INTRODUCTION
Hyperbaric oxygen (HBO) therapy involves breathing oxygen with the body exposed to an ambient pressure greater than that of sea level. HBO therapy results in the systemic delivery of oxygen that produces supraphysiologic oxygen tension in perfused tissues. The effects of HBO therapy are due to the combined effects of both increased ambient pressure and increased oxygen tension.1
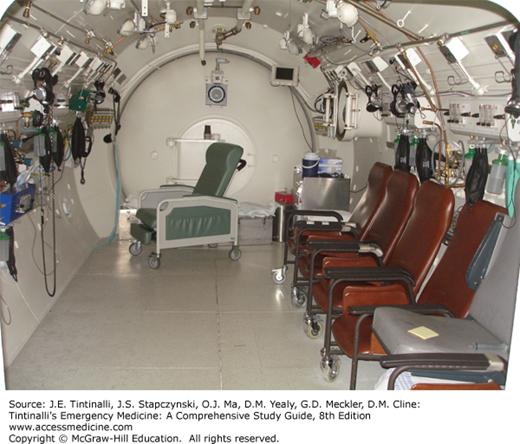
HBO therapy is delivered in a hyperbaric chamber. Monoplace chambers accommodate a single occupant and are typically clear, acrylic, plastic, cylindrical units with a door at one end (Figure 21-1). An attendant monitors the patient from the outside and communicates via intercom. Specially designed cardiopulmonary monitoring devices, intravenous infusion pumps, and ventilators enable critically ill patients to be treated in most monoplace chambers. Multiplace chambers can simultaneously treat multiple patients and will accommodate medical personnel inside the chamber (chamber tender or assistant) to perform hands-on patient assessment and care (Figure 21-2). Monoplace chambers generally use 100% oxygen for pressurization, whereas multiplace units are pressurized with air and patients breathe oxygen using tight-fitting facemasks, a hood, or endotracheal tube while inside. Most HBO chamber facilities have equipment and treatment protocols analogous to an intensive care unit.
Ambient pressure is an important concept in HBO therapy. At sea level, the pressure exerted by the air column (the atmosphere) above is quantified as 1 atmospheres absolute of pressure (1 ATA), 14.7 lb per square inch, 760 mm Hg, or 760 torr. Once a patient is placed inside a chamber, the ambient pressure is increased by the gradual inflow of compressed gas, either oxygen or air. Most HBO therapy takes place with an ambient pressure between 2.0 and 3.0 ATA.
In hyperbaric and diving medicine, the increased ambient pressure was originally described as of feet of sea water (fsw) or meters of sea water (msw) for both HBO treatment and during scuba diving. One atmosphere is equal to the pressure exerted by 33 fsw (10 msw), so starting at sea level, the ambient pressure is 1 ATA, and at a depth of 33 fsw, the ambient pressure would be 2 ATA. Describing an HBO treatment at either 2 ATA or 33 fsw communicates equivalent pressure.
A typical HBO treatment lasts 90 to 120 minutes. The initial pressurization phase is done over 10 to 15 minutes to allow for equalization of pressures within the sinuses and middle ear as ambient pressure increases. Pressure is then maintained at the desired levels for 40 to 90 minutes, followed by depressurization over 5 to 10 minutes. In a monoplace chamber, the patient is surrounded by and breathes 100% oxygen during the entire treatment. If desired, air breaks are done for 5 to 10 minutes with the patient breathing air from a mask while in the chamber. In a multiplace chamber, the patient is surrounded by air during the entire treatment and breathes 100% oxygen via a face mask or hood. Air breaks in a multiplace chamber are accomplished by removing the mask or hood and breathing the surrounding air. HBO treatments are done using preset protocols that define the level of pressurization, duration of each individual treatment, the use of air breaks, and the number of individual sessions in a course of therapy.
GAS LAWS
The physics of HBO therapy are governed by the ideal gas laws. Boyle’s law states that for gases kept at a constant temperature, the volume of that gas is inversely proportional to the pressure exerted on it. If pressure doubles, then the volume is halved. Boyle’s law is the principal behind HBO treatment of decompression sickness and air or gas embolism—reducing the size of gas bubbles within tissues and circulation by increasing ambient pressure. Boyle’s law also explains the occurrence of pain in the sinuses and ears during pressurization and decompression, as trapped pockets of gas contract or expand as ambient pressure changes.
Gay-Lussac’s law states that at a constant volume (e.g., a hyperbaric chamber) the absolute pressure is directly proportional to the absolute temperature. This explains why the ambient temperature inside a chamber increases transiently as it is pressurized and cools with decompression.
Henry’s law specifies that the partial pressure of a gas dissolved in a liquid is proportional to the pressure exerted on that gas. HBO therapy increases the ambient partial pressure of oxygen (PO2), producing an increase in the amount of dissolved oxygen carried by the blood. A patient in a hyperbaric chamber compressed to 2 ATA (equivalent to a diver at 33 fsw) breathing 21% oxygen is exposed to a PO2 of 320 mm Hg, twice the PO2 at ambient pressure before starting the treatment. Although the percentage of oxygen at 2 ATA is still 21%, the patient is inhaling twice as many molecules of oxygen with each breath. This is functionally equivalent to breathing 42% oxygen at sea level or 1 ATA.
The oxygen content of the blood is the sum of the oxygen carried by hemoglobin and oxygen dissolved in the plasma. Hemoglobin becomes fully saturated around a PO2 of 100 mm Hg; fully saturated hemoglobin carries approximately 20 mL of oxygen per 100 mL of blood, which is expressed as 20 vol%. At 1 ATA breathing room air, dissolved oxygen in the plasma is typically only 0.3 vol%. At a pressure of 3 ATA inside an HBO chamber pressurized with 100% oxygen, the arterial oxygen tension (PaO2) will approach 2200 mm Hg, which will bring the dissolved oxygen content up to about 5.4 vol%.2 This amount of dissolved oxygen can sustain basal metabolic functions in the complete absence of hemoglobin.
PHYSIOLOGIC EFFECTS
HBO therapy should be viewed as a drug and the hyperbaric chamber as a delivery device. HBO affects tissues in two ways: there are effects related to mechanical forces of increased pressure and effects due to hyperoxygenation. Of the two, elevating tissue oxygen tension is the primary effect.
Hyperoxygenation induces the formation of reactive oxygen species (superoxide, hydrogen peroxide, hypochlorous acid, and hydroxyl) and reactive nitrogen species (primarily nitric oxide). Levels generated during HBO therapy have beneficial effects seen after tissue oxygen levels return to normal (Table 21-1). Reactive oxygen species are natural byproducts of metabolism that can oxidize proteins and membrane lipids, damage DNA, and mediate tissue and organ damage seen in oxygen toxicity. The body has scavenger antioxidant systems to reverse the oxidative damage caused by reactive oxygen species generated during a typical HBO treatment of about 2 hours, so that oxygen toxicity is rare.
Inhibit microbial endotoxin and exotoxin production Enhance oxygen-dependent transport of antibiotics across cell walls Improve neutrophil oxygen-dependent peroxidase bactericidal activity Induce vasoconstriction that reduces posttraumatic tissue edema Stimulate angiogenesis by promoting the production of oxygen-dependent collagen matrix Promote wound healing by amplifying oxygen gradients at the periphery of ischemic wounds Blunt endothelial ischemia-reperfusion injury |
INDICATIONS
The Undersea and Hyperbaric Medical Society has defined clinical indications for HBO therapy, some of which are within the scope of emergency medicine practice (Table 21-2).3
Arterial gas embolism with neurologic symptoms* Decompression sickness* Carbon monoxide poisoning* Crush injury, compartment syndrome, and other acute traumatic ischemias* Exceptional blood loss anemia* Delayed radiation injury (osteoradionecrosis and soft tissue) Compromised skin grafts and flaps Acute thermal burns* Arterial insufficiencies (enhancement of healing in selected problem wounds, central retinal artery occlusion) Necrotizing soft tissue infections* Clostridial myonecrosis (gas gangrene)* Osteomyelitis (refractory) Intracranial abscesses |
Air or gas embolism can occur as a consequence of a deep sea dive–related accident4 or as the result of a medical procedure.5 Iatrogenic air or gas embolism has been reported in association with cardiovascular, obstetric/gynecologic, neurosurgical, and orthopedic procedures, generally associated with disruption of a vascular wall.6 Nonsurgical processes reported to cause air or gas embolism include overexpansion during mechanical ventilation, hemodialysis, and after accidental opening of central venous catheters. Air or gas embolism can occur either on the venous or arterial side of the circulatory system.
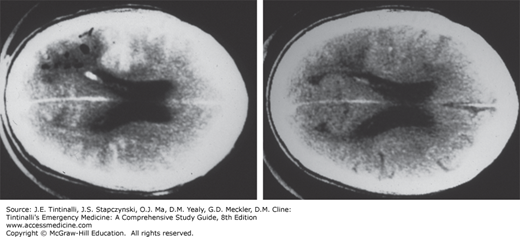
The consequences of an arterial gas embolism depend on location and magnitude of arterial occlusion. Often skeletal muscle, connective tissue, and skin can tolerate small emboli, but bubbles entering the coronary or cerebral arteries can precipitate acute coronary syndrome or stroke. Air entering the spinal cord circulation can produce weakness or paralysis. Any diver who surfaces with sudden onset of neurologic symptoms, such as confusion, speech difficulty, focal weakness, or paralysis, in less than 5 to 10 minutes should be assumed to have arterial gas embolism unless proven otherwise. Imaging with CT or MRI may help exclude an ischemic stroke or intracerebral hemorrhage. CT scan of the brain may show air in the cerebral vessels; however, this finding is variable and can be difficult to recognize (Figure 21-3).
Venous gas embolism is common after compressed-gas diving and surgical procedures.6 The amount of gas is typically small, and the bubbles are trapped in the pulmonary capillaries and resorbed without symptoms. Large quantities of gas in the pulmonary vasculature can stimulate cough, dyspnea, and pulmonary edema. A paradoxical arterial gas embolism may develop when a venous gas embolism travels to the arterial system by way of an intrapulmonary shunt or through an atrial septal defect or patent foramen ovale.
Administer oxygen to support arterial oxygenation and hasten bubble resorption. Place the patient in the supine position; there is no proven benefit to a head-down position to lower the risk of additional cerebral air embolization or a left lateral decubitus position to trap gas within the apex of the right ventricle and minimize migration. Catheter aspiration of trapped air in the right ventricle may be attempted in those rare instances when it is visualized.
HBO is recommended for air or gas embolism with neurologic or cardiovascular impairment.3 The faster the patient receives HBO, the greater is the chance for complete neurologic recovery. Various protocols are used for air or gas embolism. A standard one is Treatment Table 6 from the U.S. Navy Diving Manual, which uses compression to 2.8 ATA for 75 minutes (with three air breaks), following by decompression to 1.8 ATA for 150 minutes (with two air breaks) for a total treatment time of 285 minutes. For patients whose symptoms are not improved or worsen, a protocol using pressurization up to 6 ATA (Treatment Table 6A) is recommended. For patients with residual symptoms after the initial HBO treatment, additional treatments are recommended until there is no further neurologic improvement, typically one to two additional treatments.
Decompression sickness is due to the formation of nitrogen bubbles in body tissue and circulation during decompression (see chapter 214, “Diving Disorders”).7 During pressurization, inert gas (nitrogen if breathing air) is dissolved in body fluids. Upon reduction in ambient pressure, the dissolved gas comes out of solution and forms small bubbles in the tissue and circulation. HBO is an effective treatment because the increase in ambient pressure reduces gas bubble volume and the supplemental oxygen hastens inert gas diffusion out of the body.
Decompression sickness should be treated with HBO when such therapy is available and no contraindication exists. If HBO therapy is not available, patients with mild symptoms and neurologic stability for longer than 24 hours may be treated with supplemental oxygen therapy alone. If a patient must be transported by air to a hyperbaric facility, use pressurized aircraft to maintain sea-level pressure or transport at the lowest possible altitude in a nonpressurized craft, such a helicopter.
A variety of HBO regimens are used to treat decompression sickness,8 but most have in common pressurization to 2.8 ATA for 60 to 90 minutes, followed by stepwise decompression, similar to U.S. Navy Diving Manual Treatment Table 6. Most patients respond to a single treatment. Gas bubbles can persist for several days, and HBO may be beneficial even when begun after long delays.8
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree