CHAPTER 142
Impalement Injuries, Minor
Presentation
A sharp metal object, such as a needle, heavy wire, nail, or fork, is driven into or through a patient’s extremity. In some instances, often because prehospital care providers have been trained to leave impaled objects in place, the patient may arrive with an additional large object attached; for instance, a child who has stepped on a nail going through a board (Figure 142-1). As minor as most of these injuries are, they tend to create a spectacle and draw a crowd; this is especially true when the impaled objects are two TASER darts lodged in a handcuffed prisoner.
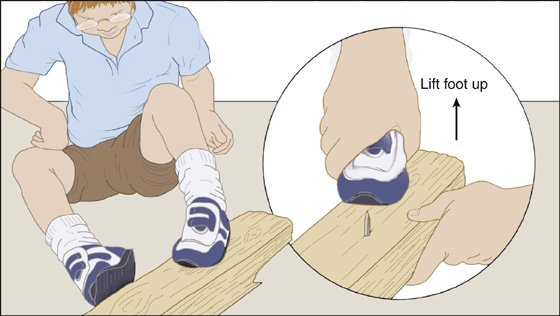
Figure 142-1 Foot stuck to nail with rapid removal.
What To Do:
 If the patient arrives with an impaled object attached to something that is acting like a lever and causing pain with any movement, either quickly cut off this lever or, when the object is known to be smooth and straight, immediately pull the patient’s extremity off the sharp object. (An exposed nail or metal spike can usually be cut with an orthopedic pin cutter [Figure 142-2].)
If the patient arrives with an impaled object attached to something that is acting like a lever and causing pain with any movement, either quickly cut off this lever or, when the object is known to be smooth and straight, immediately pull the patient’s extremity off the sharp object. (An exposed nail or metal spike can usually be cut with an orthopedic pin cutter [Figure 142-2].)
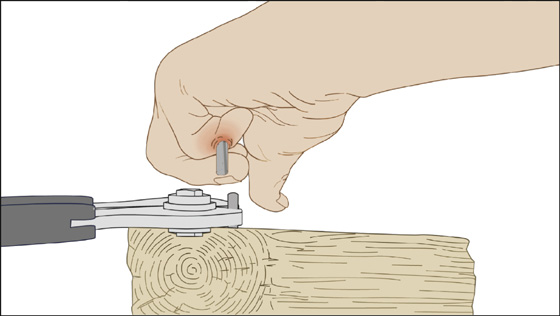
Figure 142-2 Cut an exposed nail with an orthopedic pin cutter.
 Obtain radiographs when pain and further damage from a leveraged object are not problems and when there is suspicion of an underlying fracture (as might occur with a nail gun) or fragmentation or hooking of the impaled object (as might occur with a heavy wire that has been thrown from under a lawnmower). When radiographs are necessary in the face of a painful mobile impaled object, fully immobilize and secure the object before moving the patient, thereby preventing further pain or injury. Administer analgesics as appropriate for pain, especially for pain anticipated during evaluation of the object during radiography.
Obtain radiographs when pain and further damage from a leveraged object are not problems and when there is suspicion of an underlying fracture (as might occur with a nail gun) or fragmentation or hooking of the impaled object (as might occur with a heavy wire that has been thrown from under a lawnmower). When radiographs are necessary in the face of a painful mobile impaled object, fully immobilize and secure the object before moving the patient, thereby preventing further pain or injury. Administer analgesics as appropriate for pain, especially for pain anticipated during evaluation of the object during radiography.
 It is not necessary to radiograph a penetrating nail, fork, or other nonmalleable, nonfragile object that will remain intact under the skin and is easily removed, regardless of its radiographic appearance. Radiographs offer little useful information regarding joint or tendon involvement, nor do they, in most instances, give any additional information that is not evident on clinical examination. If a puncture-type fracture is suspected, a radiograph will be more revealing if it is taken after the foreign body has been removed.
It is not necessary to radiograph a penetrating nail, fork, or other nonmalleable, nonfragile object that will remain intact under the skin and is easily removed, regardless of its radiographic appearance. Radiographs offer little useful information regarding joint or tendon involvement, nor do they, in most instances, give any additional information that is not evident on clinical examination. If a puncture-type fracture is suspected, a radiograph will be more revealing if it is taken after the foreign body has been removed.
 Examine the extremity for possible neurovascular or tendon injury.
Examine the extremity for possible neurovascular or tendon injury.
 Cleanse the object and puncture wounds with a povidone-iodine solution or equivalent antiseptic.
Cleanse the object and puncture wounds with a povidone-iodine solution or equivalent antiseptic.

 Rapid removal using sudden forceful traction on firmly embedded smooth, straight objects (e.g., fork, nail, or letter spike) is generally the most appropriate method for taking out these objects.
Rapid removal using sudden forceful traction on firmly embedded smooth, straight objects (e.g., fork, nail, or letter spike) is generally the most appropriate method for taking out these objects.
 If surgical débridement is anticipated after removal of the object, infiltration of an anesthetic should be provided before removal. Otherwise, patient preference should determine whether or not a local anesthetic is used. Local anesthesia will usually not give complete pain relief when a deeply embedded object is removed; inform the patient of this.
If surgical débridement is anticipated after removal of the object, infiltration of an anesthetic should be provided before removal. Otherwise, patient preference should determine whether or not a local anesthetic is used. Local anesthesia will usually not give complete pain relief when a deeply embedded object is removed; inform the patient of this.
 Contaminated objects that track superficially under the dermis may be released using the same techniques described in Chapter 153.
Contaminated objects that track superficially under the dermis may be released using the same techniques described in Chapter 153.
 Objects with small barbs, such as crochet needles, fish spines, and TASER darts, can be removed by first anesthetizing the area and then applying firm traction until the barb is revealed through the puncture wound. The fibrils of connective tissue caught over the barb can then be cut with a No. 11 scalpel blade or fine scissors. To provide better exposure, the entrance wound can be enlarged using the No. 11 blade.
Objects with small barbs, such as crochet needles, fish spines, and TASER darts, can be removed by first anesthetizing the area and then applying firm traction until the barb is revealed through the puncture wound. The fibrils of connective tissue caught over the barb can then be cut with a No. 11 scalpel blade or fine scissors. To provide better exposure, the entrance wound can be enlarged using the No. 11 blade.
 Most prehospital care services have protocols for removing low-risk TASER darts in the field, because the longest No. 9 barb is less than 1/4 inch in length. Use caution and appropriate consultation, however, when confronted with TASER darts lodged in the eye, ear, mouth, neck, groin/perineum, and female breast, and with any injury associated with apparent vascular or neurologic injury.
Most prehospital care services have protocols for removing low-risk TASER darts in the field, because the longest No. 9 barb is less than 1/4 inch in length. Use caution and appropriate consultation, however, when confronted with TASER darts lodged in the eye, ear, mouth, neck, groin/perineum, and female breast, and with any injury associated with apparent vascular or neurologic injury.
 After removal of the impaled object, the wound should be appropriately débrided and irrigated as described for puncture wounds (see Chapter 151). Tetanus prophylaxis should be provided (see Appendix H), and, except for contaminated wounds, such as a fish spine, prophylactic antibiotics should not routinely be prescribed. The decision to use antimicrobials should be individualized for each patient based on his general health and the nature of the impaled object (e.g., clean vs. grossly contaminated) as well as the location of the injury (e.g., deep vs. superficial, possible joint or tendon involvement, and highly contaminated punctures of the foot). A 3- to 5-day course of an antibiotic effective against Staphylococcus and Streptococcus species should be provided when appropriate.
After removal of the impaled object, the wound should be appropriately débrided and irrigated as described for puncture wounds (see Chapter 151). Tetanus prophylaxis should be provided (see Appendix H), and, except for contaminated wounds, such as a fish spine, prophylactic antibiotics should not routinely be prescribed. The decision to use antimicrobials should be individualized for each patient based on his general health and the nature of the impaled object (e.g., clean vs. grossly contaminated) as well as the location of the injury (e.g., deep vs. superficial, possible joint or tendon involvement, and highly contaminated punctures of the foot). A 3- to 5-day course of an antibiotic effective against Staphylococcus and Streptococcus species should be provided when appropriate.
What Not To Do:
 Do not send a patient for a radiograph with a leveraged object impaled, thus creating further pain and possible injury with every movement. When radiographs are necessary, fully immobilize these objects.
Do not send a patient for a radiograph with a leveraged object impaled, thus creating further pain and possible injury with every movement. When radiographs are necessary, fully immobilize these objects.
 Do not try to hand saw a board attached to an impaled object. The resultant movement will obviously cause unnecessary pain and possibly harm.
Do not try to hand saw a board attached to an impaled object. The resultant movement will obviously cause unnecessary pain and possibly harm.
 Do not confuse minor impalement injuries of the distal extremities with major impalement injuries where major blood vessels may be involved. Patients can rapidly exsanguinate from these wounds if the impaled object is removed prematurely.
Do not confuse minor impalement injuries of the distal extremities with major impalement injuries where major blood vessels may be involved. Patients can rapidly exsanguinate from these wounds if the impaled object is removed prematurely.
Discussion
Simple impalement injuries of the distal extremities should not be confused with major impalement injuries of the neck and trunk, groin, or buttock, from which the foreign object should not be precipitously removed. With major impalement injuries, careful localization with radiographs is required, and full exposure and vascular control in the operating room are also necessary to prevent rapid exsanguination when the impaled object is removed from the heart or a great vessel. Large impalement injuries of the extremities (especially of the groin, thigh, and axilla) also require immediate surgical consultation and thorough consideration of potential neurovascular and musculoskeletal injuries.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


