CHAPTER 72
Infections
Veena Venugopalan, PharmD, BCPS-AQID • Levita K. Hidayat, PharmD
 LOWER-RESPIRATORY-TRACT INFECTIONS
LOWER-RESPIRATORY-TRACT INFECTIONS
The term lower-respiratory-tract infections (LRTIs) encompass a broad range of disease states, including acute bronchitis, pneumonia, and exacerbations of chronic lung disease. There is significant overlap in the presentation of these different disease states; therefore, familiarity with the categories of lower-respiratory infection and their management is crucial to providing good primary care.
This chapter focuses on the following disease states:
 Acute bronchitis, an acute inflammation of the tracheobronchial tree, is diagnosed by exclusion. Clinically it is characterized by the presence of either a productive or nonproductive cough of 4 to 6 weeks’ duration. Chronic bronchitis is part of the spectrum of chronic obstructive pulmonary disease (see Chapter 71).
Acute bronchitis, an acute inflammation of the tracheobronchial tree, is diagnosed by exclusion. Clinically it is characterized by the presence of either a productive or nonproductive cough of 4 to 6 weeks’ duration. Chronic bronchitis is part of the spectrum of chronic obstructive pulmonary disease (see Chapter 71).
 Pneumonia is an infection of the distal portion of the lungs, involving the respiratory bronchioles, alveolar ducts, sacs, and alveoli.
Pneumonia is an infection of the distal portion of the lungs, involving the respiratory bronchioles, alveolar ducts, sacs, and alveoli.
 ANATOMY, PHYSIOLOGY, AND PATHOLOGY
ANATOMY, PHYSIOLOGY, AND PATHOLOGY
The trachea and bronchi are made of a rich epithelial cell surface composed of ciliated cells, secretory goblet cells, subepithelial cells (containing cartilage for structural support of the airways), and inflammatory mediator cells and glands. The amount of cartilage decreases as the respiratory tree branches distally and disappears altogether in the small airways (<2 mm in diameter). Tracheobronchial glands, which secrete mucus, are bigger and more numerous in the proximal airways.
Cells dedicated to airway defense are found scattered within the epithelium and submucosa. Lymphocytes may appear singly or in clusters, especially at branching points or airway bifurcations, and are called bronchus-associated lymphoid tissue. Plasma cells, especially immunoglobulin A (IgA), mast cells, and macrophages, are also found at airway bifurcations. Mast cells increase in the transition zone leading to the distal airway, where gas conduction occurs. Marked branching of the airways continues as surface area is maximized for gas exchange. This architecture helps to keep the area below the main carina sterile.
Although the lower respiratory tract is uniquely equipped to protect against invading organisms, failure of these defenses and presence of predisposing factors increase the risk of infection in the host. These factors include: (1) alteration of the normal oropharyngeal flora, (2) depressed cough and glottis reflexes, (3) altered consciousness, (4) impaired mucociliary apparatus mechanism, (5) alveolar macrophage dysfunction, and (6) immune dysfunction (Singh, 2012).
Aspiration of upper-airway flora is the most important risk for infection. Defense mechanisms include a good cough reflex; effective mucociliary clearance (continual upward beating of cilia) to remove bacteria and debris; and angulation of airways, which traps and impinges bacteria at bifurcations. For infection to occur, the following sequential steps are required, especially for oropharyngeal colonization: aspiration of organisms; bacterial attachment to epithelial cell surfaces, preventing normal epithelial cell desquamation; and subsequent removal by expectoration.
The risk of lower-airway infection is further increased by both the type of oral microflora present in the airways and host susceptibility. Severely ill patients lose their normal flora and become increasingly susceptible to enteric gram-negative bacilli. Clearance mechanisms progressively malfunction and are associated with abnormalities in mucosal surfaces. A recent viral infection may effectively strip the normal mucosa, causing intense cellular desquamation and loss of mucociliary function and local phagocytic function.
Within the terminal airway, the alveolar macrophage is the primary cellular defense. Alveolar macrophages are capable of overwhelming a challenge of low virulence—for instance, a normal, nocturnal, small-volume aspiration of oropharyngeal secretions. Activated alveolar macrophages also are capable of activating the immune system by recruiting polymorphonuclear leukocytes, found in pulmonary microvasculature reserves.
In addition, alveolar macrophages secrete cytokines, which trigger the intercellular communication systems of the immunologic response. Important lung cytokines include tumor necrosis factor, interleukin 1, and interleukin 8. They are produced in response to alveolar macrophages that activate mononuclear cells to release gamma colony stimulating factor (G-CSF). G-CSF increases myeloid progenitor cells, which trigger polymorphonuclear leukocytes to promote adhesion, chemotaxis, phagocytosis, and phosphorylation at local sites to combat infection.
 ACUTE BRONCHITIS
ACUTE BRONCHITIS
Epidemiology
In 2010, cough was among the 10 most common reasons for seeking medical attention, resulting in >30 million physician office visits (www.cdc.gov).
Etiology
The causative pathogen in acute bronchitis is identified in 16% to 40% of cases (Gonzales et al., 2001). Approximately 90% of acute bronchitis infections are caused by viruses, the most common being influenza B, influenza A, parainfluenza, and respiratory synctival virus. While respiratory syncytial virus causes asymptomatic or mild symptomatic disease in young and middle-aged adults, in elderly persons (>60 years) it leads to symptomatic lower-respiratory-tract disease.
To date, only Bordetella pertussis, Mycoplasma pneumoniae, and Chlamydia pneumoniae have been established as the nonviral causes of uncomplicated bronchitis in adults. As a group, these agents are associated with 5% to 10% of all cases of uncomplicated acute bronchitis in adults and are recovered more frequently in adults with chronic or persistent cough.
Diagnostic Criteria
Acute bronchitis should be differentiated from asthma or bronchiolitis and bronchiectasis. Asthma or br onchiolitis results from the acute inflammation of the small airways and typically presents as progressive cough accompanied by wheezing, tachypnea, respiratory distress, and hypoxemia (Wenzel & Fowler, 2006). Bronchiectesis, however, is commonly associated with the permanent dilatation of bronchi and chronic cough. While cough after acute bronchitis typically persists for 10 to 20 days and may occasionally last for 4 or more weeks, a diagnosis of chronic bronchitis is reserved for patients who have cough and sputum production on most days of the month for at least 3 months of the year during 2 consecutive years.
When making the diagnosis of acute bronchitis, a careful history, which includes any reports of sick contacts, and physical examination are necessary. A common presentation of pertussis is cough of 2 to 3 weeks’ duration in an adolescent or young adult. Fever as a symptom is less common in pertussis than in viral bronchitis.
History and Physical Examinaton
Upon physical examination, the presence of cough in the absence of fever, tachycardia, and tachypnea suggests bronchitis rather than pneumonia. Also, the presence of normal vital signs and the absence of rales and egophony on chest examination minimize the likelihood of pneumonia. An exception is cough associated with pneumonia in elderly patients, which is often characterized by the absence of distinctive signs and symptoms (Wenzel & Fowler, 2006).
Diagnostic Studies
The definitive laboratory diagnosis of an upper-respiratory viral infection causing acute bronchitis is unnecessary. Chest x-rays should be obtained in all patients who appear ill to exclude a more serious lower-respiratory infection.
Rapid diagnostic tests exist for several pathogens currently linked to acute bronchitis. However, not all tests are widely available, and their routine use is not practical or cost effective in the outpatient setting.
Treatment Options, Expected Outcomes, and Comprehensive Management
There are two strategies for the treatment of acute bronchitis: (1) antibiotic therapy, and (2) symptom management.
ANTIBIOTICS
Most reports have shown that 65% and 80% of patients with acute bronchitis receive an antibiotic despite the majority of evidence suggesting that they are ineffective (Braman, 2006). Elderly patients are particularly likely to receive unnecessary antibiotics, and more than one-half of prescriptions are for extended-spectrum antibiotics. This increased use of antibiotics is a major concern due to the risk of antibiotic resistance and of Clostridium difficile infection in the community.
The American College of Chest Physicians (ACCP) does not recommend routine antibiotics for patients with acute bronchitis. Clinical data support that antibiotics do not significantly impact the duration or severity of acute bronchitis or potential complications such as the development of pneumonia.
Clinical Pearls
 Because many patients with acute bronchitis expect to receive an antibiotic, the ACCP guidelines recommend that office or clinic time be set aside to explain the decision not to use these agents, and the potential harm of using unnecessary antibiotics to the individual and the community at large (Braman, 2006).
Because many patients with acute bronchitis expect to receive an antibiotic, the ACCP guidelines recommend that office or clinic time be set aside to explain the decision not to use these agents, and the potential harm of using unnecessary antibiotics to the individual and the community at large (Braman, 2006).
Treatment for acute bronchitis is symptomatic: acetaminophen, oral liquids, and bed rest are encouraged when malaise and fever are prominent.
Dextromethorphan (15 mg orally every 4 to 6 hours) will suppress a nonproductive cough. The literature supporting the efficacy of antitussive treatments may be difficult to interpret because the benefit appears to depend on the cause of cough illness. Acute or early cough due to colds or other viral upper-respiratory-tract infections does not appear to respond to dextromethorphan or codeine, whereas chronic cough (duration >3 weeks) associated with underlying lung disease seems to respond to these agents.
Although the ACCP does not recommend use of inhaled β2-agonists to alleviate cough, such an agent may be prescribed when wheezing is present. The effect of orally inhaled anticholinergic agents on the cough of acute bronchitis has not been studied and therefore cannot be recommended based on the evidence. Additionally, the guidelines do not recommend the use of mucolytics for the treatment of acute bronchitis due to lack of consistent favorable effect.
 COMMUNITY-ACQUIRED PNEUMONIA
COMMUNITY-ACQUIRED PNEUMONIA
Epidemiology
Community-acquired pneumonia (CAP) is a major health problem in the United States and is associated with substantial morbidity and mortality and health care costs. Pneumonia accounted for approximately 4.5 million ambulatory care visits in 2007 in the United States, about one third of which took place in hospital emergency departments. The risk of pneumonia increases markedly with age, with approximately 1 million episodes of CAP and more than 600,000 hospitalizations for pneumonia occurring in adults 65 years of age and older. Pneumonia is an important cause of death overall in the United States and the leading cause of death from infection (Moran, Rothman, & Volturo, 2013).
Etiology
Community-acquired bacterial pneumonia (CABP) is an acute bacterial infection of the pulmonary parenchyma in adults. It is associated with specific symptoms such as fever or hypothermia, chills, rigors, cough, chest pain, or dyspnea and is accompanied by a new lobar or multilobar infiltrate on a chest radiograph.
The most common bacterial pathogens associated with CABP include Streptococcus pneumoniae, Haemophilus influenza, Staphylococcus aureus, and Moraxella catarrhalis. The resistance pattern for S. pneumoniae and S. aureus has greatly changed over the past years and this should be considered in the selection of an appropriate antimicrobial regimen.
In 2007, the Centers for Disease Control and Prevention reported that 74.4% of S. pneumoniae isolates were susceptible to penicillin. Increasing S. pneumoniae resistance to macrolides is particularly concerning, with rates in 2006 exceeding 35% nationally. The prevalence of fluoroquinolone resistance was approximately 2% in 2009. Although introduction of the 7-valent pneumococcal conjugate vaccine in 2000 led to a decline in invasive infections caused by S. pneumoniae, such as CAP, among children and adults, it caused an increase in nonvaccine serotypes and produced a shift in S. pneumoniae resistance patterns. A 13-valent pneumococcal vaccine was introduced in 2010, which includes both the serotypes in the 7-valent vaccine and those that have emerged since its introduction. Continued use of this vaccine will likely shift the prevalence of S. pneumoniae serotypes, and a shift in resistance patterns may appear again. Continued surveillance to recognize these changes will be necessary.
Until recently, S. aureus was considered an uncommon cause of CAP, accounting for 1% to 5% of all cases. Previously thought of as a nosocomial pathogen, methicillin-resistant S. aureus (MRSA) has become the predominant cause of acute bacterial skin and skin structure infections in the community setting. Community-acquired MRSA (CA-MRSA) is now not only a common cause of skin infections but is increasingly being implicated in CAP. Pneumonia caused by MRSA is now recognized as an emerging clinical entity with distinctive clinical features and substantial morbidity and mortality.
The “atypical” organisms, so called because they are not detectable on Gram stain or cultivatable on standard bacteriologic media, include M. pneumoniae, C. pneumoniae, Legionella species, and respiratory viruses. With the exception of Legionella species, these organisms commonly cause pneumonia in outpatients. Also, in atypical pneumonia, systemic symptoms predominate (e.g., fever, headache, myalgias, dry or minimally productive cough, and lack of clinical signs of consolidation).
Diagnostic Criteria
SITE-OF-CARE DECISIONS
Almost all decisions regarding diagnosis and treatment of CAP involve the initial severity-of-illness assessment. Severity-of-illness tools have been validated for use in deciding outpatient versus inpatient treatment and to further determine the need for ICU admission.
SEVERITY-OF-ILLNESS TOOLS
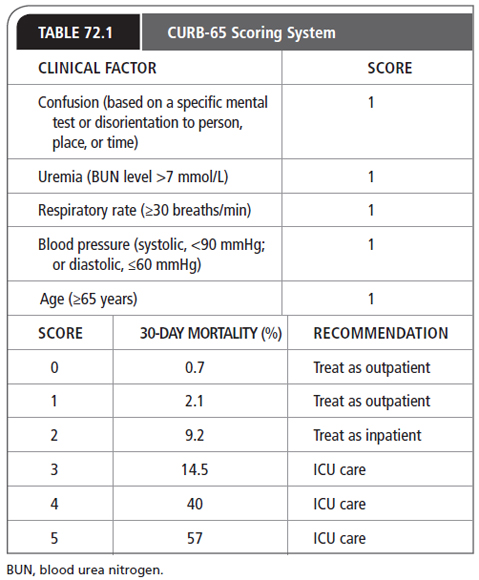
The two most widely used severity assessment tools in CAP are the Pneumonia Patient Research Team (PORT) system (also referred to as the Pneumonia Severity Index) and the confusion, uremia, respiratory rate, blood pressure, and age ≥65 years (CURB-65; Table 72.1). The PORT severity assessment tool is based on 19 variables, including clinical, laboratory, and demographic characteristics, whereas the CURB-65 relies on five factors. Although studies have revealed that both PORT and CURB-65 predicted 30-day mortality with no significant difference, the CURB-65 tool may be simpler and less cumbersome to use. A CURB-65 score of 0 to 1 suggests that a CAP patient can be treated as an outpatient, a score of two requires hospitalization, and patients with a score of ≥3 often require ICU care.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree