Hypoxemia (Decr PaO2):
Links: 5 Mechanisms (V/Q, Shunt etc) | Lab & W/u | Hypoxia | Cyanosis | Pulse Oximetry | Methemoglobin | O2 therapy | See A-a Gradient |
 Decrease O2 in the tissue. Subnormal oxygenation of arterial blood (decr delivery from the atm to the blood). Low PO2 in arterial/ capillary or venous blood. Short of anoxia.
Decrease O2 in the tissue. Subnormal oxygenation of arterial blood (decr delivery from the atm to the blood). Low PO2 in arterial/ capillary or venous blood. Short of anoxia.
ICD9 = 799.02.
Normal PAO2 = 80-100mmHg. If normal but cyanotic with decr sat think met-Hb. If sat high for the PaO2 think cyanide or carboxy-Hb.
SaO2 =: Oxygen saturation: Percentage of hemoglobin which is oxygenated (93-98%).
At pH=7.4 and Temp=37C.
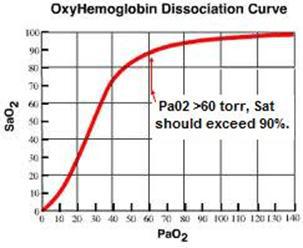
90% ~ 60 mmHg PaO2.
80% ~ 40 mmHg PaO2.
70% ~ 30 mmHg PaO2.
Evaluation of the PaO2:
80–100 mmHg Normal.
60-80 mmHg = Mild hypoxemia.
40-60 mmHg = Moderate hypoxemia.
<40 mmHg = Severe hypoxemia.
To determine PaO2: subtract 1mmHg for each decade of age. (or 100- 1/3Age) Subtract 3mmHg for every 1000 ft of altitude. Usually accompanied by an acidosis (pH <7.2), base deficit >5mEq with bicarb <20. AG >8 mEq/L, blood lactate >2mEq/L.
Ventilatory control is 3 main components: chemosensors (carotid body senses PaO2 & H+. Medullary senses PaCO2 & H+), the central controller (respiratory center in brainstem) and the effectors (respiratory muscles such as the diaphragm, intercostals and abd muscles).
Hypoxemia with a Clear Chest X-Ray: It is not uncommon for pt’s to present with life-threatening hypoxemia without major radiographic evidence of infiltration. In such cases, occult shunting and severe V/Q mismatching are the most likely mechanisms. Intracardiac or intrapulmonary shunts, asthma and other forms of airway obstruction, low lung volume superimposed on a high closing capacity (bronchitis in a supine obese pt), pulmonary embolism, and occult microvascular communications (such as occur in pt’s with cirrhosis) are potential explanations. Hypoxemia is amplified by profound desaturation of mixed venous blood, by reversal of hypoxic vasoconstriction with therapeutic vasoactive agents (nitroprusside, calcium channel blockers, and dopamine), and by the severe V/Q imbalance consequent to acute head injury. (Acute oxygenation crises following head trauma has been termed “nonedematous respiratory distress syndrome,” NERDS).
Asphyxia: the failure to provide the cell with oxygen and remove carbon dioxide, resulting in metabolic acidemia. Both circulation and ventilation are essential to avoid asphyxia.
Oxygen–hemoglobin dissociation curve:
The oxygen–hemoglobin dissociation curve plots the proportion of haemoglobin in its saturated form on the vertical axis against the prevailing oxygen tension on the horizontal axis. The oxyhaemoglobin dissociation curve is an important tool for understanding how our blood carries and releases oxygen. Specifically, the oxyhaemoglobin dissociation curve relates oxygen saturation (SO2) and partial pressure of oxygen in the blood (PO2), and is determined by what is called “haemoglobin’s affinity for oxygen”; that is, how readily haemoglobin acquires and releases oxygen molecules into the fluid that surrounds it.
Left shift (high affinity for O2): Temperature decrease. 2.3-DPG decrease. p(CO2) decrease. p(CO) increase. pH (Bohr effect) Increase (alkalosis). Increase in fetal hemoglobin.
Right shift (low affinity for O2): Temperature increase. 2.3-DPG increase. p(CO2) increase. p(CO) decrease. pH (Bohr effect) decrease (acidosis). Type of hemoglobin adult hemoglobin. Mnemonic: “CADET, face Right!” for CO2, Acid, 2,3-DPG, Exercise and Temperature. Factors that move the oxygen dissociation curve to the right are those physiological states where tissues need more oxygen. For example during exercise, muscles have a higher metabolic rate, and consequently need more oxygen, produce more carbon dioxide and lactic acid, and their temperature rises.
Adequacy of Oxygenation and the 30-60 … 60-90 rule: With a Pa02 greater than 60 torr, hemoglobin saturation should exceed 90%. A violation of this rule for oxyhemoglobin saturation indicates that something else has displaced oxygen from the hemoglobin. Methemoglobin |
Oxygen Content: O2 Content = ((Hgb x 1.34 x sat) + (Pa02 x 0.0031)). Thus, increasing the PaO2 when the O2 sat is near 90% has little affect compared (see O2 dissociation curve) to increasing the Hb.
Oxygen Transport: O2 Delivery = Cardiac output x O2 Content. This is an interplay of cardiac and pulmonary to deliver oxygen to the tissues. Delivery can be aided by increasing Hgb or cardiac output.
Oxygen Delivery: Usually in the ICU we can achieve a Hgb of 10, O2 Sat of > 90% expressed as 0.90, 0.95. Therefore, oxygen delivery in the critically ill patient is primarily manipulated through changes in the cardiac output.
5 Main Mechanisms of Hypoxemic Hypoxia: See Hypoxemia |
1. Ventilation-Perfusion (V/Q) mismatch: Causes >95% of hypoxemia in clinical medicine. Due to airway secretions, pulmonary embolism, bronchospasm (asthma, COPD), CHF, tumor-filled alveoli, interstitial lung disease, silicosis, acute pulmonary edema. Ventilation to a region of the lung is decreased in comparison to perfusion. Have normal / decr/ incr PaCO2, incr A-aDO2, good response to incr FiO2.
“V” – ventilation – the air which reaches the alveoli.
“Q” – perfusion – the blood which reaches the alveoli.
• An area with no ventilation (and thus a V/Q of zero) is termed “shunt.”
• An area with no perfusion (and thus a V/Q undefined though approaching infinity) is termed dead space.
2. Shunt (R to L): V/Q ~ = 0. Atelectasis, lobar pneumonia, pulmonary edema, intracardiac shunt, and ARDS (an increase in alveolar fluid causing reduced diffusion of oxygen into capillaries). This occurs when systemic venous blood enters the L heart w/o prior oxygenation. Ventilation =0, but perfusion continues. Shunts will not significantly correct with 100% O2 (unlike V/Q mismatch and diffusion defects). Has normal/ decr PaCO2, incr A-aDO2, minimal response to incr FiO2. Require positive pressure and/or PEEP to recruit alveoli.
3. Low Inspired PO2: high altitude. Has normal or decr PaCO2, normal A-aDO2, good response to incr FiO2. Normal A-a gradient.
4. Alveolar Hypoventilation: The most common causes in the ICU are drug-induced respiratory depression and neuromuscular weakness. Can be due to COPD, low respiratory drive from sedation (overdose narcotics) or hypothyroid or idiopathic alveolar hypoventilation or central (brain stem) dz, mechanical breathing problem (GBS, polio, MG, kyphoscoliosis, Pickwickian syndrome, myopathy, chest wall abnormality, crushed thoracic cage). Brainstem depression (opiates, benzo), obesity-hypoventilation syndrome, critical illness polyneuropathy, phrenic nerve injury (cardiac surgery), shock/multiorgan failure, myasthenia/Guillain-Barré, myopathic d/o’s (prolonged paralysis, hypophosphatemia, magnesium depletion, low cardiac output).
S/s: H-A, somnolence, decr cognitive ability, constricted pupils, asterixis, coma, diaphoresis, tachycardia, arrhythmia, cor pulmonale (late), polycythemia. Has incr PaCO2, normal A-aDO2, with good response to incr FiO2. Normal A-a gradient.
5. Diffusion Defect: interstitial lung dz, PCP pneumonia. Has normal – decr PaCO2, incr A-aDO2, good response to incr FiO2.
Other Causes of Hypoxia:
• Anemia in which arterial oxygen pressure is normal, but total oxygen content of the blood is reduced. This is due to a decreased total carrying capacity, such as a reduced Hemoglobin content.
• Hypoxia when the blood fails to deliver oxygen to target tissues.
Carbon monoxide poisoning which inhibits the ability of hemoglobin to release the oxygen bound to it.
Methemoglobinemia in which an abnormal version of hemoglobin accumulates in the blood
• Histotoxic hypoxia in which quantity of oxygen reaching the cells is normal, but the cells are unable to use the oxygen effectively, due to disabled oxidative phosphorylation enzymes. Cyanide toxicity is one example.
Labs: Abnormality –> PO2\ PCO2\ Room air O2/ Aa Gradient\ 100% O2 PaO2:
Hypoventilation –> decr\ incr\ Nl\ improves.
V/Q Mismatch –> decr\ Incr-Decr\ incr\ improves.
Fixed Shunt –> decr\ decr or nl\ incr\ minimal Incr.
Diffusion Barrier –> decr\ nl\ incr\ Nl.
Dx of Hypoxemia: PaO2 <60mmHg or SaO2<90%.
Evaluation of Hypoxemia: Note: Once recognized, transport to emergency room via ACLS (if already hospitalized, consider a monitored setting). Consider prompt intubation if not immediaterly corrected with O2 therapy as things can go bad quickly (agonal respirations, PEA, VF/VT etc).
Step #1: Is the pO2 <80 mm Hg? Is the pCO2 increased? If the pO2 is >= 80 mm Hg, adequate oxygenation is present.
Step #2: Is the Alveolar-arterial oxygen difference (A-a Gradient) increased?
Upper Limit of Normal a-A gradient in mm Hg for age:
<40yo–> 10. 40-50–> 15.
50-59–> 20. 60-69–> 25. >= 70–> 30. A-a Gradient |
Step #3: Does oxygen therapy correct the problem?
If a-A gradient normal, rapid response to O2–> hypoventilation (incr pCO2) or low inspired oxygen concentration (normal or low pCO2).
If a-A gradient incr, rapid response to O2–> ventilation-to-perfusion mismatch.
If a-A gradient incr, no or minimal increase in pO2–> right-to-left shunt or impaired diffusion.
Cause & Example:
Low inspired O2 tension: Mountaineering. Decr Pao2. Paco2 Normal or Decr. A-aDo2 Normal. Good response to incr FIo2.
Hypoventilation: Drug overdose. Decr Pao2. Paco2 Incr. A-aDo2 Normal. Good response to incr FIo2.
Diffusion impairment: Pulmonary fibrosis plus exercise. Decr Pao2. Paco2 Normal or Decr. A-aDo2 Incr. Good response to incr FIo2.
Ventilation-perfusion imbalance: COPD; pneumonia. Decr Pao2. Paco2 Normal, Decr, or incr. A-aDo2 Incr. Good response to incr FIo2.
Right-to-left shunt: Pulmonary edema. Decr Pao2. Paco2 Normal or Decr. A-aDo2 Incr. Poor response to incr FIo2.
Arterial Hypocapnia: In its simplest form, the partial pressure of arterial carbon dioxide (PaCO2) reflects the balance between the production and elimination of carbon dioxide (CO2), as described by the following formula: PaCO2 is proportional to (CO2 production / CO2 elimination) + inspired CO2. The volume of inspired carbon dioxide is usually negligible, whereas reduced carbon dioxide production is an unusual, but possible, contributor to hypocapnia. Therefore, for practical purposes, a low partial pressure of arterial carbon dioxide reflects the rate of elimination of carbon dioxide. Systemic hypocapnia results in cerebrospinal fluid alkalosis, which decreases cerebral blood flow, cerebral oxygen delivery, and to a lesser extent, cerebral blood volume.
Link: O2 therapy | Cyanosis | Hypoxemia |
Usually due to the decr delivery of O2 to the tissue (shock, anemia). Hypoxemia can occur independently, but hypoxia is often the result of severe hypoxemia.
ICD-9 codes: 799.01: asphyxia. 799.02: hypoxemia.
Types of Hypoxia:
Hypoxemic Hypoxia –> a lower than normal PaO2 (hypoxemia).
5 causes: seen with alveolar diffusion impairment, decr alveolar PO2 (decr FiO2, hypovent, incr altitude), R-L shunt, VQ mismatch.
Hypoxia with normal PaO2:
Anemic Hypoxia –> decr RBC count, carboxy-Hb, hemoglobinopathy.
Circulatory (Hypoperfusion) Hypoxia –> decr cardiac output, decr local perfusion.
Affinity Hypoxia –> decr release of O2 from Hb to tissues (CO, Met-Hb).
Histotoxic Hypoxia –> cyanide poisoning.
Respiratory Failure –> NM blockage (aminoglycosides, succinylcholine, Gallamine, Dimethyltubocurarine, CCB, Mg sulfate, Nicotine, macrolides, Penicillamine, Polymyxin B).
CNS depression (sedatives, narcotics, hypnotics, ETOH, TCA’s, O2).
Inhibition of transmission at neuromuscular junction (Captopril, Cytosine-arabinoside, Danazol, Gold, Phenytoin, Vincristine), respiratory muscle myopathy (beta agonists like fenoterol, corticosteroids, Clofibrate, diuretics, narcotics, Pancuronium, Procainamide).
S/s of Hypoxia: acute hepatic necrosis, ATN, agitation, altered MS, angina, anxiety, arrhythmias, claudication, coma, confusion, cyanosis, diaphoresis, dizziness, gangrene, HTN, hypotension, lactic acidosis, sz, somnolence, syncope, tachycardia, tachypnea.
Links: Definition & Causes | W/u, Tx & DDx | Hypoxemia | A bluish color of the skin and mucous membranes resulting from an increased amount of deoxyhemoglobin (not based on % or relative amount). Becomes clinically apparent when there is >5g/dL of unsaturated Hb (deoxyhemoglobin), which corresponds to a pAO2 of <50 torr (50% of Hb w/o O2) or SaO2 <85%. It may not be apparent in pt has a coexisting anemia. Other factors that affect the ability to detect cyanosis include skin thickness and pigmentation, lighting, ambient temperature, and skin microcirculation. The tongue is very sensitive for identifying cyanosis. The earlobes, nail beds, and conjunctiva are less reliable.
Central (Hypoxia): Central cyanosis is usually the result of deoxyhemoglobin. Seen in the nail beds and mucous membranes (tongue, conjunctiva) under natural light. Occurs in warm and cold areas. If fingers are pink but the toes are cyanotic, consider a persistent ductus arteriosus with a reversible R-L shunt seen in pulmonary HTN (Eisenmenger’s syndrome).
Cardiac Causes: Congenital heart disease with right-to-left shunting or admixture lesions. Congenital heart disease causing obstruction to pulmonary blood flow (e.g., pulmonary atresia with intact ventricular septum). Congenital heart disease with large left-to-right shunts causing pulmonary vascular congestion (e.g., large ventricular septal defect).
Pulmonary Causes: Airway obstruction (congenital or acquired). Asthma or bronchiolitis. COPD. Obstructive (including sleep) apnea. Pneumonia or other infection. Pulmonary hypoplasia. Meconium aspiration (newborn). Respiratory distress syndrome (newborn). Transient tachypnea of the newborn. Cystic fibrosis. Pulmonary edema. Intrapulmonary shunting (e.g., pulmonary arteriovenous fistula). Pulmonary hypertension resulting in right-to-left shunting (e.g., primary pulmonary hypertension, persistent pulmonary hypertension of the newborn). Pneumothorax. Atelectasis.
Neurolgical Causes: Intracranial hemorrhage. Maternal sedative administration (newborn). Sedative ingestion / OD. Infection (e.g., meningitis). Neuromuscular disease. Hypoxic insult. Seizure. Central apnea. Breath holding.
GI Causes: Diaphragmatic hernia. Gastroesophageal reflux leading to aspiration. Chronic liver disease causing pulmonary arteriovenous fistulas (hepatopulmonary syndrome).
Hematological Causes: Acquired methemoglobinemia (e.g., aniline dye; anesthetics, including topical and oral; nitrates). Hereditary methemoglobinemia (NADH cytochrome-b5 reductase deficiency). Abnormal hemoglobin variants (typically benign cyanosis).
Peripheral: results from increased oxygen uptake in peripheral tissues due to alterations in local caplillary blood flow (exposure to cold, passive congestion from polycythemia) or abnormally increased uptake of O2 from normal saturated arterial blood can cause. The result of poor peripheral circulation, leading to increased oxygen extraction by the peripheral tissues. Seen in cool exposed areas such as fingers, earlobes, tip of nose, cheeks, outer surface of the lips. It is due to increased capillary O2 extraction secondary to poor perfusion, and may be obliterated by warming or massaging the area.
Causes: Exposure to cold. Shock. Sepsis. Hypoglycemia. Acidosis. Raynaud phenomenon. Congestive heart failure. Prominent venous plexuses mimicking cyanosis. Acrocyanosis of the newborn. Breath holding.
W/u: ABG analysis will confirm the presence of hypoxia leading to cyanosis. Other useful tests include a hematocrit to detect anemia or polycythemia vera, a chest radiograph, and an electrocardiogram.
ICD-9 Code: 782.5 Cyanosis
Tx: Guided by the underlying cause. Supplemental oxygen. If the pt is unresponsive to supplemental oxygen, poor perfusion, acquired hemoglobinopathies, or large right-to-left shunts may be present. Furosemide (Lasix) should be given if CHF is present. Shock should be aggressively addressed. Electrolyte abnormalities, hypoglycemia, and acidosis should be corrected. Consider bronchodialtors such as Albuterol NEB. If airway obstruction is suspected, laryngoscopy or bronchoscopy may be indicated. In cases of methemoglobinemia, IV methylene blue at a typical dose of 1 to 2 mg/kg promptly removes methemoglobin and resolves cyanosis.
Peds: In neonates with suspected cyanotic congenital heart disease, pulmonary blood flow isoften dependent on shunting through a patent ductus arteriosus. In these patients, an intravenous infusion of prostaglandin E1 should be started, typically at a dose of 0.05 to 0.1 ¼g/kg per minute, to keep the ductus open while the evaluation progresses.
Ddx: Shock, arterial insufficiency, asthma, COPD, hypoventilation, methemoglobinemia (Should be considered when cyanosis is unresponsive to oxygen therapy and there is a normal cardiorespiratory examination.), Patent ductus arteriosis, SVC obstruction, tricuspid insufficiency, tracheal obstruction, intrapulmonary shunting, polycythemia vera, R-to-L cardiac shunt, pulmonary embolism, arterial insufficiency, upper airway obstruction, respiratory failure. Carboxyhemoglobin, and other acquired hemoglobinopathies.
Sulfahemoglobinemia: exposure to pheactin, acetanalid or sulfonamides can cause sulfer to bind to Hb. Dyshemoglobinaemias should be considered as possible causes of cyanosis, particularly in the presence of a relatively normal PaO2. This inert molecule cannot transport O2. Can get greenish-black arterial blood if have cyanosis caused by sulfhemoglobin (2 g/L) possibly brought on by heavy doses of the migraine therapy sumatriptan (Imitrex) (Dark green blood in the operating theatre. Lancet 2007;369:1972). A co-oximeter does not measure in the 620 nm wavelength at which sulfhemoglobin has peak absorption, and therefore shows as normal for both methhemoglobin and carboxyhemoglobin.
Dx with spectroscopy. Tx is supportive.
Pseudocyanosis: should be considered in any asymptomatic pt, but it should be a dx of exclusion. Pseudocyanosis is caused by abnormal skin pigmentation, giving the skin a bluish or silver hue. Causative agents include heavy metals (iron, gold, lead, and silver) and certain drugs (phenothiazines such as chlorpromazine, minocycline, amiodarone, and chloroquine). Amiodarone deposits in the skin. Silver rubbed into skin gives a blue discoloration when exposed to sun. Drug-induced Pseudocyanosis (Am J Med 2008;121:385-6)…..Heavy metals such as silver (argyria) and gold (chrysiasis) can also cause.
Harlequin cyanosis: one arm only, seen in aortic dissection, patent ductus arteriosis with pulmonary HTN and with embolic arterial occlusion.
**Ref: (Neurologic manifestations of pulmonary disease. Neurol Clin. 1989;7:605-16) (Cecil’s Textbook of Medicine, 21st ed., 2000, Saunders, pp379-83) (Consultation with the specialist: nonrespiratory cyanosis. Pediatr Rev. 1999;20:350-2) (Pleuropulmonary manifestations of systemic lupus erythematosus. Thorax. 2000;55:159-66)
Pulse Oximetry: See Hypoxemia |
Gives continuous real-time estimates of arterial saturation in the range of 80-100%, and provides an early warning of diminished perfusion while avoiding the discomfort and risks of arterial puncture. The absorption characteristics of oxyhemoglobin and deoxy-hemoglobin (reduced) are at different wavelengths (660nm, red and 940, infrared). The oximeter uses the light to estimate the ratio (assuming that the pulsatile portion represents arterial and the nonpulsatile is a mixture) to give an estimate of the SaO2. The pulse ox is calibrated to a blood co-oximeter (a spectrophotometer) that measures reduced Hb, oxy-Hb, Met-Hb, carboxy-Hb. There is excellent correlation between 75-100% saturation, otherwise it is a nonlinear relationship.
O2 SATs (normal is 80-100%):
50% –> ~27mmHg.
60% –> ~30. 75% –> ~40.
85% –> 55mmHg. 90% –> 60.
95% –> 80. 97% –> 100mmHg.
Beer’s Law: the concentration of an unknown solute dissolved in a solvent can be determined by light absorption.
May fail if: pt with hypotension/ hypothermia/ shock (low perfusion states) or perfusion of vasoconstrictors, as vasoconstriction leads to underestimation of O2 sat. Not calibrated for extremely low saturation levels (<70%). Motion artifacts. Erroneous reading when Hb <5g/dL, conditions with incr venous pulsations (TR, R heart failure, a tourniquet or BP cuff above the probe), excessive light (surgical lamp, direct sunlight), dyes & pigments (methylene blue, indigo carmine, indocyanine green, nail polish), met-Hb interferes with reading (local anesthetics, nitrates, Metoclopramide, sulfa drugs, Ca-EDTA). Darkly pigmented skin and anemia also affect the accuracy.
Effect of Fingernail Polish: There is a small decrease in O2 sat (~2%) in fingernails painted with either brown or black fingernail polish when measured with the probe in the top-to bottom position (no effect with red, yellow, dark blue, green, purple, fuchsia, light blue, and white colors). However, placing the probe in a side-to-side position precluded any minor effects fingernail polishes may have, and so may obviate the need to remove fingernail polish (Chest 2003, June 01).
Indications: During emergency airway management it can assist in assessing need for further airway management and adequacy of preoxygenation before endotracheal intubation. Used to monitor ventilator and Fi O2 changes and provide early indicator of ventilator dysfunction. Used to assist routine weaning of O2 therapy, but not mechanical ventilation. Helpful to monitor pt’s with lung dysfunction for unexpected hypoxic events. Monitor during procedures including during systemic sedation. Monitor oxygenation during interhospital and intrahospital transfer. Assess acute childhood asthma.
Masimo SET LNOP Blue Sensor: FDA approved in 8/05 as the first pulse oximeter sensor to accurately monitor cyanotic babies. Measures the oxygen saturation of arterial blood (SpO2) in pediatric, infant and neonatal pt’s with congenital cardiac lesions with accuracy of 3% from 100-80% and accuracy of 4% from 80-60%.
Factors Affecting Readings:
Severe anemia: Satisfactory readings obtained down to hemoglobin level of 5 mg/dL.
Motion-artifact: depending on probe sites. Yet forehead and nasal bridge probes may be less accurate than the finger and ear probes.
Dyes: Transient effect unless methemoglobinemia results. Methylene blue absorbs light at 660 nm, similar to the absorption of reduced hemoglobin, can artificially lower readings.
Light-artifact: Minimize by covering probe with opaque material.
Hypoperfusion: Inadequate pulse signal will be displayed. Requires a pulsating vascular bed, no reading if hypotension with vasoconstriction, hypothermia, or the administration of vasoconstricting drugs.
Electrocautery: Minimize by increasing the distance of the sensor from the surgical site.
Deep pigmentation: Use fifth finger, earlobe, or other area of lighter pigmentation.
Dark nail polish: Remove with acetone or place sensor sideways on digit.
Dyshemoglobinemias (e.g., carboxyhemoglobin and methemoglobin): Falsely elevate saturation reading.
Elevated bilirubin: Accurate up to bilirubin level of 20 mg/dL in adults; no problem reported for jaundiced children.
High saturation: Pulse oximetry not useful for monitoring hyperoxemia in neonates.
Fetal hemoglobin: No effect on pulse oximetry (remains accurate); falsely reduced CO-oximetry readings.
Venous pulsations: Artificially lower O2 saturation; choose probe site above the heart.
Dialysis graft (A-V fistula): No difference from contralateral extremity unless fistula produces distal ischemia.
Rad-57 Pulse CO-Oximeter: uses 8 wavelengths of light instead of 2 to measure both carboxyhemoglobin and methemoglobin. Conventional pulse oximeters use only two wavelengths of light, so they cannot distinguish between oxyhemoglobin and carboxyhemoglobin; they provide falsely high oxygen readings even when carboxyhemoglobin levels are as high as 70%. This oximeter appears to accurately measure these two dyshemoglobins (Anesthesiology 2006;105:892-7)…The device is a potentially invaluable resource for emergency departments if these results hold up in clinical practice and across a wider spectrum of carboxyhemoglobin and methemoglobin levels.
Transcutaneous (ear-clip) carbon dioxide measurement correlated well with results of arterial sampling (ABG) in 21 consecutive nonagitated adult patients with acute respiratory failure who presented to a single emergency department in France during a 1-month period (Intensive Care Med 2010:Nov 11;e-pub ahead of print)……shows great promise as an alternative to end-tidal–based capnometry.
**Ref: (Pulse oximetry. Respir Care Clin N Am. 1995;1:77-105) (Methemoglobinemia: etiology, pharmacology, and clinical management. Ann Emerg Med 1999;34:646-56)
Hypercapnia = Hypercarbia (Incr PaCO2):
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








