INSTRUCTIONS FOR PARENTS
HILARY A. HEWES, MD AND NANETTE C. DUDLEY, MD
DISCHARGE INSTRUCTIONS
Discharge instructions are an integral part of the emergency department experience. Well-designed instructions serve as a summary of the emergency department course and a reference for ongoing medical management by the patient and outpatient care provider. In addition, review of instructions at discharge offers a final opportunity for a patient to clarify any questions or concerns about care received or the follow-up plan. Information given to the patient and family needs to be provided in an understandable and retainable manner. Lack of comprehension of discharge instructions may lead to problems with compliance with care plan, incorrect use of medication, inadequate treatment and follow-up, and ultimately negative patient outcomes.
LEGAL AND REGULATORY CONSIDERATIONS
The Joint Commission has established standards outlining the crucial components that each hospital discharge should contain. Although obviously not specific to ED care, these recommendations can be adapted to ED discharge instruction content:
1. Reason for visit
2. Significant findings
3. Procedures and treatment provided
4. Patient’s discharge condition
5. Patient and family instructions
6. Attending physician’s name and contact information
Meaningful Use
Recently the Centers for Medicare and Medicaid Services established a financial incentive plan for the “meaningful use” of certified electronic health record technology by eligible providers and hospitals. Goals of this program are first, to improve quality, safety, efficiency and reduce health disparities; second, to engage patients and families in their health care; and third, to improve care coordination (www.healthit.gov). Eligible hospitals must meet certain required objectives each year to receive a financial incentive and avoid a payment adjustment. Well-designed discharge instructions with the information discussed below help hospitals reach the threshold for the incentive by fulfilling several possible objectives, including Core Objective 4 (maintaining an active medication list), Core Objective 12 (provide patients with an electronic copy of discharge instructions at the time of discharge), and Set Objective 7 (summary of care record for patients being transferred to another facility) (www.CMS.gov).
Legal Considerations
Discharge instructions that are well designed highlight when a patient should return for care, review potential complications associated with the patient’s diagnosis, and give clear instructions for treatments. These instructions can also serve as an important protection for emergency medicine practitioner, providing documentation that may be important when an adverse event occurs or a complaint is raised. A signature of the patient/guardian upon receipt of the instructions should be retained as part of the medical record, as should a copy of the instructions provided to the patient. This signed copy may help to serve as proof of receipt and understanding of the discharge instructions.
GENERAL PRINCIPLES OF DISCHARGE INSTRUCTIONS
Organization
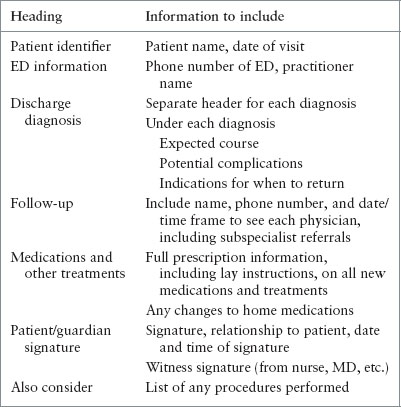
Instructions should be organized without a large amount of extra material that can distract from the critical information, and written in clear short sentences rather than paragraphs. A simplified form leads to increased patient satisfaction (Samuels-Kalow). Information should be presented with the most important items first; patients recall best the first item reviewed with them (Crane). Breaking information into separate headers with diagnosis specific instructions enhances patient recall and understanding (Table 138.1).
DISCHARGE INSTRUCTION FORMATS
The content of discharge instructions and the process by which that content is relayed to its intended audience varies widely from facility to facility. The format of the instructions can be verbal or written or may include multimedia technology. Pictures or diagrams and other visual aids may be added. Different formats have inherent strengths and weaknesses.
Verbal Instructions
Studies of discharge after hospitalization have shown that patients prefer verbal instructions from their care provider prior to discharge (Shoeb). Patients like to have a final interaction with their care provider to clarify ongoing treatment plans and to have a chance to ask remaining questions. Verbal instructions may help to overcome literacy barriers to comprehension of written instructions (Samuels-Kalow). However, verbal instructions alone are not adequate because they rely on variable communication skills of providers. Verbal instructions also rely on the patient–provider relationship, which can be challenging in the ED setting where patient care is often provided by more than one practitioner. Verbal instructions alone also do not provide any lasting documentation for the patient to reference.
TABLE 138.1
GENERAL PRINCIPALS OF DISCHARGE INSTRUCTIONS
Written Instructions
Written materials may improve recall of discharge information. A written record of the discharge instructions not only helps the patient, but also can provide valuable information to follow-up practitioners as a reference for diagnoses, care received, and changes in medications. To standardize the information provided to patients/families, many centers have moved from handwritten instructions to computer-generated or generic instructions. These preformatted instructions have the benefit of being easily legible and may be more time efficient. However, information needs to be pediatric specific and individualized (e.g., generic instructions for “chest pain” will be different for an adult vs. a child). Ideally, written instructions should have diagnosis-specific information structured under separate headings for each diagnosis. Providers can highlight the most critical information. Written instructions without verbal reinforcement are not adequate as they do not give patients and families the chance to ask clarifying questions. There is also a risk of discrepancy between reading comprehension level of the patient/family and the level of the instructions (see below). If the instructions are not written in the native language of the family they will not be well understood. In addition, written instructions often contain much superfluous information that can distract from the crucial information the provider wishes to enforce.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







