30 Ilioinguinal and Iliohypogastric Neural Blockade
Clinically Relevant Anatomy
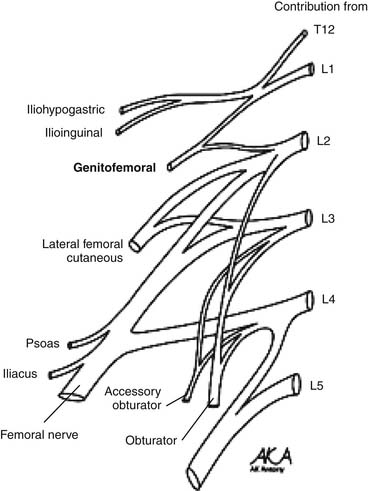
The ilioinguinal and iliohypogastric nerves are branches of the lumbar plexus originating from the ventral ramus of L1 with occasional contributing fibers from T12 (Fig. 30-1). They emerge from the superolateral border of the psoas major muscle, course posterior to the medial arcuate ligaments, and anterolateral to the quadratus lumborum. Above the anterior superior iliac spine (ASIS), they pierce the transverse abdominal muscle or transversus abdominus.1,2
The iliohypogastric nerve continues between the transversus abdominis and internal oblique, dividing into lateral and anterior cutaneous branches. The lateral cutaneous branch perforates the internal and external oblique muscle above the iliac crest and innervates the posterolateral gluteal skin. The anterior cutaneous branch runs medial to the anterior superior iliac spine, perforating the external oblique aponeurosis above the superficial inguinal ring and innervating the suprapubic skin.1,2
The ilioinguinal nerve travels through the internal oblique muscle, traversing the inguinal canal below the spermatic cord. It exits through the superficial inguinal ring to innervate the proximal medial skin of the thigh. In males, it innervates the skin over the penile root and the upper scrotum. In females, it innervates the skin covering the mons pubis and the adjoining labia majora.1,2 The iliohypogastric and ilioinguinal nerves occasionally interconnect along their courses, resulting in variations in the dermatomal distribution.3
Etiology and Pathogenesis
The vast majority of ilioinguinal and iliohypogastric neuralgias are iatrogenic. In 1942, Magee first described ilioinguinal and iliohypogastric neuralgias in scientific literature.4 Since then, a variety of etiologies have been detailed. Ilioinguinal and iliohypogastric neuropathies have been associated with a variety of lower abdominal surgeries.5 They may be the result of entrapment from sutures or staples, or result from adhesions, scarring, or inflammation. Neuroma formation, resulting from electrocauterization or laceration during open/laparoscopic procedures, may also contribute to this process.
Ilioinguinal and iliohypogastric neuralgias have been reported after various surgical procedures such as inguinal herniorrhaphy, appendectomy, abdominoplasty, needle bladder suspension, and iliac crest bone harvesting.6–9 A variety of obstetric surgical interventions such as total abdominal hysterectomy, pelvic lymphadenectomy, bilateral salpingo-oophorectomy, and other procedures involving Pfannenstiel incisions have also been associated with ilioinguinal and iliohypogastric neuralgias.10–13
The pathogenesis of these neuralgias depends on the etiology. In the case of entrapment, chronic compression may result in demyelination and axonal damage. A build-up of connective tissue in the endoneurium and perineurium may cause nerve thickening distal to the site of entrapment. In turn, this may affect the vascular supply through the vasa nervorum as well as axonal transport; ultimately disrupting neural function. Impulse generation and conduction may be affected causing symptoms.14 Neuroma formation may result from a transection of the nerve. When this occurs, the resulting axonal ends may continue to grow in a disorganized fashion. This, in turn, may result in a bulbous collection of unmyelinated fibers. These neuromas are far more mechanosensitive and thermosensitive than normal nerve endings and may produce spontaneous discharges resulting in neuropathy.15
Indications
Ilioinguinal and iliohypogastric nerve blocks are used as a diagnostic and therapeutic tool in the management of ilioinguinal and iliohypogastric neuropathies. They are used to determine true neuropathy, discriminate peripheral nerve pathology from radiculopathy, as well as to treat both chronic and acute groin pain. In addition, they may help to predict the outcome of permanent corrections such as neurectomy and neurolysis.
In combination with pharmacologic management, ilioinguinal and iliohypogastric blocks have been used to provide analgesia following surgeries such as inguinal herniorrhaphies, cesarean sections, orchiopexy, and total abdominal hysterectomies.16–19 In patients with chronic groin pain resulting from neuralgia, ilioinguinal and iliohypogastric nerve blocks have provided analgesia following failure of more conservative therapies.20
Technique
The first technique described relies on anatomic landmarks; the nerves are typically blocked 2 cm medial and superior to the anterior superior iliac spine (Fig. 30-2) along a line connecting the ASIS and the umbilicus. Here, the needle is inserted perpendicularly to the skin, noting penetration of each muscle fascial layer. Local anesthetic (10 mL with corticosteroid agent—typically methylprednisolone or triamcinolone 40 to 80 mg) is applied.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree