Key Clinical Questions
What is the approach to an immunocompromised patient with suspected infection?
What are common infectious complications in patients receiving chronic corticosteroids, or recently treated with tumor necrosis factor inhibitors or rituximab?
Should preventative measures be taken to prevent infectious complications in patients taking these medications?
What infectious complications are common among patients who have undergone splenectomy?
How should a transplant patient presenting with possible infection be evaluated?
Introduction
With the advent of newer immunosuppressive medications and the rise in organ transplantation internationally, the numbers of immunocompromised patients are rising. The diagnosis and management of infection in this growing population is challenging. In immunocompromised patients, the usual signs and symptoms of infection may be obscured, and they often have a higher burden of pathogens and disseminated infection, leading to worse outcomes. These patients are also prone to infection with a broad array of less familiar pathogens, including opportunists such as Listeria monocytogenes and Pneumocystis jiroveci, and latent pathogens such as cytomegalovirus (CMV), toxoplasma, and Mycobacterium tuberculosis, as well as typical community-acquired and nosocomial microbes.
Guiding Principles
Two pieces of information are essential to the care of the patient with impaired immunity: the patient’s epidemiologic exposures and overall severity of immunosuppression.
The net state of immunosuppression is determined by the type, intensity, and duration of immunosuppression (including the dose and number of immunosuppressive agents or the presence of innate immunodeficiencies); anatomic factors causing a mechanical breakdown in the host defenses, such as abnormal lymphatic drainage at the site of previous surgery or radiation; and the presence or absence of immunosuppressive infections such as HIV or CMV.
Patients should be questioned about epidemiology that places them at risk for specific pathogens. These include recent events (sick contacts, animal exposure, travel, consumption of undercooked meat or unpasteurized dairy products), as well as remote residence in countries where tuberculosis is endemic, or regions of the United States where histoplasmosis, blastomycosis, or coccidioidomycosis are endemic.
Medication-Related Immunodeficiency
Dozens of medications, used in a wide variety of medical conditions, may impair immunologic function; an abbreviated list is shown in Table 198-1. Some agents, such as corticosteroids and alemtuzumab, undermine several layers of host defenses. Others have a more targeted effect, such as tacrolimus and cyclosporine, which prevent normal T lymphocyte responses to immunologic stimuli. Understanding the impact of medications on immunity helps to predict which infections the host may develop.
| Immunosuppressive Agent | Immunologic Effect | FDA-approved Uses |
|---|---|---|
| Corticosteroids | ||
| Prednisone, dexamethasone | Depletes circulating lymphocytes; suppresses phagocyte migration and function | Treatment of pulmonary and rheumatologic conditions |
| Antimetabolites | ||
| Methotrexate | Inhibits dihydrofolate reductase; impairs cellular replication and repair | Treatment of RA, psoriasis, ALL, and several solid organ malignancies |
| 6-mercaptopurine | Purine analogue; inhibits cellular DNA synthesis | Treatment of Crohn disease and ALL |
| Azathioprine | Disrupts purine metabolism | Treatment of RA; prevention of rejection in SOT |
| Mycophenolate mofetil | Inhibits inosine monophosphate dehydrogenase; inhibits B and T lymphocytes | Prevention of rejection in SOT |
| T lymphocyte active agents | ||
| Tacrolimus | Inhibits T lymphocyte activation | Prevention of rejection in SOT |
| Cyclosporine | Inhibits T lymphocyte activation | Prevention of rejection in SOT |
| Sirolimus | Suppresses cytokine induction of T lymphocyte activity | Prevention of rejection in SOT |
| Monoclonal antibodies | ||
| TNF-α inhibitors | Blocks effect of TNF-α, which mediates immunologic control of intracellular organisms and granuloma formation | Treatment of RA |
| Rituximab | Monoclonal antibody to CD20; depletes B lymphocytes | Treatment of lymphoma and RA |
| Natalizumab | Monoclonal antibody to alpha-4 integrins; interferes with leukocyte migration to areas of inflammation | Treatment of multiple sclerosis and Crohn disease |
| Alemtuzumab | Monoclonal antibody to CD52; depletes B and T lymphocytes | Treatment of CLL |
| Basiliximab | IL-2 receptor antagonist; prevents IL-2 mediated lymphocyte activation | Induction of immunosuppression in SOT |
| Daclizumab | IL-2 receptor antagonist; prevents IL-2 mediated lymphocyte activation | Induction of immunosuppression in SOT |
Corticosteroids are prescribed for rheumatologic conditions, inflammatory bowel disease, allergic disease, asthma, among others. The immediate impact of corticosteroids on host defenses includes depletion of circulating lymphocytes (particularly T lymphocytes) and monocytes, and suppression of phagocyte migration and function. Long-term effects that increase infection risk include impaired skin and soft tissue healing.
Corticosteroid use increases susceptibility to common bacterial infections (Table 198-2). Reactivation of latent tuberculosis is also increased among previously exposed patients started on corticosteroid therapy. Patients should be screened for latent tuberculosis before starting corticosteroid therapy. Chronic corticosteroid use also increases susceptibility to opportunistic infections. Infrequently, infection with invasive fungi such as Aspergillus and Fusarium occurs with chronic glucocorticoid use.
| Infection | Preventative Strategy |
|---|---|
| Bacterial infections | |
| Increased susceptibility to all bacterial infections | Vigilance; routine vaccinations (including influenza and pneumonia vaccines) |
| Mycobacterial infections | |
| Tuberculosis | Check purified protein derivative or interferon-gamma release assay prior to steroid initiation; treat if indicated |
| Fungal infections | |
| Pneumocystis jiroveci pneumonia | Prophylaxis when appropriate |
| Aspergillus | A rare complication |
| Fusarium | A rare complication |
| Parasitic infections | |
| Strongyloides hyperinfection syndrome | Screen with Strongyloides antibody before steroid initiation; treat if indicated |
Two infection syndromes associated with corticosteroid use deserve special mention: Pneumocystis jiroveci pneumonia (PCP) and Strongyloides hyperinfection syndrome.
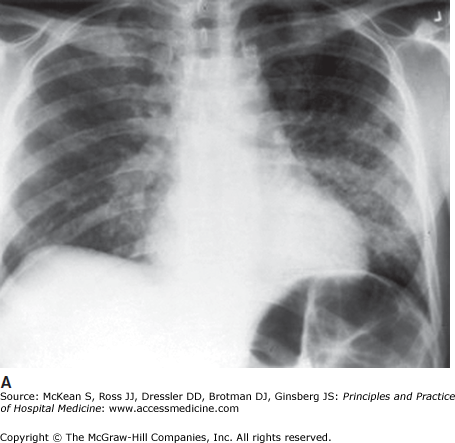
PCP is associated with prolonged corticosteroid use; the risk for PCP rises with increasing steroid dose and duration. Clinically, PCP causes fever, dyspnea, and dry cough. It is characterized radiographically by diffuse bilateral pulmonary infiltrates (Figure 198-1). Patients with PCP may be profoundly hypoxic, particularly with ambulation. The mortality associated with PCP infection in non HIV-infected patients is high—up to 50% in some case series. Therefore, suspected PCP should be treated empirically while the diagnostic work-up is ongoing.
Figure 198-1
Chest radiograph with diffuse interstitial infiltrates, and chest CT revealing ground glass infiltrates, in an HIV-positive patient with Pneumocystis carinii pneumonia (PCP). Radiographic findings in PCP may vary from impressive to quite subtle. (Reproduced, with permission, from Fauci AS, Braunwald E, Kasper DL, et al. Harrison’s Principles of Internal Medicine 17th ed. New York: McGraw-Hill 2008, Fig. 200-1.)
There are several methods of diagnosing PCP (Table 198-3). The gold standard is lung biopsy, with demonstration of characteristic cysts. More often, patients undergo bronchoscopy with bronchoalveolar lavage (BAL) or sputum induction, with testing of BAL fluid or sputum with direct fluorescent antigen or silver stain. A useful non-invasive test is the serum fungal marker beta-D-glucan, which may be very elevated in PCP, sometimes above the upper limit of the assay. (For the treatment of PCP in the non–HIV-infected population, see Practice Point.)
| Diagnostic Method | Advantage | Disadvantage |
|---|---|---|
| Lung biopsy | Gold standard for diagnosis | Invasive—requires transbronchial biopsy or surgical procedure |
| DFA of bronchoalveolar lavage fluid | Increase sensitivity compared to induced sputum | Requires invasive bronchoscopy |
| DFA of induced sputum | Less invasive than biopsy or bronchoalveolar lavage | Low burden of Pneumocystis in sputum leads to low sensitivity |
| Beta-D-glucan | Noninvasive; result characteristically greater than assay | Results often not rapidly available as it is usually a send-out test; false positive results possible in patients on hemodialysis, those who have received IVIg recently, or those with other invasive fungal infections |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree