Chapter 7 Intensive care
Acute Respiratory Distress Syndrome (ARDS)
Causes
| Direct injury | Indirect injury |
|---|---|
| Pulmonary contusion | Septicaemia |
| Gastric aspiration | Major trauma |
| Fat and amniotic fluid embolus | Cardiopulmonary bypass |
| Infection | Massive blood transfusion |
| Cytotoxic drugs | Prolonged hypotension |
| Smoke inhalation | Hepatic and renal failure |
| Oxygen toxicity | Disseminated intravascular coagulation |
Pathophysiology
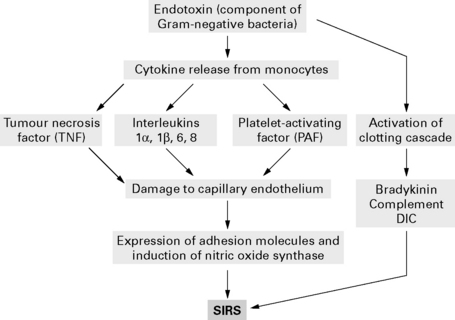
Activated neutrophils adhere to endothelial cells and release inflammatory mediators, including oxygen-free radicals and proteases, to cause lung damage. Direct lung damage or endotoxins alone are sufficient to damage endothelial cells with cytokine release and an inflammatory cascade (Fig. 7.1).
Treatment
Treat underlying cause
Other methods of improving oxygenation
 and arterial oxygenation. Long-term benefits have not been proven.
and arterial oxygenation. Long-term benefits have not been proven.Secondary infection. High risk of secondary infection reduced with prophylactic antibiotics.
Acutely Ill Patients in Hospital: Recognition of and Response to Acute Illness in Adults in Hospital
National Institute for Clinical Excellence 2007
Guidance
Chan K.P., Stewart T.E., Mehta S. High-frequency oscillatory ventilation for adult patients with ARDS. Chest. 2007;131:1907-1916.
Dernaika T.A., Keddissi J.I., Kinasewitz G.T. Update on ARDS: beyond the low tidal volume. Am J Med Sci. 2009;337:360-367.
Malarkkan N., Snook N.J., Lumb A.B. New aspects of ventilation in acute lung injury. Anaesthesia. 2003;58:647-667.
McLuckie A. High-frequency oscillation in acute respiratory distress syndrome (ARDS). Br J Anaesth. 2004;93:322-323.
Moloney E.D., Griffiths M.J.D. Protective ventilation of patients with acute respiratory distress syndrome. Br J Anaesth. 2004;92:261-270.
NICE. Quick reference guide. Acutely ill patients in hospital. NICE clinical guideline, 2007;50. www.nice.org.uk/nicemedia/pdf/CG50QuickRefGuide.pdf.
Rouby J.-J., Consstantin .J-M., Girardi C.R., et al. Mechanical ventilation in patients with acute respiratory distress syndrome. Anesthesiology. 2004;101:228-234.
Cardiovascular System
Inotropes
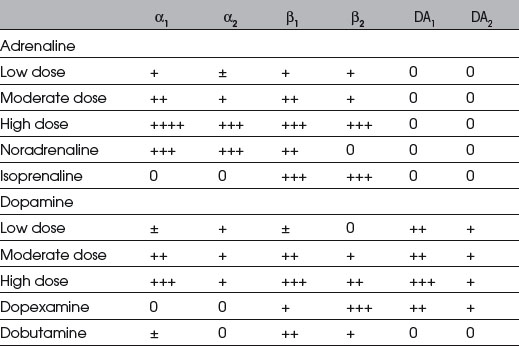
If shock persists despite adequate volume replacement and vital organ perfusion is jeopardized, inotropic drugs may be required to improve blood pressure and cardiac output (Table 7.2).
Adrenergic receptor function
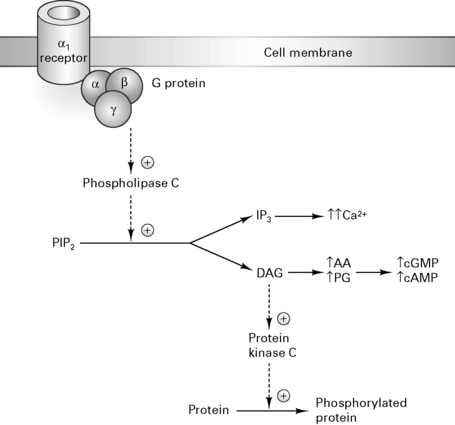
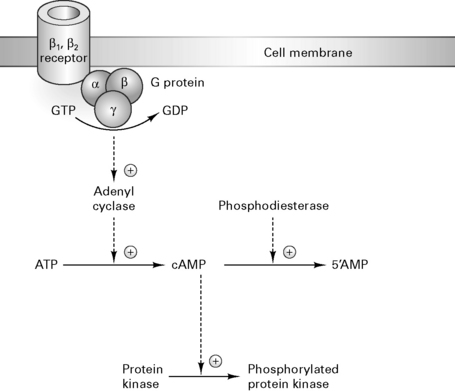
α1 receptors activate phospholipase C which cleaves phosphoinositol 4,5-biphosphate (PIP2) to diacylglycerol (DAG) and inositol triphosphate (IP3). DAG activates protein kinase C to release arachidonic acid which increases cGMP synthesis (Fig. 7.2). Activation of β1, β2 and dopamine (D1) receptors triggers the conversion of ATP to cAMP, activating protein kinase C and triggering protein phosphorylation which causes tachycardia and increases contractility (Fig. 7.3).
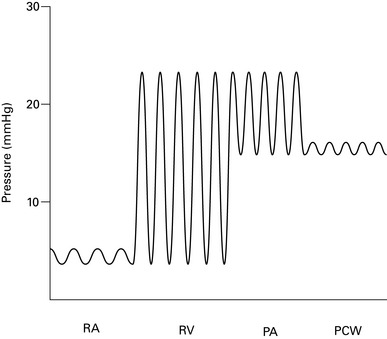
Pulmonary artery catheters
Indications
Complications
Table 7.3 Complications of pulmonary artery catheter insertion
| Associated with insertion | Associated with catheter presence |
|---|---|
| Pneumothorax/haemothorax | Infection of catheter or site |
| Haematoma | Pulmonary thrombosis/infarct |
| Cardiac arrhythmias | Cardiac arrhythmias |
| Arterial puncture | Valve damage/endocarditis |
| Pulmonary artery perforation | Pulmonary artery erosion |
| Catheter knotting | Thrombocytopenia |
| Cardiac valve damage |
Cardiac output monitoring
Invasive techniques
Non-invasive techniques
American Society of Anesthesiologists Task Force on Pulmonary Artery Catheterization. Practice guidelines for pulmonary artery catheterization. Anesthesiology. 2003;99:988-1014.
Antonelli M., Levy M., Andrews P.J., et al. Hemodynamic monitoring in shock and implications for management. International Consensus Conference. Intensive Care Med. 2007;33:575-590.
Dawson S., Jhanji S., Pears J.R.M. Cardiac output monitoring: basic science and clinical application. Anaesthesia. 2008;63:172-181.
Jhanji S., Dawson J., Pearse R.M. Cardiac output monitoring: basic science and clinical application. Anaesthesia. 2008;63:172-181.
Klein A.A., Snell A., Nashef S.A., et al. The impact of intra-operative transoesophageal echocardiography on cardiac surgical practice. Anaesthesia. 2009;64:947-952.
Moppett I., Shajar M. Transoesophageal echocardiography. BJA CEPD Rev. 2001;1:72-75.
Van Lieshout J.J., Wesseling K.H. Continuous cardiac output by pulse contour analysis? Br J Anaesth. 2001;86:467-469.
Fluid and Electrolyte Balance
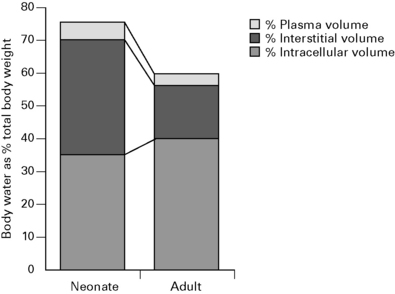
The neonate has a greater proportion of body water and in a different distribution than the adult (Fig. 7.5). More fluid is distributed within the extracellular compartment (interstitial and plasma volume) compared with the adult, resulting in a larger volume of distribution for water-soluble drugs. A large proportion of interstitial fluid is excreted within the first few weeks after birth and adult levels are attained by adolescence.
A 70 kg male has about 42 kg of water distributed through three body compartments.
Normal fluid requirements
Postoperative fluid requirements
Intravenous fluids administered perioperatively during minor gynaecological surgery reduce morbidity, particularly nausea and dizziness. However, blood coagulation appears to be accelerated by haemodilution with saline, and in patients undergoing elective abdominal surgery, the incidence of DVT was four times greater than in the fluid-restricted group (Janvrin et al 1980).
Albumin
Benefits of correcting hypoalbuminaemia are unclear. A prospective randomized study of 475 ICU patients comparing albumin and gelatin solutions failed to show any benefit (Stockwell et al 1992). In 70 children with burns, albumin supplementation failed to improve morbidity or mortality (Greenhalgh et al 1995). In septic patients, albumin infusions will only increase COP for a relatively short period. Increased capillary permeability results in >60% of albumin leaving the intravascular compartment within 4 h, potentially worsening oedema.
A controversial systematic review by the Cochrane Group of 23 randomized controlled trials found that the risk of death was 6% greater in the group treated with albumin compared with those receiving crystalloids or no treatment (Cochrane Injuries Group 1998). The Committee on Safety of Medicines now advises doctors to restrict the use of, and take special care when using, human albumin, but states that there is ‘insufficient evidence of harm to warrant withdrawal of albumin’. Hypoalbuminaemia in itself is not an appropriate indication. Risks of hypervolaemia and cardiovascular overload warrant monitoring in patients receiving albumin.
Intravenous fluids
Crystalloids
0.9% normal saline (per 1000 mL)
Dextrose saline (per 1000 mL) (4% dextrose, 0.18% saline)
Colloid versus crystalloid controversy (Table 7.4)
Table 7.4 Comparison of crystalloids and colloids
| Advantages | Disadvantages | |
|---|---|---|
| Crystalloid | Cheap | Larger volumes needed |
| Replaces extravascular loss | Small ↑ in plasma volume | |
| Increased GFR | Peripheral and pulmonary oedema | |
| Minimal effect on clot quality | ||
| Colloid | Smaller volumes needed | Risk of anaphylaxis |
| Prolonged ↑ in plasma volume | Relatively expensive | |
| Reduced peripheral oedema | Coagulopathy | |
| Poor clot quality |
British Consensus Guidelines on Intravenous Fluid Therapy for Adult Surgical Patients
Summary and recommendations
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree