1. While the incidence of burns is decreasing in western countries, 20% of burns are seen in children <5 years of age and 29% in children <16 years of age.
2. The “Rule of Nines” used to evaluate the body surface area burned must be modified from the percentages used in adults for infants and children.
3. Electrical burns often have significant internal injuries not obvious from the extent of cutaneous involvement.
4. Initial management goals in the care of burned patients include fluid resuscitation, management of electrolytes, airway control, and heat regulation.
5. Epidermis bullosa is a congenital group of blistering skin disorders, classified based on the affected skin layer and structural proteins.
6. Any shearing forces or minor trauma can cause blisters in affected patients.
INTRODUCTION
The anesthesiologist usually encounters skin as an organ upon which monitoring electrodes and devices are placed, and through which vascular catheters are placed and secured. The skin may bear lumps and bumps to be excised, lacerations to be cleansed, and wounds to be closed or sutured. However, skin is one of the largest, most metabolically active organs, and has numerous roles.
1. Protective: Guards the body from chemical, thermal, or mechanical injury. This includes harmful environmental elements such as solar radiation and weather.
2. Immunologic: Prevents entry of microorganisms, and a surface film of lipid secretions from sebaceous glands creates an antiseptic layer.
3. Fluid and protein balance: Reduces loss of fluid and moisture.
4. Thermoregulation: Insulates to decrease heat loss; also allows for rapid cooling through sweating and vasodilation.
5. Neurosensory: Nerve endings and receptors enable the nervous system to process and interpret information (pain, touch, heat, and cold).
6. Metabolism: Supports the production of vitamin D.
7. Social-interactive: Facilitates behavioral, interpersonal, and social development.
8. Storage function: Skin is the largest iron-storing organ in the body.
Severe skin injury will compromise all of the usual roles it fulfills, presenting substantial anesthetic challenges. While Table 27.1 lists a variety of severe skin disorders, most of the operating room (OR) and anesthetic challenges can be illustrated by using two examples—the treatment of burns and epidermolysis bullosa (EB).
DISORDER: Burns
CLINICAL PEARL Burned patients are in a hypermetabolic state with increased O2 consumption and CO2 production, and greatly increased fluid requirements.
The precise incidence of pediatric burn injuries worldwide is unknown. It has declined in western countries, but morbidity and mortality from burns remains a serious problem in less developed nations. Africa has the highest rate of hospitalization for pediatric burns, and the death rate may be approaching 10-fold of that reported in the Americas. Owing in part to a larger population, more than half of the world’s pediatric burn patients reside in Asia (1,2). According to the American Burn Association 2014 National Burn Repository, a collection of data from 96 hospitals in 35 states and the District of Columbia, 29% of burns occur in children less than 16 years of age. 19% are children under the age of 5 years. Males outnumber females in all age categories. The most common etiologies are fire/flame and scalds, with scalds being most prevalent in children under 5 years of age. Improved efficiency and quality of burn care is evidenced by decreased mortality rates and reduced overall length of hospital stay in the past decade (3,4).
TABLE 27.1 Severe skin disorders
Inflammatory reactions of the skin | Etiology | Treatment |
Drug eruptions |
|
|
Toxic epidermal necrolysis (TEN) | Drugs in approximately one third of cases; unknown in the remaining cases | Identify and discontinue the causative drug, if known; corticosteroids; supportive care |
Erythema multiforme | Drugs or X-ray treatment in approximately half of cases; unknown in others; infectious agents in younger patients | Identify and discontinue a causative drug; identify and treat infectious agent Supportive care Corticosteroid use is controversial |
Stevens–Johnson syndrome | A more severe form of erythema multiforme, with severe mucocutaneous manifestations |
|
Bullous diseases |
|
|
Pemphigus | Autoimmune disease with IgG antibodies that bind to the epidermis; primarily occurs in middle-aged and older persons | Systemic corticosteroids; vigilance for secondary skin infection; reverse isolation |
Bullous pemphigoid | Autoimmune disease characterized by antibodies that bind against the basement membrane of the epidermis; seen mainly in the elderly | Systemic or topical corticosteroids |
Epidermolysis bullosa (see text for details) |
|
|
IgG, immunoglobulin G.
CLASSIFICATION
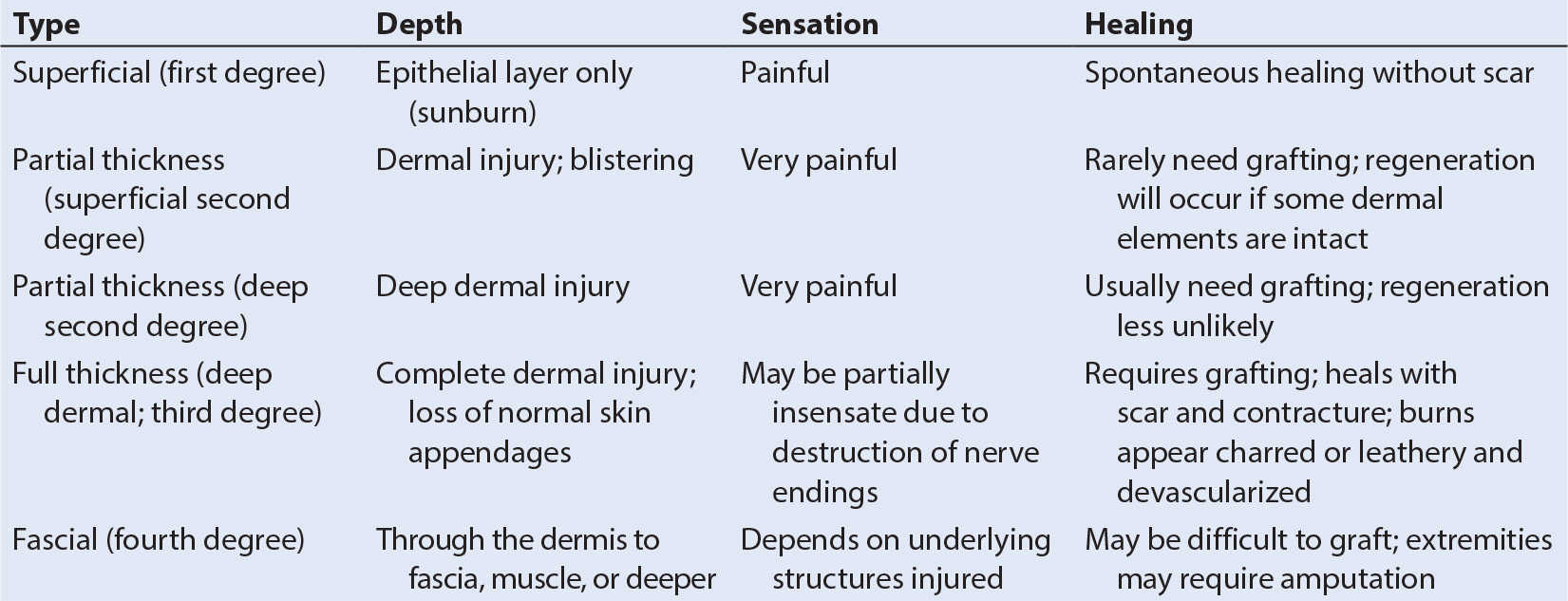
1. Burns are generally classified according to depth of injury (Table 27.2), percentage of total body surface area affected, and etiology.
2. Severity of the burn is indicated by depth, location, percentage of total body surface area affected, presence or absence of inhalation injury, associated trauma, and underlying comorbidities.
a. Burn injury located on the face, hands, feet, or genital areas is more concerning and may modify treatment. Circumferential burns require special attention. Those affecting the chest and abdomen can cause severe restriction of ventilation and cardiac output, and abdominal compartment syndrome. Those of the extremities can cause ischemia. These burns usually require urgent escharotomy (5).
b. Total body surface area (TBSA) affected should be mapped on a pediatric burn chart. The “Rule of Nines” must be modified in infants and children because the head is disproportionately larger (2,6,7).
c. Facial burns and inhalation injury compromise the airway and produce severe edema within hours of the burn. The airway must be secured in these patients as soon as possible before swelling renders it impossible (also see Chapter 37). Victims with inhalation lung injury can develop acute respiratory failure.
3. Etiologies include fire/flame, scald, thermal contact electrical, chemical, and friction (3).
a. Flame burns, especially those sustained in a closed space such as a house, are commonly associated with inhalation burns (7).
b. Electrical burns are unique. The extent of internal damage may be difficult to determine from an initial external examination, particularly following high voltage injury (7–9).
i. Even when the overlying skin appears normal, myocardial injury, ruptured viscus, fractures (from violent muscle contraction) and widespread deep tissue necrosis may be seen.
ii. Severe myoglobinuria and hyperkalemia from myonecrosis is common and can result in renal tubular injury.
iii. Osmotic diuresis with mannitol and alkalinization of the urine should be initiated as soon as possible.
iv. Fasciotomy for decompression may be required in the first 24 hours to prevent ischemia of extremities, similar to a circumferential burn, and debridement of nonviable deep tissue may be necessary early in the course (10).
INITIAL MANAGEMENT
1. Fluid resuscitation is the centerpiece of initial management in acute burns. It is critical to address massive fluid losses following the burn.
a. Urine output may not accurately reflect the adequacy of administered volume. Anuria and renal failure are invariably fatal, and must be avoided.
b. The modified Parkland formula, which utilizes a balanced isotonic salt solution, such as normal saline or Lactated Ringer’s, is most commonly used to calculate the first 24 hours fluids (2,6,7,11,12):
4.0 mL per kg × % TBSA burned × weight (kg)
Half of this volume is given over 8 hours, and the remainder over the next 16 hours, all in addition to the normal maintenance fluid requirement.
c. Hypertonic (3%) saline been advocated as a means of restoring circulating volume, but has not been shown to improve outcomes (10).
d. This initial fluid resuscitation is usually completed before the child’s first visit to the OR. But emergent needs, such as severe electrical burns, may bring some severely injured children to the OR early.
i. In those cases, blood and additional third-space losses due to surgical excision must be factored in as well.
ii. When calculating intraoperative fluid requirements during excision and grafting, one must remember to account for the increased evaporative and third-space losses from burned areas not undergoing surgery.
2. Airway control is the most critical issue in the first hours following suspected inhalation injury.
a. Any patient who is burned in a closed space, such as a house fire, must be assumed to have an inhalation injury.
b. Consider inhalation injury with flame burns to any site.
c. Edema of the internal and external airway can make intubation impossible if delayed. All patients with facial burns or significant inhalation injury should be intubated immediately.
CLINICAL PEARL Early control of the airway is the most critical issue following suspected inhalation injury; these patients should be intubated immediately.
3. Ventilation goals are important in addressing increased oxygen consumption and CO2 production.
a. Greatly improved outcomes have been reported using ventilator strategies pioneered for acute respiratory distress syndrome (ARDS)—optimizing lung recruitment and maintenance with positive end-expiratory pressure (PEEP).
b. Limit tidal volumes to decrease the risk of alveolar overdistension.
c. Consider permissive hypercapnia (13).
d. These parameters should be followed in the operating room as well as the intensive care unit (ICU).
e. Inhaled nitric oxide has been successfully used for inhalation injury with pulmonary hypertension, but controlled outcome studies are lacking (14).
4. Heat regulation is severely disrupted after large burns.
a. The risk of hypothermia increases with younger age, greater TBSA affected, and deeper burns. Room temperature and humidity must be set to uncomfortably high levels in order to prevent heat loss.
b. Intravenous (IV) fluids must be warmed, nonoperative extremities and the head should be wrapped, and inspired gases should be actively or passively warmed and humidified.
c. After the initial acute phase, the hypermetabolic state of these patients usually produces a low-grade or moderate fever.
PATHOPHYSIOLOGY
CLINICAL PEARL In burned patients, pharmacokinetics of nearly all medications except volatile anesthetics are altered due to differences in plasma protein levels, binding, and distribution of body water.
Burns adversely affect every system in the body.
Systemic inflammatory response syndrome (SIRS) can be observed early with a burn injury, and may occur even with localized burns.
1. Increased capillary permeability and loss of microvascular integrity promote loss of intravascular fluid into the burned tissues and external environment. This results in hemoconcentration, as well as massive loss and sequestration of albumin. Albumin replacement is recommended only when the serum albumin level falls below 1.5 mg per dL (15).
2. SIRS also involves activation of tumor necrosis factor-α (TNF-α), cytokines, thromboxane, interleukins, and other inflammatory mediators causing catabolism, thrombosis, and platelet aggregation.
Burns are characterized by a hypermetabolic state that persists throughout the acute stages of injury and well into the healing phase (6,7,10,12).
1. Oxygen consumption and CO2 production increase several-fold.
2. Increased evaporation from open wounds results in heat loss, which dramatically affects resting energy expenditure. Raising the ambient room temperature by several degrees can significantly counteract this response to burn injury (10,11).
3. Protein, glucose, and fat utilization are increased due to the aforementioned humoral factors as well as hyperthermia and metabolic needs of tissue repair.
4. Adequate nutrition should be instituted within 12 hours of initial injury to address higher caloric needs.
5. Fluid and electrolyte alterations, including a profound hypoalbuminemia, hypophosphatemia, and hypermagnesemia develop within the first 24 to 48 hours.
6. A decrease in ionized calcium levels occurs. This may magnify problems with hypocalcemia in the setting of blood product transfusions and citrate intoxication.
7. Associated endocrine derangements include increased insulin resistance, hypothyroidism, and hypoparathyroidism.
The cardiovascular system experiences early and late effects.
1. Cardiac function in the first days after a burn is depressed due to circulating humoral myocardial depressant factors, hypovolemia, increased blood viscosity, and increased systemic vascular resistance.
2. By 72 hours, the cardiac output increases by two or three times the normal due to high levels of catecholamines and increased renin production. This improves blood flow to organs and tissues.
a. Hypertension and tachycardia are always present, especially in younger children.
b. At this point in the clinical course, hypotension should prompt concerns for either hypovolemia or sepsis.
The respiratory system is burdened with many insults.
1. The upper airway can sustain actual burns from the inhalation of superheated gases, which can reach 1,000°F.
2. Toxic combustibles are common products of house fires, including aldehydes (from cotton, wool, and other fibers), nitric and sulfuric acids (from NO2 and SO2), and hydrogen cyanide (from polyurethane insulation). All these produce alveolar injury and pulmonary edema.
3. Inhalation of soot and particulate matter causes mechanical obstruction of small airways. The cumulative effect is necrotizing bronchiolitis. There is loss of alveolar integrity, inflammation and edema of the bronchial mucosa, and destruction of type II pneumocytes with resulting surfactant depletion.
4. Protein leakage and pulmonary edema ensue, and vascular congestion with platelet trapping promotes pulmonary microvascular thrombosis and hypertension.
5. Pulmonary compliance decreases, bronchospasm is common, and shunt and ventilation perfusion mismatching are increased.
6. Great increases in oxygen consumption and CO2 production concomitantly increase minute ventilation requirements.
a. Ventilation of burn patients must account for the patient’s increased CO2 production and oxygen consumption.
b. If acute lung injury is present, end-tidal CO2 measurements may underestimate the true PaCO2.
c. A lung protective ventilation strategy should be used with PEEP and low tidal volume ventilation.
7. Superinfections with pneumonia are common in these patients.
8. Late complications include tracheal stenosis and contractures of the neck. These problems may require surgical release and can make airway management difficult (16).
Carbon monoxide (CO) poisoning is a common complication of inhalation injury.
1. It cannot be detected with conventional pulse oximetry. Cooximetry is used to measure carboxyhemoglobin and methemoglobin levels.
2. CO binds to hemoglobin with 200 times the avidity of oxygen, and has a dissociation half-life of up to 250 minutes. This can be reduced to 40 to 60 minutes when an FIO2 of 1.0 is provided. Therefore, high concentrations of oxygen should be administered to any child who was in a closed-space fire until CO levels are reduced.
3. CO not only reduces oxygen delivery to the tissues, but also inhibits cytochrome P-450 activity. Thereby, it interferes with oxygen utilization as well.
4. Untreated CO poisoning can also result in encephalopathy. Hyperbaric oxygen therapy may be helpful in these cases, but large surface area burns may preclude the transport of the child to a chamber.
RENAL
1. The kidneys may sustain renal tubular injury from hypoperfusion, hemoglobinuria (seen in cutaneous burns), or myoglobinuria (from electrical or very deep full-thickness burns).
a. Urine output must be maintained at a high volume.
b. Alkalinization with sodium bicarbonate, and osmotic diuresis with mannitol may help limit injury.
2. Within 72 hours of a burn, the glomerular filtration rate increases and diuresis ensues. This may be related to increases in cardiac output, or insensitivity to antidiuretic hormone and aldosterone.
3. Isosthenuria (the inability to concentrate sodium in the urine) can complicate burns >40% TBSA.
Hematologic abnormalities are common in the first 72 hours after a large surface area burn.
1. Initially, hemoconcentration occurs as the patient loses intravascular volume.
2. Thrombocytopenia develops due to platelet aggregation and trapping.
3. Disseminated intravascular coagulation and consumption coagulopathy may complicate the course.
4. After the acute phase, a thrombocytosis is common, as well as elevated levels of factors V, VII, and VIII.
5. Hemolytic anemia is worsened by humoral factors that inhibit erythropoietin.
GASTROINTESTINAL
1. The gastrointestinal mucosa suffers from acute hypoperfusion. Inflammatory mediators also make it more permeable to bacteria and endotoxins.
2. Gastric stress ulcers (Curling ulcers) may develop unless prophylaxis is instituted.
3. Ileus develops within the first 72 hours after a burn.
4. The hypermetabolic state mandates meticulous attention to nutritional needs.
a. Enteral nutrition through a gastric or jejunal feeding tube should be started as soon as possible.
b. Children with jejunal feeding tubes, if demonstrated not to reflux through the pylorus, can have these feeds continued during anesthesia for excision and grafting (6).
5. The liver also suffers from acute hypoperfusion, resulting in apoptosis and elevated aspartate transaminase (AST), alanine transaminase (ALT), and bilirubin. Later, there is hepatic enlargement with intrahepatic fat and edema.
NEUROLOGIC
1. Elevated intracranial pressure (ICP) and cerebral edema can occur in the first 24 to 72 hours.
2. Patients are at risk for burn encephalopathy with associated delirium, hallucinations, seizures, and coma.
3. Etiologies of neurologic complications include hypoxia, hypertension, hypoperfusion, sepsis, electrolyte derangements, and cortical vein thrombosis.
4. Electrical burns can result in injury to the spinal cord (6).
SURGERY
1. These patients will come to surgery frequently in the early course of treatment for excision and grafting.
2. It has been shown that early surgery and coverage with split- or full-thickness grafts, cultured skin substitutes (allograft or xenograft), or artificial grafts decreases the systemic inflammatory response, reduces infection risk, and speeds recovery (17–19).
ANESTHETIC CONSIDERATIONS
CLINICAL PEARL Even routine monitoring is affected in severely burned patients. Noninvasive blood pressure (NIBP) may be contraindicated over burned extremities, necessitating placement of arterial lines, sutured in place. Adhesive electrocardiogram (ECG) leads and pulse oximeters may similarly be contraindicated. Needle ECG electrodes and nonadhesive pulse oximeters may be needed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree