KEY POINTS
Intravascular access device–associated infections may be either local or bacteremic, and the risk of developing an infection varies with the patient population, the type of device, the microbe, and the patient-microbe-device interaction.
The status of all indwelling vascular access devices should be reviewed daily by the critical care team, with attention to the duration of placement, appearance of the exit site, and continued clinical indication for the intravascular device.
Central venous catheters account for over 90% of all intravascular device–related bacteremias.
Most intravascular device–related bacteremias are caused by endogenous skin flora at the catheter insertion site that migrate along the transcutaneous portion of the catheter with subsequent colonization of the catheter tip.
Coagulase-negative staphylococci and Staphylococcus aureus account for just over 50% of all intravascular device–related bacteremias, followed in frequency by gram-negative bacilli and yeast.
Diagnosis of intravascular device–related infection, either local or bacteremic, is best approached using a combination of clinical and laboratory criteria.
Although treatment of central-line infections due to coagulase-negative staphylococci may be successful without catheter removal, infections caused by S aureus necessitate catheter removal.
Central intravascular catheter infections are essentially preventable infections. Successful prevention entails attention to a careful needs assessment for the device, careful site selection, maximal barrier precautions and sterile technique on insertion, insertion by the most skilled operators, rigorous catheter-site care, and interrupting the integrity of the system as little as possible.
The use of intravascular access devices has become an integral part of modern patient care, and nowhere is this more evident than the intensive care unit (ICU). Over the years, an increasing array of devices other than the original peripheral and single-lumen central catheters have been introduced. There is currently no standardized nomenclature for vascular access devices and they may be differentiated based on the number of lumens, site of insertion, use of cuffs or tunneling, category, or even by name. From a generic perspective they may be classified as percutaneously inserted peripheral or central lines and totally implantable devices. Central lines may be further distinguished as tunneled or nontunneled and noncuffed or cuffed. The most frequently encountered devices are single lumen peripheral lines, noncuffed, nontunneled multilumen central venous catheters (CVCs), tunneled and cuffed CVCs, flow-directed pulmonary artery catheters (PACs), peripherally inserted central and midline catheters, peripheral arterial catheters, and implantable devices. Intraosseous vascular access lines may occasionally be encountered.
These intravascular access devices provide a route for the administration for fluids, blood products, nutritional products, and medications; allow the monitoring of hemodynamic functions; and permit bloodletting and the maintenance of emergency access. However, vascular access devices may be associated with several complications, including local site infection, bacteremia, clinical sepsis without bacteremia, line fracture and extravasation of fluids or drugs, obstruction by medication, thrombosis, thrombophlebitis, and septic thrombophlebitis. Infectious complications are the most frequent and among the most serious of these complications. The magnitude of CVC-related infectious complications can be appreciated when one realizes there are an estimated 15 million days of exposure to CVCs in patients in ICUs in the United States each year with 80,000 cases of central line–associated blood stream infections (CLABSI) annually.1 Catheter-related infections are associated with significant morbidity and mortality with attributable length of stay extended between 7 and 19.1 days and attributable mortality reported as high as 24.6% to 35%.1-4
EPIDEMIOLOGY
The risk of developing device-related infection (either local or bacteremic) varies between ICUs and countries depending on the patient population, the type of device and its intended use, the microorganisms involved, and the patient-microbe-device interaction. The annual National Healthcare Safety Network in the US reports stratify CLABSIs per ICU type and representative incidence-density rates are shown from its most recent publication in Table 66-1.5 Representative rates from other types of catheters are also provided.6 The risk factors7,8 for device-associated infection that have been identified for the host, the microbe, the device, and the interactions among them are listed in Table 66-2.
Representative Rates for Intravascular Device-Associated Bacteremia
| Type of Device | Setting | Incidence Density Rate |
|---|---|---|
| Peripheral | ||
| Short-term, infusion lock | Med-surg wards | 0.5/1000 catheter-days |
| Midline | Med-surg wards | 0.2/1000 catheter-days |
| Arterial | Med-surg ICU | 1.7/1000 catheter-days |
| PICC | Out/inpatient | 1.0 -2.1/1000 catheter-days |
| Central | ||
| Non-cuffed venous (single- or multilumen) | Medical ICU | 2.0-2.6/1000 catheter-days |
| CCU | 2.0/1000 catheter-days | |
| Surgical ICU | 2.0-2.6/1000 catheter-days | |
| Trauma | 3.6/1000 catheter-days | |
| Pediatric ICU | 1.3-3.3/1000 catheter-days | |
| Burn units | 5.50/1000 catheter-days | |
| Cuffed venous (Hickman, Broviac) | Hematology-oncology wards | 1.7/1000 catheter-days |
Risk Factors for Device-Related Infection
| Patient-related factors |
| Age (age ≤1 year or ≥60 years) |
| Loss of skin integrity (burns) |
| Presence of neutropenia (absolute neutrophil count ≤1000) |
| Chemotherapy and radiotherapy |
| Distant focus of infection |
| Severity of underlying illness |
| Prolonged hospitalization before catheterization |
| Use of total parenteral nutrition |
| Device-related risk factors |
| Type of device material (steel, polyurethane, tetrafluoroethylene, and silicone more resistant to bacterial adherence than polyethylene and polyvinylchloride) |
| Frequency of surface irregularities |
| Thrombogenecity of catheter materials (predisposes to bacterial colonization) |
| Use of antibiotic- or antiseptic-impregnated catheters (reduces risk) |
| Microbe-related risk factors |
| Adherence properties (adherence to fibronectin or directly to polymer materials) |
| Biofilm formation (antiphagocytic and may potentiate pathogenecity by acting as a barrier to antimicrobial penetration) |
| Host-microbe–device interaction risk factors |
| Type of placement (cutdown higher risk than percutaneous) |
| Emergent placement (higher risk than elective placement) |
| Site of placement (femoral and jugular sites greater risk than subclavian site) |
| Duration of use (longer duration increases the risk) |
| Use of aseptic technique at the time of insertion (use of maximal barrier precautions—mask, sterile gown and gloves, and large drape—decreases risk) |
| Dense cutaneous colonization at device entry site (higher density of bacteria per unit area increases risk) |
| Dressing material (gauze dressing associated with lower risk for central lines) |
| Skill of puncturist (greater operator skill decreases risk) |
| Type of skin antiseptic used for insertion (alcoholic chlorhexidine preparations associated with less risk) |
| Use of topical antimicrobial ointment (may decrease risk) |
| Frequency of entry into the system (greater frequency of entry or excessive manipulation increases the risk) |
Of the many intravascular devices available, the peripheral venous catheter is by far the most commonly used. Most peripheral venous catheters currently are made of polyurethane or steel and are associated with a very low risk of bacteremia, with less than one episode of bacteremia per 500 devices.7,8 There is little difference currently in the risk of bacteremia regardless of whether polyurethane or steel needles are used if the same level of asepsis is applied at the time of placement.
Peripheral arterial catheters are in widespread use in ICUs for blood pressure monitoring and for obtaining arterial samples for blood gas determination. The incidence of bacteremia related to peripheral arterial devices is about 1.7/1000 catheter-days6,9 and the rate of significant colonization (≥15 colony-forming units [cfu] on semiquantitative culture) is about 5%.9,10 Insertion by cutdown, catheterization lasting 4 days or longer, and inflammation at the catheter exit site are associated with a higher risk of significant catheter colonization.
CVCs are estimated to account for over 90% of all catheter-related bacteremias. Prospective studies of noncuffed, short-term single or multilumen catheters inserted into either internal jugular or subclavian sites have found bacteremia rates of 1% to 5% and rates of significant colonization of the catheters (≥15 cfu on semiquantitative culture or ≥103cfu/mL on quantitative culture) ranging between 5% and 30%11-18 depending on the use and duration of the catheter plus the patient population. Peripherally inserted central catheters (PICCs) have lower catheter-related bacteremia rates, ranging between 1% and 2% but this depends on the inpatient versus outpatient setting.6,19 In the ICU setting, the risk of infection with PICCs is only marginally less than with CVCs placed in the subclavian or internal jugular veins.19 Many of the factors that may influence the risk of catheter colonization and/or catheter-related bacteremia are listed in Table 66-2. The presence of a distant focus of infection, bacteremia, tracheostomy, loss of skin integrity, emergent placement, internal jugular or femoral placement, absence of appropriate barrier precautions, transparent dressings, a high frequency of entry into the system, and multilumen catheters increase the risk of significant catheter colonization.1,12-15,18,20-27
The use of less than maximal barrier precautions, the use of 10% povidone-iodine or 70% alcohol alone as compared with alcoholic chlorhexidine as an antiseptic, the use of transparent dressings (in some but not all randomized studies), duration of catheterization of 4 days or more, and heavy cutaneous insertion-site colonization all have been associated with an increased risk of catheter-related bacteremia for central catheters.12-15,20,28-30 Factors that have been independently associated with CLABSI include prolonged hospitalization before catheterization, prolonged duration of catheterization, heavy microbial colonization at the catheter exit site or hub, use of the femoral or internal jugular sites, neutropenia, prematurity, use of total parenteral nutrition, or substandard care.31 In two separate systematic reviews, antibiotic-coated and first-generation antiseptic-impregnated CVCs have been demonstrated to reduce catheter colonization and bloodstream infection significantly.31-33 However, the effects have been modest and the methodologic quality of the studies was rated as poor and most of the studies were carried out before the widespread emphasis on infection control bundles for the care of central lines.33 In addition, another meta-analysis suggested that the benefit of the anti-infective catheters was time dependent and evident only during the first week after insertion.34 The use of chlorhexidine-impregnated sponge dressings has been advocated as an adjunct to reduce vascular catheter-related bloodstream infections but the results of two randomized controlled studies in the critical care setting are disparate, with one large and well-conducted study demonstrating a significant reduction in catheter-related infections and another smaller study that had low power demonstrating no difference.35,36 Neither study used alcoholic chlorhexidine-containing products as initial skin antisepsis prior to vascular catheter insertion, making it difficult to interpret what impact the chlorhexidine-impregnated sponge dressings would have in this setting.
Replacement of existing catheters over a guide wire is associated with a significantly lower rate of mechanical complications than replacement by insertion at a new site but more frequently results in infection of the newly placed catheter.37
Pulmonary arterial catheters (PACs), which are used in the management of hemodynamically unstable, critically ill patients, carry many of the same risk factors and rates of bacteremia as CVCs. Most PACs consist of a polyurethane catheter that passes through a percutaneous indwelling Teflon™ introducer sheath. Prospective studies have identified several risk factors associated with significant catheter colonization, including placement with less stringent barrier precautions, internal jugular vein placement, prolonged catheterization (≥4 days), and heavy microbial colonization at the catheter insertion site.20,38,39 Exposure of a PAC to bacteremia from a distant focus of infection, catheterization for 4 days or more, and difficulty with insertion also have been found to increase the risk of bacteremia. The incidence of bacteremia from PACs is about 1%.39
PATHOGENESIS
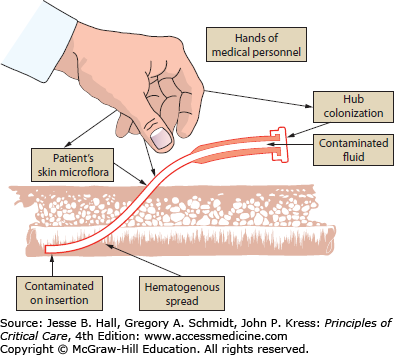
Microorganisms can gain entry (Fig. 66-1) to the intravascular device (usually an intravascular catheter) and the intravenous delivery system in several ways to cause device- or catheter-related bacteremia, including contamination of infusate, contamination of the catheter hub–infusion tubing junction, hematogenous seeding of the catheter tip, and colonization at the cutaneous catheter exit site.
Contamination of infusate may be intrinsic, occurring at the manufacturing level, or extrinsic, occurring via the administration sets, the extension tubing, the use of outdated intravenous solutions, or a break in aseptic technique allowing faulty admixtures. The potential for proliferation of organisms in various infusate fluids after intrinsic contamination has been well documented with strains of Klebsiella, Enterobacter, and Serratia.3,40,41Candida species have a propensity to grow in hypertonic glucose solutions used in parenteral solutions, and the commercially available lipid emulsions support the growth of most organisms.42 Nosocomial bacteremias secondary to contaminated infusate usually have occurred in epidemics or clusters but with improvement in manufacturing standards are now exceedingly rare. Extrinsic contamination of infusate causing central catheter–related bacteremia is also a very uncommon problem, with an estimated incidence of less than 1 per 1000 cannula-related septicemias. Most are reported in epidemics occurring as a result of the exposure to a common source of microbial contamination such as multidose vials, administration sets, or contaminated water-bath warmers. The risk of fluid becoming extrinsically contaminated is related to the duration of infusion through the administration set. Most hospitals now have policies that require replacement of the entire delivery system every 72 hours, which represents one of the most important control measures for reducing the complications of contaminated infusates. Similar to intrinsic contamination, hematogenous seeding of the catheter tip with consequent bacteremia is considered to be an uncommon event.
The majority of cannula-related bacteremias are thought to result from local endogenous microflora colonizing the skin at the insertion site and/or the transcutaneous wound7,29,43,44 that migrate along the subcutaneous tunnel, colonize the subcutaneous portion of the catheter, and then finally colonize the tip of the catheter. Another mechanism is colonization of the internal surface of the catheter hub, with subsequent colonization of the internal surface of the catheter and eventual colonization of the catheter tip.45-47 This colonization could occur as a result of obligate manipulations of the connection during tubing replacements or improper connection. After the hub has been contaminated, the microbes would be carried intraluminally, reach the catheter tip, and colonize the fibrin sheath. The origin of these microorganisms colonizing the hub is often the hands of those manipulating the hub rather than the flora of the patient’s skin. This latter mechanism of catheter tip colonization is considered an important contributor to intraluminal colonization of long-term catheters.45-47 Other routes of infection including hematogenous seeding from a distant focus of infection or, rarely, contaminated infusate are considered to be responsible for 5% or less of catheter-related infections.7
Studies of central-line infections (short indwelling insertion times) using molecular subtyping techniques to differentiate the different strains of infecting and colonizing organisms have demonstrated that approximately 80% of the microorganisms from distal catheter tips are concordant with organisms present on the skin at the catheter insertion site. The source of the remaining organisms was either contamination of the catheter hub, hematogenous colonization from remote sites, or unknown sources. Of episodes of catheter-related bacteremia, concordance of organisms at the catheter insertion site, the catheter tip, and the blood varied between 86% and 100%.
It also has been shown in several studies15
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree