Hypertensive crisis is characterized by severe hypertension associated with end-organ damage (hypertensive emergency) or impending end-organ damage (hypertensive urgency).
Hypertensive crisis is characterized by severe hypertension associated with end-organ damage (hypertensive emergency) or impending end-organ damage (hypertensive urgency). Hypertensive crisis can develop either de novo or as a complication of preexisting essential or secondary hypertension. Any disorder that causes hypertension can give rise to a hypertensive crisis.
Hypertensive crisis can develop either de novo or as a complication of preexisting essential or secondary hypertension. Any disorder that causes hypertension can give rise to a hypertensive crisis. Hypertensive crisis is a rapid onset, acute disease and therefore a trigger factor may be implicated in its pathogenesis; these include neurohormonal factors such as the renin-angiotensin system, endothelin, vasopressin, and catecholamines.
Hypertensive crisis is a rapid onset, acute disease and therefore a trigger factor may be implicated in its pathogenesis; these include neurohormonal factors such as the renin-angiotensin system, endothelin, vasopressin, and catecholamines. The endothelium in resistance vessels plays a central role in blood pressure (BP) homeostasis, as it attempts to compensate for changes in vascular resistance through increased autocrine and paracrine release of vasodilator molecules, such as nitric oxide and prostacyclin.
The endothelium in resistance vessels plays a central role in blood pressure (BP) homeostasis, as it attempts to compensate for changes in vascular resistance through increased autocrine and paracrine release of vasodilator molecules, such as nitric oxide and prostacyclin. In sustained severe hypertension, these compensatory endothelium-mediated vasodilator responses are overwhelmed, which leads to endothelial decompensation, endothelial failure, and vasoconstriction.
In sustained severe hypertension, these compensatory endothelium-mediated vasodilator responses are overwhelmed, which leads to endothelial decompensation, endothelial failure, and vasoconstriction. Clinical manifestations consist of features related to hypertension and those related to target organ injury. The absolute BP is often not as important as the rate of elevation. Acute elevations in BP are less well tolerated and more likely to produce symptoms than are chronic elevations.
Clinical manifestations consist of features related to hypertension and those related to target organ injury. The absolute BP is often not as important as the rate of elevation. Acute elevations in BP are less well tolerated and more likely to produce symptoms than are chronic elevations. Clinical distinction between hypertensive emergency and hypertensive urgency is crucial; however, the principles of treatment are the same.
Clinical distinction between hypertensive emergency and hypertensive urgency is crucial; however, the principles of treatment are the same. The principal goals of treatment are tightly controlled BP reduction and prevention of end-organ injury. The recommended aim is to reduce the mean arterial pressure by 20%-25% within a period of 15 minutes to 2 hours. Subsequent rate of reduction of the BP is dictated by clinical status and the rapidity with which the hypertension may have evolved. Too rapid a reduction in BP is to be avoided, as that can worsen end-organ dysfunction except in the treatment of hypertensive crisis associated with aortic dissection where appropriate treatment requires rapid reduction of systolic BP to minimize aortic wall stress.
The principal goals of treatment are tightly controlled BP reduction and prevention of end-organ injury. The recommended aim is to reduce the mean arterial pressure by 20%-25% within a period of 15 minutes to 2 hours. Subsequent rate of reduction of the BP is dictated by clinical status and the rapidity with which the hypertension may have evolved. Too rapid a reduction in BP is to be avoided, as that can worsen end-organ dysfunction except in the treatment of hypertensive crisis associated with aortic dissection where appropriate treatment requires rapid reduction of systolic BP to minimize aortic wall stress. Choice of drugs must take into account organs involved in the disease process and the adverse effect profile.
Choice of drugs must take into account organs involved in the disease process and the adverse effect profile. distinct: hypertensive emergencies and hypertensive urgencies. Hypertensive emergency is defined as sudden, severe hypertension complicated by acute end-organ damage; hypertensive urgency is characterized by severely elevated BP without end-organ damage (2). The clinical distinction between these two groups is the presence or absence of target organ damage— not the absolute level of the BP. The organ systems most frequently involved are those that maintain strict autoregulation to sustain physiologic function, including the central nervous system (CNS), cardiovascular system, and kidneys (Table 112.1). Involvement of these organ systems results in specific clinical syndromes.
distinct: hypertensive emergencies and hypertensive urgencies. Hypertensive emergency is defined as sudden, severe hypertension complicated by acute end-organ damage; hypertensive urgency is characterized by severely elevated BP without end-organ damage (2). The clinical distinction between these two groups is the presence or absence of target organ damage— not the absolute level of the BP. The organ systems most frequently involved are those that maintain strict autoregulation to sustain physiologic function, including the central nervous system (CNS), cardiovascular system, and kidneys (Table 112.1). Involvement of these organ systems results in specific clinical syndromes.TABLE 112.1 MANIFESTATIONS OF HYPERTENSIVE CRISES | ||
|---|---|---|
|
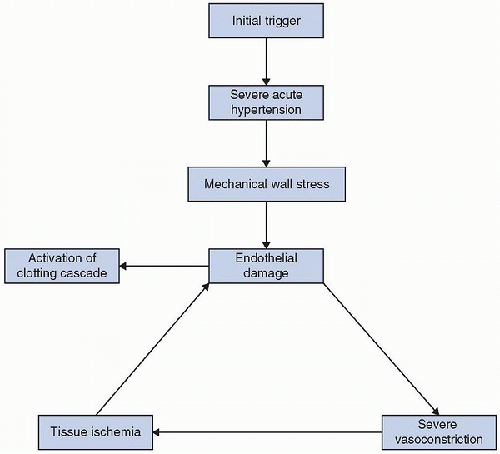
 (Table 112.2). Any disorder that causes hypertension can give rise to hypertensive crisis. The endothelium in resistance vessels plays a central role in BP homeostasis, as it attempts to compensate for changes in vascular resistance through increased autocrine and paracrine release of vasodilator molecules, such as nitric oxide and prostacyclin. With sustained severe hypertension, these compensatory endothelium-mediated vasodilator responses are overwhelmed, which leads to endothelial decompensation, endothelial failure, and vasoconstriction (5). Although the detailed pathophysiology of hypertensive crisis remains to be elucidated, an initial abrupt
(Table 112.2). Any disorder that causes hypertension can give rise to hypertensive crisis. The endothelium in resistance vessels plays a central role in BP homeostasis, as it attempts to compensate for changes in vascular resistance through increased autocrine and paracrine release of vasodilator molecules, such as nitric oxide and prostacyclin. With sustained severe hypertension, these compensatory endothelium-mediated vasodilator responses are overwhelmed, which leads to endothelial decompensation, endothelial failure, and vasoconstriction (5). Although the detailed pathophysiology of hypertensive crisis remains to be elucidated, an initial abrupt  increase in vascular resistance seems to be a necessary step and is likely related to a sudden surge in humoral vasoconstrictors (6). Activation of the renin-angiotensin system, nitric oxide (NO), endothelin, vasopressin, and catecholamines has been postulated to play important roles in the pathophysiology of hypertensive crises (7,8,9).
increase in vascular resistance seems to be a necessary step and is likely related to a sudden surge in humoral vasoconstrictors (6). Activation of the renin-angiotensin system, nitric oxide (NO), endothelin, vasopressin, and catecholamines has been postulated to play important roles in the pathophysiology of hypertensive crises (7,8,9).TABLE 112.2 CAUSES OF HYPERTENSIVE CRISIS | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
 fibrin (Fig. 112.1). Further progression leads to fibrinoid necrosis of the arterioles with resulting ischemia and the release of additional vasoactive mediators generating a vicious cycle of repeated injury (6,16,17). Activation of the renin-angiotensin system leads to further vasoconstriction and production of proinflammatory cytokines such as interleukin-6 (IL-6) (14,18). The process also triggers an increase in NADPH oxidase activity, which generates the release of reactive oxygen species (ROS) and further tissue injury (19,20).
fibrin (Fig. 112.1). Further progression leads to fibrinoid necrosis of the arterioles with resulting ischemia and the release of additional vasoactive mediators generating a vicious cycle of repeated injury (6,16,17). Activation of the renin-angiotensin system leads to further vasoconstriction and production of proinflammatory cytokines such as interleukin-6 (IL-6) (14,18). The process also triggers an increase in NADPH oxidase activity, which generates the release of reactive oxygen species (ROS) and further tissue injury (19,20).well as chronic inhibition of NO synthesis with N-nitro-L-arginine methyl ester (L-NAME) leads to development of arterial hypertension (24,25). Studies in both humans and animals show that the restoration of NOS activity by administration of NOS cofactors such as tetrahydrobiopterin (BH4) or L-arginine result in increased bioavailability of NO, improved endothelial function, and prevention of hypertension (26,27).
 smooth muscle relaxation and inhibits platelet aggregation (29). Endothelin, another endothelium-derived agent, on the other hand, has a potent vasoconstrictor effect and may act alone or in concert with other agents such as thromboxane A2 (TXA2), prostaglandin F2α (PGF2α), or endothelial-derived constrictor factor (EDCF) to cause vasoconstriction. The relative amounts of the various factors released by the endothelial cell are kept in a tight equilibrium and are dependent on the physiologic circumstance and pathophysiologic status. Disturbance of this equilibrium can result in an acute hypertensive episode.
smooth muscle relaxation and inhibits platelet aggregation (29). Endothelin, another endothelium-derived agent, on the other hand, has a potent vasoconstrictor effect and may act alone or in concert with other agents such as thromboxane A2 (TXA2), prostaglandin F2α (PGF2α), or endothelial-derived constrictor factor (EDCF) to cause vasoconstriction. The relative amounts of the various factors released by the endothelial cell are kept in a tight equilibrium and are dependent on the physiologic circumstance and pathophysiologic status. Disturbance of this equilibrium can result in an acute hypertensive episode.Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree