrieval Team
Southampton General Hospital and the Radcliffe Hospital
- http://www.nwts.nhs.uk
North West & North Wales Paediatric Transport Service
Royal Manchester Children’s Hospital and Alder Hey Children’s Hospital
- http://www.sheffieldchildrens.nhs.uk
Embrace transfer service for Yorkshire and the Humber
Sheffield Children’s Hospital
Management of patients with traumatic brain injury
The principles of management of traumatic brain injury are important to all anaesthetists and have been covered in questions included in Chapters 7 and 16. A useful algorithm has been developed by St George’s neurocritical care unit[8] and is shown in Figure 31.3. This should aid management of patients with head injuries.
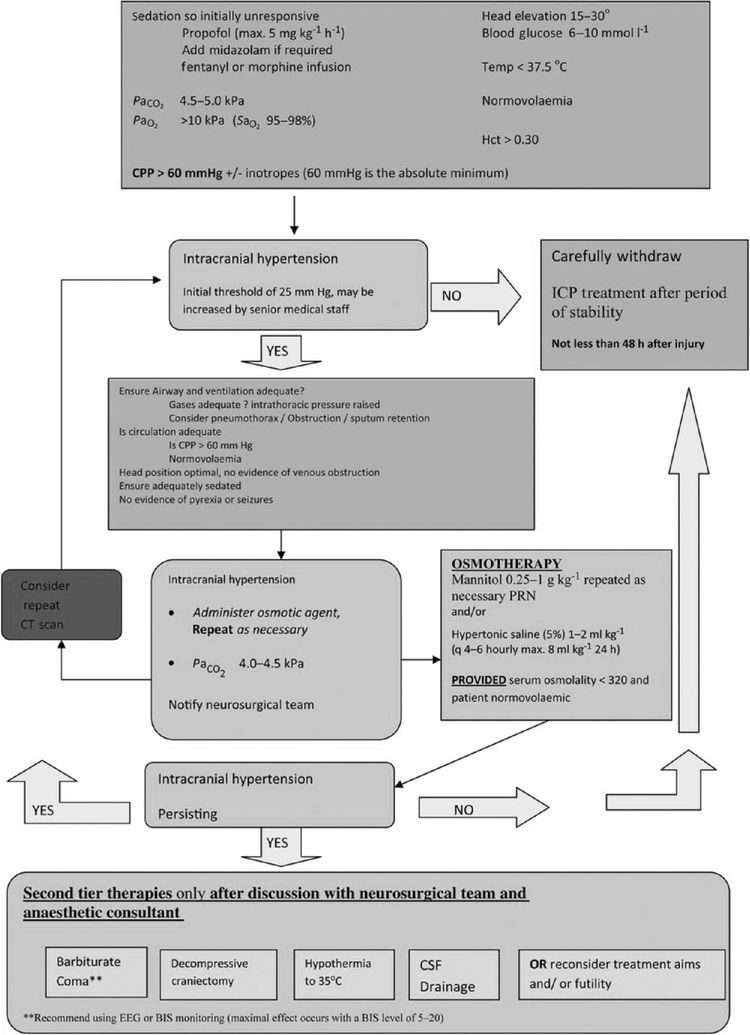
Management algorithm for patients with severe traumatic brain injury.
National Tracheostomy Safety Project Guidelines
Patients with tracheostomies are not only commonplace in the ICU, but many are now managed in the ward environment. The NAP4 audit found that tracheostomy complications were attributable to half of all airway-related deaths and cases of brain damage in critical care.
The National Confidential Enquiry into Patient Outcome and Death (NCEPOD) published a report (On the Right Trach?) in 2014 which reviewed care received by patients who underwent tracheostomy insertion. One of the principal recommendations was that bedside staff caring for tracheostomy patients must be competent in recognizing and managing common airway complications, including tube obstruction or displacement[9].
The National Tracheostomy Safety Project (NTSP) is a UK-based group that was developed to improve the management and care of patients with tracheostomies. The NTSP have developed educational resources and emergency guidelines for all healthcare professionals to follow in the event of an airway problem in both laryngectomy patients and those with tracheostomies[10].
As an anaesthetist you are very likely to be called to help at any emergency involving these patients, therefore it is essential that you know the emergency NTSP guidelines and are able to deal with common problems such as tube blockage and dislodgement quickly and safely. The guidelines highlight early use of oxygen on the stoma and the face, early use of capnography and connection to a Mapleson C circuit. This may be obvious, but remember that it is impossible to orally intubate a patient with a laryngectomy.
The NTSP guidelines for tracheostomy emergencies (Figure 31.4) and laryngectomy patients (Figure 31.5) are shown[11].

Emergency tracheostomy management.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





