KEY POINTS
ICU-acquired weakness designates clinically detected weakness in critically ill patients in whom there is no plausible etiology other than critical illness. Patients can be labeled with this diagnosis with a suggestive history and when they can participate in a comprehensive bedside neuromuscular examination.
Electrophysiology testing, direct muscle stimulation, and biopsy may be necessary to characterize neuromuscular injury in the patient who is unable to participate in a comprehensive neuromuscular examination, is failing to improve function despite weeks of therapy, or for the patient with asymmetric weakness.
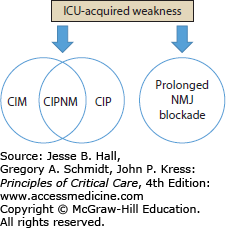
When conducted, advanced testing, particularly electrophysiology tests, can characterize the specific phenotype of ICU-AW including critical illness polyneuropathy, critical illness myopathy, a combination of the two (polyneuromyopathy), or prolonged neuromuscular blockade.
The exact epidemiology of ICUAW is unknown. Studies show that 46% of patients with sepsis, multiorgan failure, or prolonged mechanical ventilation are diagnosed with ICUAW. In patients undergoing mechanical ventilation for 7 days or more, 25% develop ICUAW.
Factors associated with the diagnosis of ICUAW include the presence of multisystem organ dysfunction, sepsis, SIRS, and hyperglycemia and the duration of mechanical ventilation. The only known therapy to prevent ICUAW has been strict glycemic control with insulin; however, adverse events with this therapy have prevented its utilization.
INTRODUCTION
Many patients admitted to the intensive care unit (ICU) develop a syndrome of neuromuscular dysfunction characterized by generalized muscle weakness and an inability to be liberated from mechanical ventilation. Since this syndrome occurs in the absence of preexisting neuromuscular disease, it is believed to reflect illnesses or treatments occurring in the ICU. Early reports described two categories of acute, acquired neuromuscular dysfunction: polyneuropathy (during sepsis and multisystem organ failure)1,2 and myopathy (particularly in patients with acute respiratory failure who received glucocorticoids and/or neuromuscular blocking agents).3,4 Decades of research on this acquired nerve and muscle injury has characterized specific phenotypes via comprehensive physical examination, electrophysiologic testing, and histopathology. Overall, the spectrum of neuromuscular disorders acquired in the ICU is now collectively referred to as “ICU-acquired weakness” (ICUAW) (Fig. 83-1).5
The rising incidence and societal burden of critical illness—such as sepsis and the acute respiratory distress syndrome6-8—coupled with declining case fatality rates and an aging population,9,10 suggests that the number of patients with ICUAW and its sequelae may be substantial and likely to grow. Accordingly, intensivists must have familiarity with the presentation of ICUAW, recognize when to conduct advanced testing, and understand the diagnostic tests involved. Although currently limited in scope, measures designed to prevent or attenuate ICUAW must be considered and implemented.
CRITICAL CARE SURVIVORSHIP AND ICUAW
Critical care outcomes research has demonstrated substantial morbidity in survivors. Injuries include general deconditioning, muscle weakness, dyspnea, depression, anxiety, and reduced health-related quality of life.11 One widely cited catalyst for attention to the burden of neuromuscular weakness was the comprehensive observations of a cohort of survivors of acute respiratory distress syndrome (ARDS) published in 2003.12 These 109 survivors were young (median age, 45 years), had few pre-existing comorbidities, and were severely ill (median APACHE II score, 23). Their critical illness was marked by prolonged mechanical ventilation (median duration, 21 days) and ICU and hospital lengths of stay (median duration, 25 and 48 days, respectively). Despite severe acute lung injury, serial follow-up examination during the first year after ICU discharge demonstrated restoration of lung function. Lung volumes and spirometry normalized by 6 months and carbon monoxide diffusion capacity improved to 72% predicted at 12 months. In contrast, all 109 patients reported poor function attributed to the loss of muscle bulk, proximal weakness, and fatigue. One year after ICU discharge, the median distance walked in 6 minutes was 66% of predicted and only 49% of patients had returned to work.
More recently, the same cohort was characterized at 5 years after ICU discharge.13 All patients reported subjective weakness and decreased exercise capacity when compared to function before ICU admission. Although there was no evidence of clinical weakness on examination, the median distance walked in 6 minutes remained lower than expected based on age and sex (76% predicted). By the fifth year, 77% of patients had returned to work; however, patients often required a modified work schedule, gradual transition back to work, or job retraining. In addition, patients were plagued with the psychological ramifications of their severe illness; more than half of survivors experienced at least one episode of physician-confirmed depression or anxiety.
Others have reported similar findings of post-ARDS debilitation. Specifically, an observational trial of 112 ARDS survivors without baseline impaired physical function noted a 66% cumulative incidence of physical impairment during 2 year follow-up.14 This impairment, defined as the acquisition of two or more dependencies in instrumental activities of daily living, had greatest incidence by 3 months after discharge and was associated with longer ICU stay and prior depressive symptoms. More recently, a comprehensive 1 year follow-up of patients enrolled in a randomized controlled trial of nutritional strategies in patient with ARDS demonstrated that survivors, regardless of nutritional strategy, experienced substantial impairments in endurance (as defined by six minute walk test) and cognitive function.15
Acquired neuromuscular weakness and loss of function have been measured in other contexts of critical illness, including severe sepsis and mechanical ventilation in the elderly. To determine the impact of a hospitalization for severe sepsis, Iwashyna and colleagues utilized The Health and Retirement Study, a cohort of Americans over age 50 undergoing biennial surveys of physical and cognitive function.16 Participants were stratified into those surviving a hospitalization for severe sepsis (n = 516) versus controls (survivors of a nonsepsis hospitalization, n = 4517). Among patients with no functional limitations at baseline, severe sepsis was associated with the development of 1.57 new limitations (95% CI: 0.99-2.15), as well as a more rapid rate of development of functional limitations after hospitalization (0.51 new limitations per year, p = 0.007 compared with baseline). The study also found that the incidence of severe sepsis was highly associated with progression to moderate to severe cognitive impairment.
In a similar design, Barnato et al used a longitudinal cohort study of Medicare recipients to investigate the association of mechanical ventilation and disability.17 Community dwelling patients over age 65 completed quarterly interviews of physical function for four years. Survivors of hospitalization with or without mechanical ventilation had similar levels of disability from each other, but significantly more than those who were never hospitalized. There was a substantial increase in disability in both groups after hospitalization, greater among survivors of mechanical ventilation than in those hospitalized without mechanical ventilation. In adjusted analyses, mechanical ventilation was associated with a 30% greater disability in activities of daily living (ADLs) and a 14% greater disability in mobility.
These studies show that decrements in physical function occur across the spectrum of critical illness. Although these outcomes may be influenced by other factors—such as age, preexisting comorbidities, acquired psychological and cognitive dysfunction, and social support—it is clear that ICUAW needs to be recognized early to enable preventive interventions. However, the recognition of ICUAW has often been hindered by challenges with various diagnostic testing approaches and complex nomenclature.
CLINICAL PRESENTATION OF ICUAW
The clinical approach is based on the recognition of generalized weakness in the appropriate setting, the exclusion of causes extrinsic to critical illness, and the measurement of muscle strength.5 The historian should carefully review the time course of neuromuscular symptoms as they relate to the underlying critical illness. Potential risk factors for ICUAW should be identified—including sepsis, multiple organ failure, mechanical ventilation, hyperglycemia, and exposure to pharmacologic agents like glucocorticoids and neuromuscular blocking agents (NMBAs). Neurologic examination evaluates key functional domains including consciousness, cognitive function, cranial nerves, motor and sensory systems, deep tendon reflexes, and coordination. Motor assessment should include tone and bulk in addition to strength.
Physical examination of patients for ICUAW is dependent on the cooperation and maximal effort of the patient—an aspect of bedside assessment that can be confounded by sedation and delirium. When a reliable motor examination is possible, affected patients will exhibit diffuse, generally symmetrical motor deficits in all limbs, ranging from paresis to true quadriplegia.18 Weakness affects the extremities and diaphragm yet often spares the cranial nerves; accordingly, pupillary and oculomotor function and facial grimace are usually preserved. Patients often have concurrent respiratory failure with protracted dependence on mechanical ventilation.
An early clue for isolated myopathy (without neuropathy) is that painful stimulation—such as pressure upon the nail bed—results in a limited to absent limb response, yet normal grimacing. For patients with ability to undergo a reliable sensory examination, deficits to light touch and pin prick may implicate the presence of polyneuropathy. Reflexes are usually diminished to absent, but normal reflexes do not rule out the diagnosis.
The most commonly reported test of muscle strength in critically ill patients is manual muscle testing. A standardized bedside muscle exam can be utilized to evaluate individual muscle groups. The Medical Research Council (MRC) Score grades the strength of functional muscle groups in each extremity on a scale from zero to five (Table 83-1).19 Individual MRC scores obtained from predefined muscle groups can be combined into a sum score, yielding a global estimate of motor function. The usual standard is to combine three muscle group scores for each limb; therefore, sum scores span from zero (complete paralysis) to 60 (full strength). This scoring has demonstrated excellent inter-rater reliability and can be utilized to document the extent of disease and track serial changes over time.20,21
Medical Research Council (MRC) Neuromuscular Examination
| Functions Assessed: |
| Upper extremity: Wrist flexion, forearm flexion, shoulder abduction |
| Lower extremity: Ankle dorsiflexion, knee extension, hip flexion |
| Score for Each Movement: |
| 0—No visible contraction |
| 1—Visible muscle contraction, but no limb movement |
| 2—Active movement, but not against gravity |
| 3—Active movement against gravity |
| 4—Active movement against gravity and resistance |
| 5—Active movement against full resistance |
| Maximum score: 60 (4 limbs, maximum 15 points per limb)—Normal |
| Minimum score: 0—Quadriplegia |
To better characterize the incidence of acquired neuromuscular disorders in the ICU and to validate the bedside muscle strength examination, De Jonghe and colleagues prospectively evaluated 95 patients without preexisting neuromuscular injury that had undergone mechanical ventilation for greater than 7 days.22 The first day a patient was awake and following commands was considered day 1. On the seventh day after awakening, patients underwent MRC muscle strength testing to determine a sum score. A priori, they labeled patients with a sum score of less than 48 to have “ICU-acquired paresis.” To confirm the peripheral neuromuscular origin of the clinical weakness, all patients underwent an electrophysiologic examination exam at day 7 and persistently weak patients underwent muscle biopsy at day 14. All patients with ICU-acquired paresis demonstrated sensory-motor axonopathy. Histological features of primary myopathic changes were observed in all patients with paresis persisting 1 week after the initial diagnosis.
Since this landmark trial, leaders in the field have established use of the term “ICU-acquired weakness” to characterize clinically detected weakness in critically ill patients in whom there is no plausible etiology other than critical illness.5 ICUAW, synonymous with ICU-acquired paresis, is defined by the MRC muscle strength sum score <48 in a patient that is awake and able to follow commands (Table 83-2). Since this delineation, this diagnosis has been repeatedly applied as a secondary end point in prospective clinical trials to crudely assess for the presence of muscle injury and weakness.23,24
Diagnostic Features of ICUAW
|
The intensivist should remain cognizant of the limitations of the MRC strength examination. It requires a patient who is awake, cooperative, and capable of contracting muscle with maximal force. Scores also can be affected by patient positioning, the number of limbs available for assessment (pain, dressings, amputation), and, most importantly, timing. Experts have lamented other limits including the omission of distal lower extremity function and poor ability to detect subtle changes over time.
DIFFERENTIAL DIAGNOSIS
Generalized weakness may result from injury to the brain or brainstem, myelopathies, anterior horn cell disorders, polyneuropathies, neuromuscular junction disorders, and muscle disorders (Table 83-3). The weakness may represent the exacerbation or unmasking of a chronic underlying neuromuscular disease. Alternatively, the weakness may represent the acute neuromuscular condition. In cases of uncertainty, additional tests should be performed, including neuroimaging of the brain, brainstem, or spinal cord; infectious and immunologic serologies, cerebrospinal fluid analysis, and electrophysiology (EP) studies.
Acute Generalized Weakness Syndromes in Critically Ill Patients
Bilateral or paramedian brain or brainstem lesionsa
|
Spinal cord disordersa
|
Anterior horn cell disorders
|
Polyradiculopathies
|
Peripheral nervous disorders
|
Neuromuscular junction disorders
|
Muscle disorders
|
With a good history and physical examination, many of the differential diagnoses can be excluded with confidence. Given that some of the other diagnoses are treatable, ICUAW should be regarded as a diagnosis of exclusion. The weakness must follow the onset of the critical illness; symptoms prior to admission should direct attention to other etiologies. The inability to interview the patient, due either to intubation or delirium may limit historical detail and proper physical examination. The presence of delirium should not dissuade the search for a neuromuscular disorder, especially when cognition is improving and the weakness is not.
ADJUNCTIVE TESTING FOR NEUROMUSCULAR INJURY
Methods to confirm ICUAW and identify its subcategories include EP studies, direct muscle stimulation, and morphologic analysis of muscle or nerve tissue. These tests help to exclude other differential diagnoses and can help to characterize the specific subcategory of ICUAW: neuropathy, myopathy, neuromyopathy, or prolonged neuromuscular junction blockade. This section details the application of each test. Figure 83-2 provides an algorithm for the work-up of a patient exhibiting weakness or inactivity.