Transient Ischemic Attacks (TIA):
Link: PP & Types | S/s | W/u, Risk & Dx | Tx | Prognosis & DDx | Carotids |
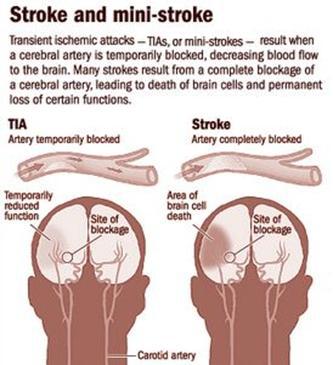 Transient neurological attacks (TNAs) are attacks with temporary (<24 hours) neurological symptoms. These symptoms can be focal, nonfocal, or a mixture of both. TIA’s are a distinct subset of TNA’s, they are also called transient sx’s with infarction (TSI) or “angina of the brain”…some suggest that patients with TIA should be considered to have unstable angina of the brain and to require urgent attention. TIA is defined as a temporary (<24 hr) focal neuro deficit due to brief interruption of local cerebral blood flow. Most last minutes to hours. TIA is a critical harbinger of impending stroke. If takes longer than 24 hr to resolve (25-72hr), then called a Reversible Ischemic Neurologic Deficit (RIND). 1/3 of full stroke pt’s have had a TIA. 60% of pt’s with a completed stroke have had premonitory TIAs. 8% with a TIA will proceed to a CVA @1mo, 11% in 90 days, 15% @1yr, 33% @5yr (Neurology 2003;60:1429-1434). In the carotid territory, usually only last 10-14min. Vertebrobasilar TIA’s last ~8min, often have a hemodynamic basis such as hypotension and cardiac arrhythmia. Paradoxically, a rapid recovery from a TIA may indicate a more unstable pathology as ischemic tissue that has recovered remains risk (NEJM 2002;347:21).
Transient neurological attacks (TNAs) are attacks with temporary (<24 hours) neurological symptoms. These symptoms can be focal, nonfocal, or a mixture of both. TIA’s are a distinct subset of TNA’s, they are also called transient sx’s with infarction (TSI) or “angina of the brain”…some suggest that patients with TIA should be considered to have unstable angina of the brain and to require urgent attention. TIA is defined as a temporary (<24 hr) focal neuro deficit due to brief interruption of local cerebral blood flow. Most last minutes to hours. TIA is a critical harbinger of impending stroke. If takes longer than 24 hr to resolve (25-72hr), then called a Reversible Ischemic Neurologic Deficit (RIND). 1/3 of full stroke pt’s have had a TIA. 60% of pt’s with a completed stroke have had premonitory TIAs. 8% with a TIA will proceed to a CVA @1mo, 11% in 90 days, 15% @1yr, 33% @5yr (Neurology 2003;60:1429-1434). In the carotid territory, usually only last 10-14min. Vertebrobasilar TIA’s last ~8min, often have a hemodynamic basis such as hypotension and cardiac arrhythmia. Paradoxically, a rapid recovery from a TIA may indicate a more unstable pathology as ischemic tissue that has recovered remains risk (NEJM 2002;347:21).
Poor Public Awareness of stroke sx’s: Almost 18% of 18,462 subjects (mean age of 65.8) with no prior dx of stroke or TIA had at least 1 stroke sx, and individuals with more stroke risk factors were more likely to have stroke sx’s (Arch Intern Med. 2006;166:1952-1958) …. The most common sx’s were sudden numbness (8.5% of the cohort), sudden weakness (5.8%), sudden loss of vision (4.6%), sudden inability of linguistic expression (3.8%), sudden loss of one half of vision (3.1%), and sudden inability to understand speech (2.7%)….. increasing the risk of reporting at least 1 sx of stroke if annual income <$25,000 and educational level < high school graduation, African Americans (1.6-fold), increased number of risk factors and those living in the “stroke belt” (SE USA).
ICD-9 = 435.9.
PP: Typically due to either low flow (large artery) or embolization (artery-to-artery, cardioaortic or unknown source) or lacunar / small penetrating vessel TIA.
Low flow TIA: usually have inadequate collateral blood supply. See brief (minutes to hours), repetitive, stereotyped spells occurring in the territory of the internal carotid artery.
Embolic TIAs: usually single and more prolonged (typically last hours) and the sx’s are related to the vascular territories involved.
4 causes of low flow & embolic TIA’s: Atherothrombotic stenotic lesions at the origin of the internal carotid artery that are narrowed >70%. Intracranial atherothrombotic disease that produces low-flow or embolic TIA due to lesions at the distal vertebral artery/vertebrobasilar junction/proximal basilar artery. Emboli to the top of the basilar artery or the middle cerebral artery stem that come from a source below, either arterial, aortic, or cardiac. Dissection lesions at the origin of the petrous portion of the internal carotid artery or at the C1-2 level of the vertebral artery as it enters the foramen transversarium.
Lacunar/small vessel TIA: usually is due to lipohyalinosis from HTN, but also may arise because of atheromatous disease at their origin. See face, arm, and leg weakness or numbness.
Crescendo TIA’s: are >2 attacks in 24hr, a medical emergency.
Subclavian steal syndrome: stenosis of the L subclavian proximal to the origin of the vertebral artery leads to cerebral/ cerebellar sx’s during exertion and are accompanied by L arm claudication.
Carotid Circulation: atheroma or emboli.
Post cerebral circulation: atheroma, cervical osteophyte or osteoarthritis compressing the artery.
Vs TSI: Analysis of 87 pt’s indicates that transient sx’s associated with infarction (TSI) appears to be the most unstable phenotype of TIA, at it is associated with the greatest risk for imminent stroke (Ann Neurol 2005;57:679-86) (infarcts were significantly smaller, on average, in TSI pt’s than in ischemic-stroke pt’s, but no particular lesion-size threshold distinguished the two).
TNA’s: Sudden attacks of neurologic dysfunction that do not qualify as TIA’s (one not attributable to the dysfunction of a single arterial territory of the brain) according a 10- year study with 6000 subjects aged 55 or older (JAMA. 2007;298(24):2877-2885)…all had roughly similar clinical courses……Relative to those subjects without any neurologic attacks, the hazard ratio for subsequent stroke among those with TIAs was 2.14; among those with nonfocal attacks, the HR was 1.56; and among those with attacks showing both focal and nonfocal characteristics, the HR was 2.48 (but these patients were rare).
S/s: Last <10min in 90%. Sx’s can be of almost any stroke syndrome including numbness with or w/o weakness of hand, face or legs. Paralysis, even upside-down vision. Sudden trouble walking, dizziness or loss of balance or coordination. Sudden confusion, trouble speaking (aphasia, slurred speech) or understanding. Sudden severe H-A with no known cause.
Transient Monocular Blindness (amaurosis fugax): from ischemia in the territory of the central retinal artery (a small embolus to the ophthalmic artery). Presents with blurring or darkening of the vision (“a curtain had descended”) that peaks in seconds. May see embolic particles (Hollenhorst plaques) in the retinal artery branches. Confers a lower risk of subsequent stroke than hemispheric TIA, thus CEA only beneficial in high-risk pt’s (NEJM 2001;345:1084).
Important Historical Points: Date of first spell and number of attacks. Frequency of attacks. Duration of attacks. Specific body parts and functions involved. Any associated difficulty with speech, vision, swallowing, etc. Other associated symptoms (chest pain, shortness of breath, nausea and vomiting, headache). Any history of hypertension, diabetes mellitus, hypercholesterolemia, coronary artery disease, peripheral vascular disease, drug abuse. Any past episodes suggestive of retinal, hemispheric, or vertebrobasilar TIA. Current medications especially aspirin, oral contraceptives, antihypertensives.
Other Affected Areas:
Cranial nerves: visual loss in one or both eyes. Bilateral loss may indicate more ominous onset of brainstem ischemia. Double vision, if double vision is subtle, the pt may describe it as “blurry” vision.
Vestibular dysfunction: true vertigo is likely to be described as a spinning sensation rather than nonspecific lightheadedness.
Difficulty swallowing: may indicate brainstem involvement; if the swallowing problem is severe, there may be an increased risk of aspiration.
Motor function: unilateral or bilateral weakness affecting the face, arm, or leg Bilateral signs may indicate more ominous onset of brainstem ischemia.
Sensory function: unilateral or bilateral: either decreased sensation (numbness) or increased sensation (tingling, pain) in the face, arm, leg, or trunk. If sensory dysfunction occurs without other s/s, the prognosis may be more benign, but recurrence is high.
Speech and language: slurring of words or reduced verbal output; language difficulty pronouncing, comprehending, or “finding” words If speech is severely slurred or facial drooling is excessive, there is an increased risk of aspiration. Writing and reading also may be impaired.
Coordination: clumsy arms, legs, or trunk; loss of balance or falling (particularly to one side) with standing or walking Incoordination of limbs, trunk, or gait may indicate cerebellar or brainstem ischemia.
Psychiatric or cognitive function: apathy or inappropriate behavior These sx’s can indicate frontal lobe involvement and frequently are misinterpreted as poor volitional cooperation.
Excessive somnolence: this sx may indicate bilateral hemispheric or brainstem involvement.
Agitation or psychosis: rarely, these sx’s may indicate brainstem ischemia, particularly if they occur in association with CN or motor dysfunction.
Confusion or memory changes: these rarely are isolated sx’s; more frequently, they are associated with language, motor, sensory, or visual changes. Inattention to surrounding environment, particularly to one side; if severe, pt may deny deficit or even his or her own body parts. Depending on the severity of neglect, the physician may need to lift the pt’s arm to check for strength, rather than rely on the pt to perform this task. It could be argued further that these TIAs are not transient at all because if your cognitive functioning is impaired and your quality of life is impaired, some people would argue that that is symptomatic (Stroke. Published online August 2, 2007).
W/u: Similar to a stroke, but the workup is not necessarily urgent and can often be done as an outpatient if resolved. The pt needs to be aware that the highest risk period is soon after the TIA and that the w/u needs to be completed quickly.
Step #1: CBC, lytes, LFT’s, glucose, cholesterol, HDL/ LDL, ESR, RPR, PTT/PT, ECG, Carotid duplex U/S study, non-contrast cranial CT or MRI (Imaging Studies). Holter monitor (r/o A-fib). See stroke Initial Eval |
2nd Line tests: Used to resolve any diagnostic uncertainty as appropriate. Transthoracic/esophageal echo, transcranial Doppler, MRA, cerebral angiography, prothrombic w/u (homocysteine, C-reactive protein, anticardiolipin antibody, factor 5 Leiden), ambulatory ECG, LP (if possible SAH is suspected). Testing for silent myocardial ischemia with an exercise stress test or thallium perfusion.
***If ongoing sx’s need expedited evaluation: no reliable way to determine if the abrupt onset of neurologic deficits represents reversible ischemia without subsequent brain damage or if ischemia will result in permanent damage to the brain (stroke). Pt’s with TIA who were worked up in the ED observation unit had shorter stays (25.6 vs. 61.2 hours), lower costs (US$890 vs. $1547), and comparable outcomes to those who were worked up in the hospital (Ann Emerg Med 2007;50:109-19).
Indications for Inpatient Evaluation of Possible TIA or Stroke:
High-risk cardioembolic source: acute myocardial infarction (especially if large and significant wall-motion abnormality is present), mural thrombi, new-onset atrial fibrillation Consider anticoagulation.
TIAs manifested by major sx’s: such as dense paralysis or severe language d/o Possible evolving large hemispheric stroke with increased risk of brain swelling.
Increasing frequency or severity of TIAs (crescendo pattern): Possible evolving thromboembolic stroke.
Evidence of high-grade carotid artery stenosis: Carotid artery evaluation for possible emergency intervention (surgery, stent, or angioplasty).
Drooling, imbalance, decreased alertness, difficulty swallowing: Increased risk of falling, or of aspiration and other pulmonary complications.
Severe H-A, photophobia, stiff neck, recent syncope: Possible subarachnoid hemorrhage: obtain emergency CT scan of the head; if the scan is negative but clinical suspicion remains high, CSF evaluation or possible cerebral angiography is needed.
The 7-point ABCD2 Score to Risk Stratify TIA:
ABCD2 a prognostic tool for predicting the early risk (7 day) of stroke after TIA that may help physicians determine which pt’s need emergency care (Lancet 2007; 369:283-92). Score is based on age, blood pressure, clinical features, diabetes, and TIA duration.
2pt’s for TIA duration of >60,
2pt’s for unilateral weakness,
1pt for age >60,
1pt for SBP >140 mmHg systolic or >90 mmHg diastolic,
1pt for speech impairment without weakness,
1pt for TIA duration 10 to 59 minutes, and
1pt for diabetes.
~21% of pt’s are classified as high risk (6-7 points, 8.1% 2-day risk), 45% moderate risk (4-5 points, 4.1% 2-day risk), and 34% low risk (0-3 points, 1% 2-day risk). An ABCD2 score of >4 may justify 24-hour hospitalization in the U.S. solely on the basis of a greater opportunity to administer thrombolysis early if a subsequent stroke occurs in the hospital as opposed to at home.
6-point ABCD Score: Age: 60 = 1 point. BP at presentation: SBP >140 mm Hg or DBP >90 = 1 point.
Clinical features: unilateral weakness = 2 points, speech disturbance without weakness = 1 point.
Duration of sx’s: 60 minutes = 2 points, 10–59 minutes = 1 point, <10 minutes = 0 points. The 7–day risk for stroke was 0%, 2%, 16%, and 36% among 209 pt’s with scores of <4, 4, 5, and 6, respectively (Lancet 2005;366:29-36). Those with a score >4, consider emergency tx or hospitalization.
• The predictive ability of a 6-point score based on age, blood pressure, clinical features and duration (ABCD) is improved by the addition of CT imaging in identifying patients with a high stroke risk after a TIA (Stroke 2008;39:297-302)…..They found that 10 (3.6%) patients had a stroke within 10 days and 15 (5.5%) had one within 30 days.
• For every point of the ABCD score, the odds ratio for a stroke increased by 2.55 at 7 days and 2.62 at 30 days. Outcomes after TIA were comparable for people managed as outpatients and those managed as inpatients, after triage with the ABCD2 risk-stratification score (Stroke 2011;42:1839)……hospitalization (for patients with ABCD2 scores of 6–7 or ABCD2 scores of 4–5 with significant vascular stenosis) or discharge for follow-up at an outpatient TIA clinic (ABCD2 score of 0–3 or ABCD2 score of 4–5 without significant vascular stenosis).
Dx: There really is no ‘gold standard’ for diagnosing TIA. Sixty of 100 consecutive TIA diagnoses made in a major urban medical center’s emergency department were judged to be wrong after a neurologist reviewed the patients’ medical records and test results (AAN meeting 2008; Abstract S4)…..the 60 misdiagnosed patients actually had: Migraine with aura (14 cases). Toxic-metabolic effects related to drugs, infections, glycemic abnormalities, or hypertensive encephalopathy (14). Atypical partial seizure (13). Compressive neuropathy (8). Psychiatric disorder (7). Unclassifiable (4)…..In 38.3% of the cases judged to be misdiagnosed, symptom onset was gradual. Only 10% of the correctly diagnosed TIA cases involved gradual onset (P=0.007)…..the presence of non-specific symptoms and a history of prior unexplained focal neurological episodes — which are unusual in genuine TIA (1%).
Tx of TIA: See Links: PV & Long-term Tx | Antiplatelet | Prognosis & DDx | Always start with as needed supportive tx with O2, glucose, control fever, keep SBP <160, DBP <90, hydrate. Determine the pathophysiology of the TIA so that specific stroke preventive therapy can be prescribed.
Can treat as outpatient if low risk (current episode prior to 2wks, small neuro deficit, infrequent events, monocular vision loss). Manage cardiovascular risk factors.
Rapid assessment and tx protocol of a first TIA or minor ischemic stroke dramatically reduces risk for subsequent major stroke by about 80% (Lancet and Lancet Neurol 2007;online October 9)…..The protocol included a 300-mg loading dose and subsequent 75-mg daily dose of aspirin combined with a 300-mg loading dose followed by a 75-mg daily dose of clopidogrel for 30 days….High-risk individuals were also prescribed 40 mg/day of simvastatin to treat elevated cholesterol, as well as antihypertensive medication when indicated. In addition, anticoagulation therapy and carotid endarterectomy was administered as required…..”possible new standard for tx of TIA as at 90 days, the stroke rate was 1.24%, compared with an expected rate of 5.96%”.
Hospitalize if high risk (current episode within 2wks, frequent events, large neuro deficit). Start secondary prevention as with acute stroke. TIA pt’s should definitely not receive thrombolytic therapy, but should receive antithrombotics if high risk. Hospitalization if appropriate imaging studies, including evaluation of the cerebral vasculature, are not immediately available.
If ischemic: Start ASA 81-325mg/d. If unable to use ASA use Clopidogrel (Plavix) 75mg/d (an ADP blocker). If recurrent sx’s on ASA use Aggrenox (ASA + Dipyridamole) BID or Clopidogrel. Start statin & risk factor therapy. Early, aggressive tx (clopidogrel 300-mg loading dose and subsequent 75-mg qd + ASA 75mg x 30 days + 40 mg/day of simvastatin and anti-HNT med if indicated) of pt’s who have suffered a first TIA or minor ischemic stroke significantly reduces the risk of recurrent stroke by >90% (16th European Stroke Conference: EXPRESS Trial: June 1, 2007).
If cardioembolic: Multiple stroke sites, +AF/ mitral stenosis/ mechanical valve/ recent AMI/ LV aneurysm or patent foramen ovale, start IV/SQ Heparin / Warfarin as generally low risk of brain hemorrhage. Also start a statin & CV risk factor therapy. Stroke pt’s with a PFO and ASD are at incr risk of recurrence, but not with either one alone (NEJM 2001;345:1740). Links: Carotids |
Prognosis & Ddx: 10-12% have s subsequent stroke/ TIA in the 90-day period after the event, 50% of these occur in the first 2 days. Many TIA pt’s, especially those with prolonged sx’s (>30min) or aphasia have detectable brain injury on diffusion-weighted imaging (Neurology 2004;62:376-80).
• Risk for stroke after TIA or minor stroke Is substantial (BMJ 2004;328:326-8), estimated cumulative stroke risks for TIA pt’s is 8% at 7 days, 11.5% at 1 month, and 17.3% at 3 mo’s. For minor-stroke pt’s, estimated cumulative risks are 11.5%, 15%, and 18.5%.
• The 90-day rate of stroke recurrence in 1085 patients referred to the TIA clinic decreased from 10.3% during April 2002 through September 2004 to 2.1% during October 2004 through March 2007 (reduced by 79%)(Lancet 2007;370:1432)….Based on evaluation, testing was ordered and antithrombotic therapy was instituted before discharge……Urgent evaluation of TIA is often best performed during hospitalization, but these studies suggest that immediate access to a TIA clinic staffed by vascular neurologists to diagnose TIA, initiate appropriate evaluation, and begin treatment may be a reasonable alternative.
• TIA carries a “not so benign” prognosis, they have about a 50% complication rate as strokes (Stroke 2004;35:2453-2458)……during a hospital stay, 8% of TIA pt’s had pneumonia or UTI (Vs 19% of stroke pt’), 2% had a cardiovascular event (vs 4% of stroke pt’s), and 8% had a subsequent stroke during their hospital stay.
• TIAs typically occur just hours or days before a stroke, leaving a small window for preventive efforts (Neurology 2005;64:817-820) (17% of TIAs occurred on the day of the stroke, 9% on the previous day, and 43% at some time during the preceding week). Within 3 mo’s of a TIA >14% of people experience a stroke (Stroke 2005;36:720-724).
• In a prospective study, 15% of patients had not recovered full functioning 3 months after transient ischemic attack or minor ischemic stroke (Stroke 2012:Sep 13;e-pub ahead of print).
• Pt’s who experience a TIA are at a substantially increased risk of having a major stroke within 1 week according to a large systematic review (Lancet Neurol; published online November 12, 2007)…the risk for major stroke following TIA is 5.2% at 7 days and 3.2% at 2 days. — a finding that, researchers say, warrants treating TIA as a medical emergency.
• More than 15% of patients can be expected to have a stroke within 90 days of TIA presentation according to a meta-analysis of 11 studies (Arch Intern Med 2007;167:2417). An analysis from the EXPRESS trial, which showed that urgent aggressive intervention after a TIA or minor stroke cut the 90-day risk for recurrent stroke by 80% (2% vs. 8%), now confirms this strategy reduces fatal and nonfatal stroke as well as disability, hospital admission days, and costs by the same magnitude (Lancet Neurol. 2009;Published online February 5)…..After a TIA or minor stroke, the risk for recurrent stroke within 7 days is between 8% and 10%…..The incidence of fatal or disabling stroke at 6-month follow-up was significantly lower in the second phase than in the first phase (0.3% vs. 5.1%).
• Risk for stroke within 24 hours after TIA was 5% in a large population-based study in the UK on 488 patients with first TIAs from 2002 to 2007 (Neurology 2009;72:1941)…..the risk for stroke was 1.2% within 6 hours, 2% within 12 hours, and 5.1% within 24 hours……Of the 59 strokes that occurred within 30 days after TIA, 25 (42%) occurred within the first 24 hours. ….Nineteen of the 25 patients who had strokes within 24 hours had ABCD2 scores 5……Risk for stroke within 24 hours after TIA was 2.0% in patients with ABCD2 scores 4, 6.5% with scores of 5, 11.8% with scores of 6, and 33.0% with scores of 7. …..Although stroke risk correlates with the ABCD2 score, even patients in the lowest risk ABCD2 group have a 2% risk for stroke within 24 hours, which is sufficient to warrant emergent evaluation.
• A population-based study shows that TIA precedes an acute stroke in only 12.4% of cases, ranging up to about 20% for large artery strokes according to data on 16,409 consecutive patients (Neurology. 2009;73:1074–1076)…..urgent diagnosis and treatment clinics for TIA may only prevent a relatively small percentage of stroke overall…..we might prevent only 80% of 12.4% of strokes, assuming we could diagnose and treat these patients very soon after a TIA has occurred.”
• Suffering a TIA reduces 1-year survival by almost 4%, and 9-year survival by 20%, with a relatively poorer outcome among those older than 65 years (Stroke. Published online November 10, 2011).
• A substantial proportion of patients (15%) with TIA or minor stroke (NIH Stroke Scale score <4) become disabled after the event a study on 499 patients shows (Stroke. Published online September 13, 2012)…..None of the poor outcomes were associated with complications from carotid revascularization or anticoagulation….Of the patients with a disabled outcome at 90 days, 55 (74%) had no recurrent stroke, whereas 19 (26%) had a recurrent event (symptom progression in 9 and recurrent stroke in 10).
The “ABCD” rule for predicting stroke following a first TIA can be used by emergency physicians to decide which patients may be candidates for discharge home if followed with urgent outpatient evaluation (Ann Emerg Med 2009;53:662-673)…..Risk factors included in the ABCD rule were age 60 years or older, elevated blood pressure, unilateral weakness, speech impairment without unilateral weakness, and symptom duration, for a total of 6 possible points. …..ABCD scores of less than 4 indicated the risk of stroke was reliably less than 2% at days 2 and 7, the authors report. At scores of 4 or higher, the risk of stroke increased to 5.4% at 2 days and ranged from 6.3% to 13.2% at 7 days.
• Risk for stroke within 24 hours after TIA was 5% in a large population-based study with 488 patients (Neurology 2009;72:1941-47)…..the risk for stroke was 1.2% within 6 hours, 2% within 12 hours, and 5.1% within 24 hours…..Of the 59 strokes that occurred within 30 days after TIA, 25 (42%) occurred within the first 24 hours……….The 7-point ABCD2 score predicted 24-hour recurrence well — risk ranged from 2% among patients with scores of 4 or lower to 33% for those with scores of 7.
Non-Focal TIA’s: disturbances of consciousness [syncope, acute confusion, or transient global amnesia], amnesia, unsteadiness, or dizziness. Prognosis of nonfocal TIA is nearly the same with nonfocal as with focal transient attacks (hemiparesis, dysarthria, or amaurosis fugax) according to a population-based cohort study with 6,000 pt’s (JAMA 2007;298:2877)….both are associated with high risk for stroke (~10% in the subsequent 3 months)…..Patients with nonfocal attacks were also at greater risk for developing dementia (HR, 1.59), and those with mixed attacks (a combination of focal and nonfocal) were at greater risk for developing ischemic heart disease (HR, 2.26), vascular death (HR, 2.54), and dementia (HR, 3.46).
Ddx: complicated migraine, arrhythmia, sz (Todd’s paralysis), hypoglycemia, subdural bleed, neurosis, and tumors (especially with acute hemorrhage).
Neurologists are proposing 3 clinical features to help clinicians diagnose difficult-to-assess TIAs from nonischemic causes: (Cerebrovasc Dis. 2008;Published online November 4).
3 clinical characteristics independently associated with a final diagnosis of a nonischemic transient neurologic attack:
1 Gradual symptom onset (OR 6.7). Speed of onset was the strongest indicator of a TIA, ask the patient if their symptoms came on like lightning — within as other neurological problems that can mimic a TIA — migraines or seizures symptoms take more than a minute to manifest.
2 History of unexplained transient neurologic attacks (OR 10.6).
3 Presence of nonspecific symptoms (OR 4.2).
• Previous research has found that transient visual and sensory symptoms are less associated with TIA and subsequent stroke. Nonspecific neurologic complaints, such as cognitive impairment, are also less common in TIA. However, physical findings such as carotid bruit are suggestive of TIA.
**Ref: (Tx of acute ischemic stroke (Ann Emerg Med 2001;37:202-16) ( Hypertension and stroke. Ann EM 1999;34:244-55) (J Gen IM 1998;13) (Arch IM 1994;120:633-7) (Am Fam Phys 2000;61:2) (EM Clin NA 1996;14:1) (Prevention of stroke, JAMA 1998;281:1112-20) (Prevention, Am Fam Phys 1999;60:8) (SAH, NEJM 2000;342:1) (Prevention of stroke, NEJM 1995;333:21) (Acute stroke. Emerg Med Clin North Am 1996;14:197-216) (Tx of acute ischemic stroke. NEJM 2000;343:10) (Merritt’s Textbook of Neurology, 10th ed., 2000, Williams & Wilkins) (LP in SAH, Ann Emerg Med 1998;32) (Spontaneous intracerebral hemorrhage. NEJM 2001;344:19) (Guidelines for prevention of stroke in pt’s with ischemic stroke or transient ischemic attack. Stroke 2006;37:577-617)
Links: Definitions | Minor injury, Eval & CT scan Indications | Concussion (Mild Traumatic Brain Injury = TBI) | Major | GCS | Spinal Cord Injury |
Traumatic Brain Injury (TBI): results in disturbance or LOC (= concussion).
Closed Head Injury (CHI): results from disruption of reticular activating system by a torsional movement of cerebrum about the midbrain. CHI has a 5% risk of Post Traumatic Epilepsy (PTE) with 80% of first sz within 2 yrs. Higher incidence of PTE with hematomas and retained ferric fragments, larger lesions/contusions and frontal-temporal lesions, penetrating injury’s having 50% risk of PTE. If the clinical exam indicates a strong possibility of CNS injury, obtain a neurosurgery consultation rapidly. If there is blood behind the tympanic membrane (hemotympanum), CSF otorrhea, or CSF rhinorrhea, assume skull fx regardless of radiographic findings.
Concussion: brief loss of consciousness (LOC, <6hr) with no parenchymal abnormalities on CT. Usually traumatically induced.
Cerebral Contusion: (hemorrhagic contusion), direct injury to the brain itself. See high density areas on CT (“salt and pepper”), usually with much less mass affect for their apparent size. May enlarge or coalesce with time. Occur in areas where sudden deceleration causes brain to impact a bony prominence (tempora, frontal, occipital poles).
Contrecoup Injury: (counter blow), force imparted to the head causes the brain to compress against the skull in area opposite the blow, resulting in contusion.
Uncal herniation: blown ipsilateral pupil (1st warning sign), contralateral then ipsilateral hemiplegia. Declining mental status. Tachypnea and decerebrate (extension) posturing
Central herniation: behavioral mental status changes. Frequent sighs or yawns, +/- Cheyne-Stokes respiration. Miotic reactive pupils, +/- roving eye movement progressing to bilateral blown pupils. Extremity rigidity then decorticate (flexion) then decerebrate posturing.
Posterior fossa herniation: coma, bradycardia, respiratory arrest.
Diffuse Axonal Injury: a primary lesion of rotational acceleration/ deceleration head injury. Due to stretching & tearing of the axons secondary to trauma. Thought to be responsible for post-concussive syndrome. Often causes hemorrhagic foci in corpus callosum and dorsolateral rostral brainstem, with microscopic evidence of diffuse injury to axons. (retraction balls, scarring, degeneration). Pt is often immediately rendered comatose.
ICD-9 Codes:
850.0 With no loss of consciousness
850.1 With brief loss of consciousness
850.2 With moderate loss of consciousness (1-24 hours)
850.9 Concussion, unspecified
• Risk for TBI increases with the presence of mental disorders (odds ratio, 1.94), age 70 or older (compared with age 30–39: OR, 1.87), living in more rural than urban areas (OR, 1.38), and low income (OR, 1.92) according to data on 16,635 patients (J Neurol Neurosurg Psychiatry 2012 Jul 8;e-pub ahead of print)…..Medical conditions associated with elevated TBI risk were hypertension, diabetes, stroke, epilepsy, and renal dialysis. Psychiatric disorders associated with the highest TBI risk included nonpsychotic disorders due to brain damage (OR, 8.32) and disorders arising from alcohol or substance use (OR, 4.40). After adjustment for demographics, TBI risk was greater with more pre-TBI psychiatric outpatient visits, prescriptions, and hospital care. We need to evaluate psychiatric patients and educate them regarding the risks for TBI, whether associated with substance use, sedative effects of medications, careless use of cellular phones, nonuse of helmets, etc. Our sickest patients are at the highest risk for a possibly preventable disorder.
Step #1: Evaluate airway & breathing per ATLS guidelines. Immobilize the cervical spine. Note any crepitus, step off (abnormal contours) when palpating the spinous processes. Note any soft tissue injury. Look for tracheal deviation or JVD. Listen to lungs and heart.
Step #2: Exam Findings | Indications for CT scan | Concussion Eval | Major | GCS |
Look for: Raccoon eyes = periorbital ecchymosis (basilar skull fx).
Battle’s sign = discoloration in the line of the posterior auricular artery, with ecchymosis first appearing near the tip of the mastoid process (basilar skull fx).
Perform funduscopic to look for hemorrhage & venous pulsations), inspect eyelids.
Eye mov’t: if none then bilateral pontine lesion. If Dysconjugate gaze then brainstem lesion. If horizontal conjugate gaze then unilateral pontine or frontal lobe lesion.
Neuro: Level of consciousness:
Awake = aroused and aware.
Lethargic/ somnolent = diminished arousal, but can be maintained with repeated light stimuli.
Stupor = severely impaired arousal with vigorous stimulation.
Confusion = impaired attention, but able to follow commands.
Delirium = intermittent confusion with agitation.
Coma = total or near unresponsiveness.
Grade: Mild –> <30min LOC & posttraumatic amnesia, no skull fx.
Moderate –> 1-24hr, skull fx.
Severe –> >24hr, brain contusion, intracranial hematoma.
Sonographic measurement of mean binocular optic nerve sheath diameter (if >5 mm) accurately detects increased intracranial pressure in adult pt’s after head injury (Ann Emerg Med 2007;49:508-514)…..Bedside ultrasonography has a sensitivity of 84% and the specificity was 73% vs 25% sensitivity via clinical assessment in this study with 59 pt’s.
Indications for CT:
Canadian Head CT Rule: Head CT required only in pt’s with minor head injuries (witnessed LOC or disorientation with GCS 13-15).
Rule: A CT scan is done if one or more medium and high risk factors are present:
High risk for neurosurgical intervention: GCS <15 2hr after injury, suspected open/ depressed skull fx, any sign of basal skull fx (hemotympanum, raccoon eyes, CSF otorrhea, Battles sign), >2 episodes of vomiting, age >65yo.
Medium risk: amnesia for events before impact >30min, dangerous mechanism (fall >3ft, fall >5 steps, ejected from motor vehicle, pedestrian hit by motor vehicle).
• Using both high and medium risk criteria to detect clinically important brain injury: sensitivity 98.4%, specificity 49.6%, proportion of pt’s with CT ordered 54.3%. Using the high risk criteria to identifying pt’s requiring neurological intervention: sensitivity 100%, specificity 68.7%, proportion of pt’s with CT ordered 32.2%. (Lancet 2001;357:1394).
• The Canadian CT head rule has higher specificity for important clinical outcomes than does the New Orleans criteria and its use may result in reduced imaging rates (JAMA 2005;294:1511-18).
• The Canadian CT Head Rule was found to be superior to New Orleans Criteria in minor head injury (Acad Emerg Med 2012;19:2)….Both rules were 100% sensitive for identifying patients with each of these three outcomes, but the Canadian CT Head Rule had significantly higher specificity than the New Orleans Criteria (36% vs. 10%, 35% vs. 10%, and 81% vs. 10%, respectively).
New Orleans Criteria for Determining if CT Is Indicated After Minor Head Injury:
CT is needed if the pt meets one or more of the following criteria: Headache. Vomiting. Age older than 60 years. Drug or alcohol intoxication. Persistent anterograde amnesia (deficits in short-term memory). Visible trauma above the clavicle. Seizure.
• Applicable for adults with a normal GCS of 15 and blunt head trauma that occurred within the previous 24 hours that caused loss of consciousness, definite amnesia, or witnessed disorientation (NEJM 2000;343:100-5).
• Neuro exam is an unreliable predictor of intracranial injury in pt’s with a seizur disorder, CT scan should be routine with any head trauma regardless of prior history (Arch Surg 2005;140:858-64).
• For children <2 years of age, the benefit of computed tomography outweighs the risk of malignancy (radiation) only for those at highest risk for brain injury (J Pediatr 2012:Aug 24;e-pub ahead of print)….high risk for clinically important traumatic brain injuries (ciTBI, defined as head injury resulting in death or requiring neurosurgery, endotracheal intubation for >24 hours, or hospital admission for =2 nights) includes a GCS score of 14, other signs of altered mental status, or palpable skull fracture.
Decision rules for computed tomography in head injury in adults
(Appropriateness Criteria for head trauma. National Guideline Clearinghouse 2012, Nov 5)
•American College of Emergency Physicians (ACEP) clinical policy for adults e 16 years old with mild traumatic brain injury (Glasgow Coma Scale [GCS] score 14 or 15)
o if loss of consciousness or posttraumatic amnesia, noncontrast head computed tomography (CT) indicated only if 1 or more of (ACEP Level A)
§ headache, vomiting, age > 60 years old, drug or alcohol intoxication, short-term memory deficit, signs of trauma above clavicle, posttraumatic seizure, GCS score < 15, focal neurologic deficit or coagulopathy.
o if no loss of consciousness or posttraumatic amnesia, noncontrast head CT may be considered only if any of (ACEP Level B)
§ focal neurologic deficit, severe headache, vomiting, age > 65 years old, signs of basilar skull fracture, GCS score < 15, coagulopathy, dangerous mechanism of injury, including, ejection from motor vehicle, pedestrian struck by vehicle or fall from > 3 feet (1 meter) or 5 stairs.
o skull film x-rays not recommended for mild traumatic brain injury (ACEP Level B)
patients with isolated mild traumatic brain injury who have negative head CT may be safely discharged from emergency department (ACEP Level B)
PECARN head injury prediction rule: From the Pediatric Emergency Care Applied Research Network (PECARN) database.
Severe Injury Mechanism is defined as a motor vehicle collision with patient ejection, death of another passenger, or rollover; pedestrian or bicyclist without helmet struck by motor vehicle; falls (>3 feet for children younger than 2 years, >5 feet for children aged 2 years or older); or head struck with a high-impact object. Of 42,099 patients (median age, 5.7 years), 367 (0.9%) had clinically important TBI, a severe injury mechanism was documented in 5869 patients (14%) and was an isolated finding (only one of the 6 risk factors) in 3302 patients (8%) (Arch Pediatr Adolesc Med 2012;166:356)…of those with isolated injury, 0.3% of those aged younger than 2 years and 0.6% of those aged 2 years or older had clinically important TBI.
Other Possible Indications: GCS 13-14, LOC, intoxication with ETOH or drug, Auto Vs auto, Auto Vs pedestrian, Auto Vs bicycle. Other impressive source of injury, evidence of skull fx, Age <2 or >60, abnormal neuro exam, H-A & emesis, current anticoagulation therapy, post injury sz, short-term memory deficit, physical evidence of trauma above the clavicles.(NEJM 2000;343:100).
GCS <13 or deficit get CT (Routine CT not needed in pt with h/o LOC or amnesia w/o s/s depressed skull fx or abn MSE (Ann Em Med 1996:27)….No routine CT if h/o LOC or amnesia without S/S of depressed skull fx and nl MSE.
• The risk and benefits of CT scans in minor head trauma in children needs re-evaluating (BMJ 2004;328:19-21), as even low doses of ionizing radiation administered to the brain prior to the age of 18 mo’s (at dose levels overlapping those imparted by CT can) appear to adversely affect long-term intellectual development according to a Swedish study.
• Clinical prediction rules could help physicians determine when a child >2yo with blunt head trauma does not need a CT scan (if non-severe injury mechanism, no signs of basilar skull fracture, and no severe headache) according to data on more than 42,000 children presenting to emergency departments with seemingly minor head trauma (Lancet 2009;Early Online Publication, 15 September)……In the validation population, the prediction rule for children younger than 2 years (normal mental status, no scalp hematoma except frontal, no loss of consciousness or loss of consciousness for less than 5 sec, non-severe injury mechanism, no palpable skull fracture, and acting normally according to the parents) had a NPV for ciTBI of 100% and sensitivity of 100%.
CATCH rule: A decision rule can identify children with minor head injury who need to undergo CT, thereby reducing the number of scans and saving children from unnecessary exposure to ionizing radiation (CMAJ. Published online February 8, 2010).
This rule states that CT of the head is required only for children with minor head injury and any one of the following findings, which they divided into high risk, meaning the need for neurologic intervention, and medium risk, meaning brain injury on CT scan.
High risk: 1. Failure to reach a score of 15 on the Glasgow Coma Scale within 2 hours. 2. Suspected open or depressed skull fracture. 3. History of worsening headache. 4. Irritability on examination.
Medium risk: 1. Any sign of basal skull fracture. 2. Large, boggy hematoma of the scalp. 3. Dangerous mechanism of injury (eg, motor vehicle crash, fall from elevation > 3 feet [91 cm] or 5 stairs, fall from bicycle with no helmet)
• The high-risk factors were 100.0% sensitive (95% confidence interval [CI], 86.2% – 100.0%) for predicting the need for neurologic intervention and would require that 30.2% of patients undergo CT.
• The medium-risk factors were 98.1% sensitive (95% CI, 94.6% – 99.4%) for the prediction of brain injury by CT and would require that 52.0% of patients undergo CT, the study authors report.
Normal CT:
Admit –> intoxicated, no competent observer at home, intractable N/V/ progressive sx’s, abnormal neuro exam.
Instructions to Return –> alteration in gait/ eyesight/ MS/ behavior, vomiting, unequal pupil size, worsening H-A, any other inexplicable abnormality.
Head injury: awaken pt q 1-2hr and touch parent fingertip or follow simple commands for 24hr.
Post Head Injury Advice: Time is needed to heal. Reduce your responsibilities. Expect poor concentration (70%), irritable/ fatigue/ depression (63%), memory problems/ H-A/ anxiety (59%), dizziness, diplopia and photosensitivity. A study advocates for routine follow-up CT in 20yo patients with mild traumatic brain injury and abnormal CT scans who do not require surgery as cost effective (J Trauma 2008;65:66)(but not in the aged 40, 60, and 80yo groups)(based on the incidence of delayed hematoma, and the probability that hematoma surgery could be performed before deterioration led to coma).
Elderly: Elderly pt’s with blunt head trauma are at higher risk for significant intracranial injuries, which in turn are more likely to have an occult presentation (Acad Emerg Med 2006;13:302-7)……elderly pt’s injuries were more likely to have an occult presentation, defined as normal level of consciousness, no neurologic deficit, and no evidence of open, depressed, basilar, or diastatic skull fx (26.1% vs. 1.5%). When symptomatic, elderly pt’s were less likely to have nausea, vomiting, and H-A.
Link: Definitions, PP, ICD9 | Evaluation, S/s & Tx | Grade & Returning to Play (Sports and Recreation) | Post Concusion Syndrome & Recovery Stages |
But to ensure that concussions are fully taken care of, athletes, parents and coaches first need to spot the symptoms. Many parents and coaches mistakenly believe concussions always involve loss of consciousness.
• The incidence of traumatic brain injury (TBI) uncovered by a study in New Zealand is much higher than some previous estimates (Lancet Neurol. Published online November 22, 2012)……The vast majority (95%) had mild TBI, with the risk of sustaining mild TBI more than 18 times greater than that for moderate or severe TBI. About a third of the patients (36%) didn’t present to hospitals at the acute stage of TBI. Falls (which accounted for 38% of TBIs), assaults (17%), exposure to mechanical forces, and transport accidents were the most common cause of TBI. The study found a greater than expected proportion of TBI in children and younger adults — they represented almost 70% of all TBI cases as opposed to the 40% to 60% reported elsewhere.
Consensus from the International Conference for Concussion: (J Sci Med Sport 2009;12:340-351)
1. Concussion may be caused either by a direct blow to the head, face, neck, or elsewhere on the body with an impulsive or rotational force transmitted to the head.
2. Concussion typically results in the rapid onset of short-lived impairment of neurologic function that resolves spontaneously.
3. Concussion may result in neuropathologic changes, but the acute clinical symptoms rarely reflect a functional disturbance rather than structural injury.
4. Concussion results in a graded set of clinical syndromes that may or may not involve loss of consciousness; resolution of the clinical and cognitive symptoms typically follows a sequential course. It could be, for example, that a young athlete took an elbow to the head during a basketball game, then has no appetite for dinner that night.
5. Concussion is typically associated with grossly normal structural neuroimaging studies.
The biggest concern is the risk of so-called “second-impact syndrome,” which can occur with another blow to the head before a concussion is healed. Second-impact syndrome can have severe consequences — including bleeding inside the skull, brain swelling and death.
Mild traumatic brain injury (MTBI): a term used interchangeably with the term concussion. Defined as impact to the head and a GCS score of 13 to 15, with or without only brief loss of consciousness or posttraumatic amnesia. Trauma-induced alteration in mental status, may or may not involve loss of consciousness. Concussion is any change in mental status caused by a sudden violent rocking back and forth of the brain inside of the skull due to a blow to the head or upper body. Sx’s can include H-A, amnesia, dizziness, confusion, lack of hand-eye coordination, and in some cases, loss of consciousness. Mechanical injury (trauma) to the brain causing transient alteration in neurological function such as loss of consciousness (<10%), disturbances in vision or equilibrium.
• A single sports-related concussion in an adolescent leads to a significant reduction in cerebral blood flow (CBF) that may persist for more than 1 month after the injury (Pediatrics. Published online November 30, 2011)……these “lingering ‘non-visible’ effects reinforce why return to play (and school) needs to be carefully and individually assessed, even without reported symptoms or obvious clinical signs.”……Improvement toward control CBF values occurred in only 27% of the concussed youth at 14 days postinjury, and 64% at more than 30 days postinjury.
• A study on of collegiate contact sport athletes found that the cognitive effects of smaller head impacts that do not cause concussion (subconcussive hits) were not apparent (Neurology 2012;78:1777)……the lack of preseason differences between contact and noncontact athletes in this study was reassuring.
• Even one season of repetitive head impacts (ice hockey or football) might have a negative effect on cognitive performance in college athletes (Neurology 2012;78:1777)……significantly more contact-sport athletes than noncontact-sport athletes (22% vs. 4%) performed more than 1.5 standard deviations below their predicted score on postseason tests of learning and memory (1.5 standard deviations was prospectively selected as a marker of “significantly poorer than expected” performance)……parents and young adults should be made aware to ensure informed decision making about contact-sport participation.
Leading causes: Falls. Motor vehicle trauma. Unintentionally struck by/against events as seen in assaults and sports. Players with a h/o previous concussion are more likely to have future concussive episodes than those with no history; 1 in 15 players with a concussion have additional ones in the same playing season (JAMA 2003;290:2549-55), supporting the time-honored rule of a 7-day recovery period before athletes with concussions may return to the playing field. TBIs have increased 21% since 2004, whereas the population has grown only 6.3%, according to new data from the CDC. In particular,
• TBIs are increasing among children as more become active in sports and among the elderly as that demographic grows (National Center for Injury Prevention and Control; 2010 via ww.cdc.gov/traumaticbraininjury/tbi_ed.html).
Loss of Consciousness (LOC): Inquire whether LOC occurred or was observed and the length of time the pt lost consciousness. Up to 90% of concussions do not involve LOC (Brain Injury 2006;20:889-94).
PP: Unlike more severe TBIs, the disturbance of brain function from MTBI is related more to dysfunction of brain metabolism rather than to structural injury or damage. The current understanding of the underlying pathology of MTBI involves a paradigm shift away from a focus on anatomic damage to an emphasis on neuronal dysfunction involving a complex cascade of ionic, metabolic and physiologic events. Scientists have increasingly linked the head injuries common in contact sports to neurodegenerative disorders, including motor neuron diseases (MND) such as amyotrophic lateral sclerosis (J Neuropathol Exp Neurol. 2010;69:918-929).
ICD-9 codes:
850.0 (Concussion, with no loss of consciousness).
850.1 (Concussion, with brief loss of consciousness < 1 hour).
850.9 (Concussion, unspecified)
959.01 Head injury, unspecified (not recommended for concussion/MTBI)
310.2 Postconcussion syndrome
• Teen athletes may be hesitant to report concussive symptoms because of concern over how their reports will be received by the coach according to data from varsity high school athletes from three football, two boys’ soccer, and four girls’ soccer teams in the Seattle, WA, area (50 participants) (J Adol Health. 2013;52:330-335.e3)….Athletes wanted to keep playing and knew that reporting symptoms might result in being removed from the game……athletes were also hesitant to report symptoms to coaches if they did not result in significant pain or disability.
Evaluation: Any athlete who is symptomatic requires serial neuro exams for as long as the sx’s persist to determine if there is deterioration. Initial observation & eval should be at least 15 min. The hallmark of sports-related concussion presents with functional deficits rather than structural deficits. Acutely, a concussed individual may display transient changes in cognition, postural ability, and symptom reports. See The Sport Concussion Assessment Tool (SCAT) |
CDC Concussion-Management Tool Kit: The Acute Concussion Evaluation (ACE) Form: Designed to aid in the initial evaluation and dx of pt’s with a known or suspected concussion and guidance for helping pt’s to recover and avoid reinjury. http://www.cdc.gov/ncipc/tbi/physicians_tool_kit.htm
3 major components that require evaluation: Characteristics of the injury. Types and severity of the sx’s. Risk factors that can lead to a protracted period of recovery.
1. Injury Description: Ask the pt (and/or parent, if child) about how the injury occurred, type of force, and location on the head or body where the force (blow) was received. Different biomechanics of injury may result in varied symptom patterns. For example, an injury that occurs to the posterior aspect of the head may result in visual changes, balance problems, and fatigue. The force to the head may be indirect, such as with an individual being struck in the body resulting in the head accelerating forward and then backward quickly (e.g., whiplash). The cause of the injury may also help to estimate the force of the hit or blow the pt sustained. The greater the force associated with the injury, the more likely the pt will present with more severe sx’s.
Exertion. Inquire whether any sx’s worsen with exertion, that is, with physical activity (e.g., running, climbing stairs, bike riding) and/or cognitive activity (e.g., academic studies, multi-tasking at work, reading or other tasks requiring focused concentration). Indicating incomplete recovery, which may also be protracted with over-exertion.
Orientation –> person/ place/ time/ situation.
Q’s to ask athlete: At which field are we playing? What team are we playing? Which quarter (period, half) is it? How far into the quarter (period, half) is it? Which team scored last? What team did we play last week? Did we win?
Concentration –> digits or mo’s in reverse order.
Memory –> 3 objects at 0 & 5 min. Recent newsworthy events, teams in sporting contest.
Immediate Sx’s: vacant stare, confusion, disorientation, slurred speech, gross lack of incoordination, emotional lability, memory deficits (repeatedly asking questions already answered, inability to recall 3 words in 5min), LOC (paralytic coma, unresponsive to arousal), delayed verbal and motor responses. Vacant stare.
Delayed Sx’s: Altered taste or smell. Amnesia or memory difficulty. Anxiety. Attention deficits. Blurred vision. Depression. Dizziness, vertigo. Emotional lability or irritability. Fatigue. Headache. Impaired coordination. Intolerance to light or smells. Lethargy. Loss of consciousness. Nausea, vomiting. Postural instability. Sleep disturbance. Tinnitus.
Amnesia (Retrograde): memory loss that has occurred for events before the injury. Determine the length of time of memory dysfunction as research indicates that even seconds of amnesia may predict more serious injury.
Amnesia (Anterograde): Determine whether amnesia has occurred for events after the injury. Also referred to as post-traumatic amnesia (PTA).
Check pupils, coordination (FTN, tandem gait), sensation.
Provocative testing –> sprints 40 yards, 5 push/ sit ups looking for sx’s or signs.
Reflexes: A simple visuomotor test may help clinicians identify concussion in young people who are often not otherwise monitored (American Academy of Neurology (AAN) 62nd Annual Meeting: Abstract 1215. Presented April 10-17, 2010)……”It is a standardized and simple clinical measure of reaction time…..the examiner released a rigid cylinder affixed to a weighted disk to assess how quickly they were able to catch it.
Questions to Detect Acute Sensorial Dysfunction After a Head Injury
“Hello,what is your name?”(orientation to person)
“Who am I?” (orientation to person and your role as a physician: an athlete should know the team physician)
“What is the day and date?”“What is the time of day?” (orientation to time)
“Where are we?” (orientation to place: practice field or stadium)
“What has just happened to you?” or “What was the last play?” (current events and recent memory)
“What team are you playing?” (current events and recent memory)
“What is the score of the game?” (current events and recent memory)
“Can you repeat the months of the year backward?”(comprehension and attention span)
“Can you remember these three items?” Recite an item such as table, a color, and an address and ask the patient to repeat them after a few minutes. (recent memory)
Ask about pain, blurred or double vision, tinnitus, dizziness, and numbness or tingling. (Checks current neurologic symptoms)
Neuroimaging: Isolated LOC or amnesia does not predict brain injury in pt’s with blunt head trauma, these isolated sx’s do not need to be investigated with cranial CT as <2% rate of traumatic brain injury (Pediatrics 2004;113:e507-e513). Immediate CT was more cost-effective than admitting pt’s for 24-hour hospital observation in pt’s with confirmed or suspected loss of consciousness or amnesia before ED arrival, a normal neurologic exam (BMJ 2006;333:465-8).
• Children with mild TBI (40% had LOC and 18% had brain abnormalities on MRI) can experience physical and cognitive symptoms and impaired function for many months (Arch Pediatr Adolesc Med 2012:Mar 5;e-pub ahead of print)……somatic and cognitive symptoms at 2 weeks predicted lower ratings of physical health-related quality of life (HRQOL) at 3 months postinjury.
• A study has suggested that sports-related concussions in children may lead to some measurable emotional and behavioral functioning problems in the months that follow the injury (American Academy of Neurology (AAN) 65th Annual Meeting. Abstract P01.256. Presented March 18, 2013). In the end, they extrapolated their recommendations for children from data showing that high school athletes tend to take longer for improvement in symptoms and neurocognitive performance after a concussion…..athletes younger than high school might show the same trend.
Tx: Office monitoring: appropriate if the number and severity of sx’s are steadily decreasing over time and/or fully resolve within 3 to 5 days. If sx’s not abating or worsen, referral to an MTBI specialist may be warranted. Consider diagnostic testing such as neuroimaging (CT or MRI scan) or neuropsychological testing (helpful for confirming self-reported sx’s and tracking recovery). See Grade & Returning to Play (Sports and Recreation) | Post Concusion Syndrome & Recovery Stages |
Rest: Increased rest and limited exertion are important to facilitate the pt’s recovery. Physicians should be cautious about allowing pt’s to return to driving, especially if the pt has problems with attention, processing speed, or reaction time. Pt’s should also be advised to get adequate sleep at night and to take daytime naps or rest breaks when significant fatigue is experienced.
• No sports participation until sx’s resolve. Generally, an athlete can safely recover from an initial concussion as long as the brain has had time to heal. Returning an athlete to play before the brain has had time to heal places that athlete at risk for a second concussion and further, more serious injury. Sx’s may persist for weeks to mo’s.
• College football players require an average of 1 week for post-concussive sx’s to subside, and those players with a history of concussion are more likely to experience future concussive injuries (JAMA 2003;290:2556-2563), 90% had grade 1 or 2 concussions, 6.4% experienced loss of consciousness (median duration of 30 sec), while post traumatic amnesia (19.1%) or retrograde amnesia (7.4%) common.
• Contact-sports players who experience one traumatic brain injury are at increased risk for a second concussion soon thereafter (lowers an individual’s injury threshold) (JAMA 2003;290:2549-2563,2604-2605), moreover, it may take several days before sx’s, cognition, and postural stability return to normal, and recovery may take longer in pt’s with a recurrent concussion.
• Several websites have concussion management software that tests reaction time, memory, problem solving and information processing at cogstate.com, headminder.com, impacttest.com.
• A major depressive episode is fairly common after a mild traumatic brain injury, especially among pt’s with abnormal CT results or signs of depression 1 week after injury (Arch Gen Psychiatry 2005;62:523-528).
• High school and college athletes with migraine H-A characteristics after a concussion may have increased neurocognitive impairment (J Neurosurg 2005;May)….should not be allowed to return to play before the H-A resolves as may suffer from second-impact syndrome, rare but catastrophic. Rivastigmine (Exelon): effective in treating moderate to severe memory loss in a subgroup of pt’s who have suffered traumatic brain injury (Neurology. 2006; 67:748-755, 936).
• After a concussion, taking a week off from nearly all mental and physical activity — including television, talking on the phone and visiting with friends – may be linked with improved mental performance and fewer symptoms a study suggests (J Pediatr 2012;online May 24th)…..Even when the week of total rest came months after the injury occurred, it still had benefits on post-concussion syndrome involves headaches, mental fogginess, fatigue, and difficulty concentrating or sleeping, among other symptoms. “Back off physical and cognitive activity until your symptoms improve and avoid things that provoke and make your symptoms worse. That’s ideal because then you can individualize.”
Grade & Returning to Play (Sports and Recreation):
Grade 1 (mild): transient confusion only, no LOC, Posttraumatic amnesia (PTA) < 30min. Temporarily observe. Can return to play if normal / asymptomatic within 15-20 min (some say if asymptomatic X 1week). If happens again, then no play X 2wks. 3rd time then out for the season, no contact sports for 3mo. Having one’s “bell rung” (mild, or “ding,” concussion) is often considered “normal” in athletics, but it can cause substantial morbidity (Am J Sports Med 2004;32:47-54), caution is advised as overzealous parents, coaches, and athletes might minimize sx’s to maximize playing time, current return-to-play guidelines might not be stringent enough as 36 hours after injury, the athletes still demonstrate significant declines in memory and dramatic increases in self-reported sx’s compared with baseline measurements.
Grade 2 (moderate): LOC <5min (seconds to minutes). Confusion & PTA >30 min but <24hr. May be dizzy. Remove from event. If sx’s persist >1hr then to medical. May return to play in 1 week if asymptomatic. 2nd episode, then no play X 1mo. 3rd , then terminate the season.
Grade 3 (severe): LOC >5min or PTA >24hr + retrograde amnesia. Transport to hospital for evaluation. Can return to play in 1mo if asymptomatic for 1 week. If 2nd or +imaging study, then terminate season. H/o neurosurgery, then contact sports contraindicated.
Complications:
Posttraumatic amnesia: anterograde (new memories) or retrograde (unable to recall info before injury). Can last for hours to weeks, correlates with the LOC and severity of injury. Memory problems 24 hours postconcussion also correlated with injury severity (Curr Opin Orthopedics 2003;14:392-397).
Post-traumatic Headache: common (~100%). May be tension, occipital, migrainous, supraorbital or infraorbital. Traumatic hemorrhage must always be ruled out. Some correlation between duration and severity of injury. Most improve in 5mo. Give NSAIDs, TCA, stress management, biofeedback, rehab. The presence of any postconcussion H-A 7 days after injury was associated with other postconcussive sx’s such as slower reaction times, and reduced memory.
• In a prospective study of 100 patients, 66% reported headaches (“no typical characteristics”) in the 7 to 10 days immediately following mild head injury (Cephalalgia 2011;31:1618)…..resembled migraine or probable migraine in 35% of those with headache….Predictors of headache included other chronic pain, pre-existing headache, “post-traumatic symptoms,” and concurrent mood changes.
Posttraumatic seizures: can happen immediately or after 1yr, 80% who will have one have it by 2yrs. Incr risk with early onset sz’s, >2 in first wk or >3 in first yr. Prophylaxis is controversial.
Insomnia: Minor traumatic brain injuries (mTBI) may contribute to the emergence of new circadian-rhythm sleep disorders (CRSD), most commonly delayed sleep-phase syndrome or an irregular sleep-wake pattern (Neurology 2007; 68:1136-1140)…..as many as 40% to 65% of pt’s with minor traumatic brain injuries complain of insomnia and this can exacerbate other sx’s, such as headache, emotional distress, and cognitive impairment, and compromise the rehabilitation process.
Second Impact Syndrome: a 2nd minor blow can result in loss of autoregulation of the brains blood supply causing vascular engorgement and herniation. An initial concussion increases the likelihood of subsequent concussion four- to sixfold (Am J Phys Med Rehabil 2003;82:653-9). Repeated concussions do not result in greater neurocognitive impairment than that caused by previous concussions of similar severity, however, repeated concussions result in more reported sx’s and a greater risk of persistent postconcussion sx’s (J Neurosurg 2003;98:477-84).
Multiple Concussions –> punch drunk. Seen in boxers. Traumatic brain injury, whether mild, moderate, or severe, has been linked to a doubling of dementia risk (HR 2.6) according to data from 281,540 U.S. veterans aged 55 years or older (Alzheimer’s Association International Conference (AAIC). P2-117. Presented July 18, 2011)……The unadjusted risk for dementia was more than double in those with TBI compared with those with no TBI, at 15% vs 7%, respectively….several potential mechanisms have been proposed to explain the link between TBI and dementia: that TBI is associated with diffuse axonal injury or swelling of the axons that form connections between the neurons, which disrupts neuronal communication…or TBI increases the risk of developing tau tangles and ß-amyloid plaques…or over the longer term, axonal degeneration may occur, even after a single TBI.
An athlete with concussion should not return to practice or competitive play until all symptoms have resolved, in order to avoid the risk for further injury during the vulnerable period before the brain has recovered (Clin J Sport Med. 2013;23:1-18).
• Any athlete suspected of having concussion should be immediately removed from play and assessed by a healthcare professional trained in the evaluation and management of concussions.
• “There is no same day return to play for an athlete diagnosed with concussion,” the statement advises.
• It also discusses the evidence and limitations of different types of tests and assessments in athletes with concussion; for many tests, further research is needed to validate their use, the authors note.
• Supports the use of checklists for assessing concussion symptoms and tracking them over time. Computerized neuropsychological tests can be useful if performed by experts but are not necessary for most athletes with concussions, the authors conclude.
• Emphasizes the need for complete recovery before return to play for any athlete with concussion.
• There is no evidence that equipment, including helmets or mouth guards, reduces concussion risk. “Greater efforts are needed to educate involved parties including athletes, parents, coaches, officials, school administrators, and health care providers to improve concussion recognition, management, and prevention,” the statement reads.
The Ohio State University Sports Medical Center’s standard return-to-play exertional protocols:
(Concussion Assessment and Management. Clin Sports Med 2010;29:1)
Standard Return to Play:
Day 1: 30 to 40 minutes of nonimpact aerobic activity.
Exercise bike 15 minutes up to heart rate of 120 beats per minute (bpm).
Cool down for 5 minutes.
Increase intensity, maximum heart rate of 145 to150 bpm, maintain for 15 minutes.
Cool down for 5 minutes.
No additional physical exertion. Immediately discontinue activity if there is any increase in athletes’ symptoms and return to rest without physical activity until symptoms resolve.
Day 2: 45 minutes of aerobic activity including jogging, running, sprints, or position-specific athletic drills; no contact
Cool down for 5 minutes
After at least 30 minutes rest, may lift weights for 30 minutes. Immediately discontinue activity if there is any increase in athletes’ symptoms and return to rest without physical activity until symptoms resolve.
Day 3: Full participation practice. Immediately discontinue activity if there is any increase in athletes’ symptoms and return to rest without physical activity until symptoms resolve.
Day 4: Full game participation. Individuals who have a suspected concussion must not be permitted to resume contact or regular activity until they can move with usual dexterity and speed and are perfectly oriented as to the time, place, their own identity, and are able to identify the activities in which they were engaged just before the injury. Each institution can develop their own return-to-play protocols, however the protocol should be a graduated, step-wise protocol with a return to rest upon the presence of symptoms. Further, return-to-play protocols can be extended to fit the severity and duration of initial cognitive symptoms.
The Ohio State University Sports Medical Center’s extended return-to-play exertional protocols:
Extended 5-Day Return to Play
Day 1: 30 to 40 minutes of nonimpact aerobic activity.
Exercise bike 15 minutes up to heart rate of 120 bpm.
Cool down for 5 minutes.
Increase intensity, maximum heart rate of 145 to150 bpm, maintain for 15 minutes.
Cool down for 5 minutes.
No additional physical exertion. Immediately discontinue activity if there is any increase in athletes’ symptoms and return to rest without physical activity until symptoms resolve.
Day 2: 30 to 40 minutes of nonimpact aerobic activity.
Exercise bike 10 minutes up to heart rate of 120 bpm.
Cool down for 5 minutes.
Increase intensity, maximum heart rate of 145 to150 bpm, maintain for 25 minutes.
Cool down for 5 minutes.
No additional physical exertion. Immediately discontinue activity if there is any increase in athletes’ symptoms and return to rest without physical activity until symptoms resolve.
Day 3: 45 minutes of aerobic activity including jogging, running, sprints, or position-specific athletic drills; no contact.
Cool down for 5 minutes.
After at least 30 minute rest may lift weights for 30 minutes. Immediately discontinue activity if there is any increase in athletes’ symptoms and return to rest without physical activity until symptoms resolve.
Day 4: Full participation practice.
Immediately discontinue activity if there is any increase in athletes’ symptoms and return to rest without physical activity until symptoms resolve.
Day 5: Full game participation.
Precautions and recommendations. During rehabilitation or follow-up, the referring physician should be aware of signs and symptoms of worsening conditions. Further, the physician should caution all of those involved with the rehabilitation process regarding stipulations following a concussive injury. This may include strength and conditioning coaches, academic advisors, and others that have interaction with athletes who have concussions. If athletes report an increase in symptoms, the medical professional should decrease cognitive and physical exertion. Further stipulations include:
• symptoms increasing with mental and physical exertion.
• mental status changes.
• worsening strength deficits.
Post Concussion Syndrome (PCS):
Equilibrium disturbances that may persist for 1-2 weeks. Should check neuroimaging or neuro psych testing. The occurrence and severity not related to the type or severity of injury, duration of the post-traumatic amnesia or duration of the LOC. Most return to premorbid functioning within 3-5mo. A stduy with 201 pt’s with mild traumatic brain injury (TBI) and PCS found that the greatest predictors of low PCS at 6 months were low posttraumatic stress and low PCS early after injury and no premorbid physical problems (J Neurol Neurosurg Psychiatry 2008;79:936)…..Full return to work was predicted by having more than 11 years of education, absence of nausea or vomiting on admission, no additional extracranial injuries, and no severe pain early after injury….editorialist notes that “the study allows physicians to assure patients of their good prognosis and elucidates factors that indicate the need for more-intensive evaluation and treatment”.
Early Sx’s (min to hours): H-A, dizzy, N/V, lack of awareness of surroundings, tinnitus, visual changes. Postconcussion sx’s are common after mild TBI (GCS of 14-15), physical sx’s predominate early (dizziness in 74%, headache in 45% andfatigue in 24%); emotional sx’s predominate late (J Trauma 2007;62:657-63)….At 8 weeks, ongoing headache, dizziness, fatigue, poor vision, nausea, and depression were significantly associated with poor recovery.
Fatigue: It is unkown whether fatigue in TBI is related to sleepiness or to other factors (e.g., so-called central fatigue related to TBI) (Neurology 2008;71:1609)……mild sleepiness tends to worsens fatigue in these patients.
Late Sx’s (days to weeks): persistent low-grade H-A, light headed ness, poor attention/ concentration, memory dysfunction, easy fatigability, sleep disturbance, anxiety/ depression, irritable, intolerance to bright lights, difficulty focusing vision, intolerance to loud noises, tinnitus, personality changes.
• Postconcussive symptoms persist for at least 1 month in most (63%) patients according to a study on 68 patients after minor head injury (J Emerg Med 2011;40:262)……The most persistent symptoms were headache (42%), dizziness (29%), fatigue (28%), and cognitive impairment (28%)…….Athletes should be advised to avoid both exertion and contact until all symptoms have resolved and they have been cleared to return to playing sports by a physician knowledgeable about sports-related concussion.
• A study found that three months after mild traumatic brain injury (mTBI), 14% of children over six still had increased fatigue, emotionality, irritability, headaches and other symptoms characteristic of PCS (Pediatrics 2010;online July 26).
“Fogginess” may predict recovery: A depersonalization feeling described as if being underwater, a step removed from their surroundings or having regressed from a world of HDTV to regular TV. According to data on 108 high school age athletes, those with fogginess were 4.3-fold more likely to have a slower recovery (mean of 29 vs 6 days) (Fam Prac News 2009;39:14).
Neuropsychiatric Disorders: treatment often focuses on “neurological” symptoms — e.g., cognitive or physical symptoms in traumatic brain injury (TBI) or number of seizures in psychogenic nonepileptic seizures (PNES). Addressing mood or anxiety issues may improve these patients’ quality of life (J Neuropsychiatry Clin Neurosci 2009;21:181)….For TBI patients, depression worsens all symptoms, whether typical depressive symptoms (e.g., sleep, mood, or concentration) or somatic ones (e.g., vision impairments, nausea, headaches, or dizziness). QOL in PNES was related to depression and somatic symptoms, not seizure frequency.
• It is the psychiatric disorder, not the injury, that affects functional impairment and quality of life pt’s with mild traumatic brain injury (mTBI) and thus mental health professionals have a key role in treating patients with TBI (Am J Psychiatry 2010 Jan 4;e-pub ahead of print).
• Young adults who’ve suffered head injuries are more likely to get into a fight or take part in other kinds of violence (Pediatrics 2011;online May 29th)……brain injuries can cause changes in emotions, including impulsivity and aggression.
• Kids who have a concussion or other traumatic brain injury are more likely to develop headaches for up to a year afterward than children who sustain injuries elsewhere (Pediatrics 2011;online December 5).
• Headaches, as well as neurologic and psychiatric symptoms related to post-concussion syndrome (PCS), can last up to 8 years after a traumatic brain injury (TBI) a study of veterans has shown (American Headache Society 54th Annual Meeting. Posters 82 and 83. Presented June 21, 2012)…..”Many of the up to 25% of soldiers returning from combat zones who have suffered a significant TBI continue to experience the after-effects over time.” Experts have noted that modern weapons are designed to maximize the explosive force transmitted to a target. They are refined in such a way that they intensify the generated force or shock waves and cause maximum damage. These study results challenge the notion that everyone who gets their “bell rung” from a head injury will be back to normal if they just “wait awhile until the cobwebs get cleared out,” said Dr. Couch. “This might be so in most cases, but not all,” he said. The incidence of headache was 95% to 97% over the 8-year period, with almost half of headache sufferers manifesting severe or very severe headache problems. 30% to 40% of both groups had minimal or mild/moderate depression. Headache and depression may coexist, possibly because of involvement of genes related to the serotonin system.
Depression: Researchers look at the possible predictors for depression (seen in 53%) after TBI and the effects on patients 1 year later (JAMA 2010;303:1938)…..Post-injury depression occurred in 68% of those with prior depression and in 41% of those without. After adjustment for multiple baseline factors associated with depression, post-injury depression risk was significantly increased in those with depression at the time of injury, prior depression history, or lifetime alcohol dependence…..significantly more depressed participants had anxiety disorders than nondepressed participants (60% vs. 7%)…..In addition, TBI is associated with increased comorbidity and poorer health-related quality of life in those with MDD than in those without MDD……an invisible disorder within an often invisible injury. A study using polysomnography confirms sleep disturbances in patients with TBI, including increased wake after sleep onset (WASO) and reduced sleep efficiency, an average of 14 months after their injury compared with healthy control subjects (Neurology. 2010;74:1732-1738)…..Other findings, including reduced evening melatonin production in these patients, as well as increased levels of depression and anxiety, may be contributing to these problems.
Signs of Deteriorating Neurological Function: If any of these signs are reported, they should be referred to an emergency department for an immediate medical evaluation. Headaches that worsen. Seizures. Focal neurologic signs (Weakness or numbness in arms or legs). Looks very drowsy or can’t be awakened. Repeated vomiting. Slurred speech. Can’t recognize people or places. Increasing confusion or irritability. Onset / worsening of neck pain. Unusual behavior change. Significant irritability.
Females: Female and high school athletes may need more time to recover from a concussion than their male or college counterparts according to data on 222 pt’s (Am J Sports Med 2012;April 26th)……Overall, females complained of more symptoms (e.g., headache, dizziness, nausea, ringing in the ears, fatigue and confusion) than their male counterparts — an average of 14 symptoms, versus 10……High school athletes improved more slowly than older athletes.
• Mindfulness-based cognitive therapy (MBCT) reduces symptoms of depression in individuals with traumatic brain injury (TBI) research suggests (EPA 2013: 21st European Congress of Psychiatry: Abstract 1494. Presented April 7, 2013). Patient interventions consisted of 10 weekly sessions of 1.5 hours with consideration of issues associated with TBI, such as memory, fatigue, and concentration, using simplified language and repetition to reinforce learning. A book and compact disk were provided to facilitate meditation, which was recommended for 20 to 30 minutes a day.
W/u: can send pt to a regional neuro-psychiatric clinic for eval and rehab. Acute changes in the corpus callosum visible on magnetic resonance diffusion tensor imaging (DTI) up to 6 days after mild traumatic brain injury are related to postconcussion symptoms a small study indicates (Neurology 2008;70:948-955)……Despite normal head CT imaging and neurologic functioning, many individuals report postconcussion symptoms following mild traumatic brain injury……”DTI may prove to help in refining diagnosis, therapeutic intervention, and management of mild traumatic brain injury.”
• Moderate to severe brain trauma increases the risk of pituitary abnormalities that warrant investigation before they become symptomatic (ENDO 2009;Abstract P3-625)…..45% of a retrospectively identified group had endocrine abnormalities consistent with pituitary dysfunction, while growth hormone deficiency accounted for the largest proportion of cases, 10% to 20% of patients had evidence of multiple hormonal disorders.
Warn All Pt’s: RTC if severe or worsening H-A, difficulty with vision, vomiting, fever, stiff neck, urinary/bowel incontinence, weakness or numbness, somnolence or confusion, restlessness, unsteadiness, sz, inability to awaken pt.
• Symptoms (attributable to “organic” brain injury, not psychological factors) persist longer than 5 years in some pt’s after mild TBI (Acta Neurol Scand 2007;115:398)….this study doesn’t help us predict which pt’s these will be or why.
• Somatic sx’s or their treatments may produce cognitive sx’s in postconcussive syndrome (PCS) (J Int Neuropsychol Soc 2006;12:792). A loss of brain tissue after a traumatic head injury may help explain the cognitive and emotional fallout that often follows the event (Neurology 2008;70:771-778)….using high-resolution MRI, researchers found a stepwise, dose-response relationship between loss of volume and brain injury, encompassing both frontal and posterior brain regions……even patients with a mild injury had changes that could be reliably distinguished from the noninjured controls…..helps explain the well-known substantial handicap that patients have in the wake with a traumatic brain injury, particularly with concentration, working memory, organizing, planning, and mood changes……A spatially extensive pattern of volume loss varied along with injury severity, with particularly widespread effects in white matter volume and sulcal/subdural cerebrospinal fluid…..Focal lesions were associated with greater loss of volume in the left medial ventral frontal and posterior temporal regions, but volume loss included other regions and remained marked even when analyses were restricted to patients with diffuse injury…..Loss of white matter, also widespread, was greatest in the lateral superior frontal, superior parietal, posterior temporal, and posterior cingulated regions bilaterally, with a tendency toward greater volume loss in the right hemisphere.
• The frequency of symptoms such as fatigue, headache, sleep difficulties, and irritability weres similar in patients with mild TBI and in those with trauma but no TBI at day 5 according to a study on 175 hospitalized patients (J Neurol Neurosurg Psychiatry 2008;79:300)……Clinicians should emphasize evaluating individual symptoms in trauma patients, rather than diagnosing a “syndrome,” which may have differing pathophysiologic substrates.
• Recovery from a concussion may take longer for female athletes than for males, with a more symptomatic recovery according to a study on 141 females and 93 male soccer players with an average age of 16.3 (American Orthopaedic Society for Sports Medicine meeting 2008;July).
• A study shows that repeated head hits during a single season generally don’t have detrimental effects for athletes playing contact sports, however, findings among young athletes showed a subgroup of athletes for whom impacts to the head appeared to affect learning and memory (Neurology. 2012;78:1777-1784,1712-171).
Stages of Recovery:
1. No activity. Complete rest. Once asymptomatic can proceed to level 2.
2. Light aerobic exercise such as walking, or stationary cycling. No resistance training.
3. Sport-specific exercise: such as skating in hockey, running in soccer. Progressive addition of resistance training at steps 3 or 4.
4. Noncontact training drills.
5. Full contact training after medical clearance.
6. Game play. (2nd International Conf on Concussion in Sport (Clin J Sport Med 2005;15:48-55)
PV: The concussion tool kits will be distributed by the CDC to coaches, principals, and athletic directors at high schools can also be ordered or downloaded free of charge at http://www.cdc.gov/ncipc/tbi/coaches_tool_kit.htm.
Wear a helmet when: riding a bike, motorcycle, snowmobile, scooter, or all-terrain vehicle; playing a contact sport, such as football, ice hockey, lacrosse, or boxing; in-line skates or riding a skateboard; Batting and running bases in baseball or softball; Riding a horse; or Skiing, sledding, or snowboarding. Wear a seat belt every time they drive or ride in a motor vehicle. Follow the safety rules and those for the sport. Practice good sportsmanship.
Make living areas safer for seniors by: Removing tripping hazards such as throw rugs and clutter in walkways; Using nonslip mats in the bathtub and on shower floors; Installing grab bars next to the toilet and in the tub or shower; Installing handrails on both sides of stairways; improving lighting throughout the home; and Maintaining a regular physical activity program, if their health care provider agrees, to improve lower body strength and balance.
Make living areas safer for children by: Installing window guards to keep young children from falling out of open windows; Using safety gates at the top and bottom of stairs when young children are around; Keeping stairs clear of clutter; Securing rugs and using rubber mats in bathtubs; and Not allowing children to play on fire escapes or on other unsafe platforms. Make sure playground surfaces are made of shock-absorbing material, such as hardwood mulch or sand, and are maintained to an appropriate depth.
• Most youth recover fully after concussion, but research suggests there is a vulnerable period when a second impact can result in intracerebral hemorrhage, cerebral edema, or death. The first concussion law was passed in Washington State in 2009 (The Zackery Lystedt Law), and similar laws have now been passed in other states. These laws require athletes to be removed from play if they have a suspected concussion and not return to play until cleared by a clinician. They also stipulate concussion education for coaches, athletes, and parents. However, there are no provisions for concussion detection. Concussion-causing collisions can be subtle, and signs and symptoms of concussion (such as headache, nausea, and dizziness) are often nonspecific. Although athletic trainers are helpful for concussion detection, only about 42% of high schools in the United States employ an athletic trainer.
Sport Concussion Assessment Tool (SCAT):
One of the most commonly used sideline assessments. It includes a concussion symptom checklist, concentration and memory tasks, and neurologic screening; however, reliability and validity evidence is unavailable at this time. The two-sided SCAT card includes an index card-sized section for the athlete to self score 18 sx’s and a brief sideline medical evaluation. This tool represents a standardized method of evaluating people after concussion in sport. Err on the side of being conservative when you use the SCAT card in a bright, noisy arena, a retreat to the locker room can remove the physician and the player from the pressure of the arena.
Name: _____________________ Date: __________
Sport/Team: ________________ Mouth Guard? Y N
1) SIGNS
Was there loss of consciousness or unresponsiveness? Y N
Was there seizure or convulsive activity? Y N
Was there a balance problem/unsteadiness? Y N
2) MEMORY
Modified Maddocks questions (check those correct)
At what venue are we? ___ Which half is it? ___ Who scored last? ___ What team did we play last? ___ Did we win last game? ___
3) SYMPTOM SCORE Total number of positive sx’s (from “SYMPTOMS” box on other side of the card) = ______
4) COGNITIVE ASSESSMENT (Check those correct) 5 word recall
Immediate Delayed (after concentration tasks)
Word 1 _______ cat ___ ___
Word 2 _______ pen ___ ___
Word 3 _______ shoe ___ ___
Word 4 _______ book ___ ___
Word 5 _______ car ___ ___
Months in reverse order (circle those incorrect) Jun-May-Apr-Mar-Feb-Jan-Dec-Nov-Oct-Sep-Aug-Jul
OR
Digits backwards (check those correct)
5-2-8 3-9-1 ___
6-2-9-4 4-3-7-1 ___
8-3-2-7-9 1-4-9-3-6 ___
7-3-9-1-4-2 5-1-8-4-6-8 ___
Ask delayed 5-word recall now
5) NEUROLOGICAL SCREENING Pass / Fail
Speech ___ ___
Eye Motion and Pupils ___ ___
Pronator Drift ___ ___
Gait Assessment ___ ___
Any neurologic screening abnormality necessitates formal neurologic or hospital assessment.
6) RETURN TO PLAY ATHLETES SHOULD NOT BE RETURNED TO PLAY THE SAME DAY OF INJURY.
When returning athletes to play, they should follow a stepwise sx-limited program, with stages of progression. For example:
1. rest until asymptomatic (physical and mental rest)
2. light aerobic exercise (e.g. stationary cycle)
3. sport-specific training
4. non-contact training drills (start light resistance training)
5. full contact training after medical clearance
6. return to competition (game play)
There should be ~ 24 hours (or longer) for each stage and the athlete should return to stage 1 if sx’s recur. Resistance training should only be added in the later stages. Medical clearance should be given before return to play.
INSTRUCTIONS: For the use of medical doctors, physiotherapists or athletic therapists. In order to maximize the information gathered from the card, it is strongly suggested that all athletes participating in contact sports complete a baseline evaluation prior to the beginning of their competitive season. This card is a suggested guide only for sports concussion and is not meant to assess more severe forms of brain injury.
Signs: Assess for each of these items and circle – Y (yes) or N (no)
Memory: Select any 5 words (an example is given). Avoid choosing related words such as “dark” and “moon” which can be recalled by means of word association. Reach each word at a rate of one word per second. The athlete should not be informed of the delayed testing of memory (to be done after the reverse months and/or digits). Choose a different set of words each time you perform a follow-up exam with the same candidate.
SYMPTOMS: Headache, “pressure in the head”, neck pain, balance problems or dizziness, nausea or vomiting, vision problems, hearing problems or ringing in the ears, “don’t feel right”, feeling “dinged” or “dazed”, confusion, feeling slowed down, feeling like in a “fog”, drowsiness, fatigue or low energy, emotional, irritable, difficulty concentrating or remembering
Concentration/Attention: Ask the athlete to recite the months of the year in reverse order, starting with a random month. Do not start with December or January. Circle any months not recited in the correct sequence. For digits backwards, if correct, go to the next string length. If incorrect, read trail 2. Stop after incorrect on both trials.
Neurologic Screening: Trained medical personnel must administer this examination. These individuals might include medical doctors, physiotherapists or athletic therapists. Speech should be assessed for fluency and lack of slurring. Eye motion should reveal no diplopia in any of the 4 planes of movement (vertical, horizontal and both diagonal planes). The pronator drift is performed by asking the pt to hold both arms in front of them, palms up, with eyes closed. A positive test is pronating the forearm, dropping the arm, or drift away from midline. For gait assessment, ask the pt to walk away from you, turn and walk back.
Return to Play: A structured, graded exertion protocol should be developed; individualized on the basis of sport, age and the concussion history of the athlete. Exercise or training should be commenced only after the athlete is clearly asymptomatic with physical and cognitive rest. A doctor should ideally make final decision for clearance to return to competition. (Clin J Sport Med 2005; 15:48-55) (Br J Sport Med 2005;39: 196-204)
DETECT (Display Enhanced Testing for Concussions and Mild Traumatic Brain System): could help physicians, athletic trainers, parents, or coaches decide when it is safe to send an athlete back into the game. The device can “detect brain injuries right on the sidelines of a football game, on a battlefield, or in the emergency room. computer-driven, interactive headset of oversized goggles and earmuffs envelops the player’s ears and eyes, shutting out most noise and all light. Immersed in a virtual environment, the athlete would take a seven-minute mini-neuropsychological exam by pressing one of two buttons on a handset. The results of the sideline exam would be compared with pre-season baseline scores for signs of cognitive impairment. Neuropsychological assessment should not be the sole basis of a return to play decision but rather be seen as an aid to the clinical decision making. Neuropsychological testing should not be done while the athlete is symptomatic since it adds nothing to return-to-play decisions and it may contaminate the testing process by allowing for practice effects to confound the results.
Links: Prognosis & Tx | Skull Fx | Spinal Cord | Coma | See Hemorrhagic (Subdural / Epidural) | Subarachnoid Hemorrhage & Intracranial aneurysm |
GCS <8. Emergency dx & therapeutic procedures to establish satisfactory cerebral perfusion pressures (MAP > 90mmHg).
Factors that Portend Worsened Prognosis after Traumatic Brain Injury:
Extremes of age <2 or >60 yr.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








