Objectives/indications
Children often present to the emergency department with complaints regarding the head and neck. Such pathology affecting the head and neck involves infectious processes, anatomic abnormalities, and trauma. Only recently has point-of-care ultrasound been applied to the diagnosis of pathology affecting the head and neck.
Point-of-care ultrasonography may be applied to various pathologic processes in the head and neck, including ocular, neck masses, peritonsillar abscesses, and sinusitis. Ophthalmologists have utilized ocular ultrasound since the 1950s. With ultrasound, numerous processes can be identified. This includes but is not limited to vitreous hemorrhage, retinal detachment, globe rupture, and foreign bodies. Ocular ultrasound may also be used as an indirect measurement of intracranial pressure.
In addition, children of all ages often present with various neck masses. The identification of the neck mass is integral to the proper management and treatment of these patients. However, it is often clinically difficult to distinguish an enlarged lymph node from an abscess or a congenital anatomic abnormality. Older children may present with signs and symptoms suggestive of a peritonsillar abscess. However, it may be difficult to distinguish an abscess from peritonsillar cellulitis. Further, given the proximity to the vessels, it is imperative to identify a fluid collection prior to incision and drainage. Lastly, there is some role for ultrasonography in identifying sinusitis. In the future, there is potential for point-of-care ultrasound to augment or even eventually replace other diagnostic modalities such as tomography, MRI, or radiographs, which involve radiation and/or extensive cost and resources.
Ultimately, the application of point-of-care ultrasound is still evolving for pathology involving the head and neck. This chapter reviews existing literature for each application, and the technique to perform these examinations.
Ocular Ultrasound
Background
The evaluation of the pediatric eye can be challenging for clinicians, particularly in the setting of trauma. Given the fluid-filled nature of the eye and superficial location, ultrasonography is ideal in detecting both normal anatomy and pathology. Ocular ultrasound offers the unique ability to evaluate all key structures of the eye, with minimal cooperation from the patient. It can be utilized to detect globe rupture, the presence of foreign bodies, and may also be useful in the evaluation of intracranial pressure. Particularly in settings where an ophthalmologist may not be available to evaluate a patient emergently, ocular ultrasound may be used as a screening tool to evaluate those patients that require emergent evaluation versus those patients who can be seen in the next 24 hours.
Ocular ultrasound is a tool that has historically been utilized by ophthalmologists in the diagnosis of ocular pathology and disease processes. The use of ocular ultrasound by emergency physicians was first described in 2000 for the diagnosis of globe rupture and vitreous detachment in adult patients. Since then, several small case series of adult patients have suggested the utility of point-of-care ultrasound for patients with other ocular pathology, including vitreous hemorrhage, retinal detachments, globe rupture, central retinal artery and vein occlusion, lens dislocation, retrobulbar hematomas, and foreign bodies. Blaivas et al. studied emergency department patients with a history of eye trauma of acute visual change. Their results showed a sensitivity of 100%, specificity of 97.2%, PPV of 96.2%, and an NPV of 100% in diagnosing ocular pathology. This pathology included penetrating globe injuries, retinal detachments, central retinal artery occlusion, lens dislocation, vitreous hemorrhage, and vitreous detachment. Emergency sonologists were in agreement with the criterion standard in 60 of the 61 cases.
Another use of ocular ultrasound has been optic nerve sheath diameter (ONSD) measurements as a surrogate marker for the diagnosis of elevated intracranial pressure. A positive correlation has been shown between optic nerve sheath diameter and intracranial pressure as measured by an invasive monitoring device. Point-of-care ultrasound may have a role as a screening test for elevated intracranial pressure in patients with traumatic brain injury, as the specificity and negative predictive value were 100% in one study. In another study of patients with suspected elevated intracranial pressure, point-of-care ultrasound demonstrated a high sensitivity and specificity with an enlarged ONSD (>5 mm). There have also been several studies specifically addressing the use of ocular ultrasound in pediatric patients. In a case-control study of symptomatic patients with radiologic confirmation of elevated intracranial pressure (CT or head ultrasound), there was a highly significant difference in the ONSD in the case group compared to the control group. Le et al. evaluated patients with suspected increased intracranial pressure in the emergency department and intensive care unit. They used cut-offs as per established norms for ONSD of 4.0 mm in children of less than one year and 4.5 mm in children of one year and older. The gold standard to which the optic nerve measurement was compared was CT scan, ventriculostomy pressure, or lumbar puncture opening pressure. Using the measurements by the ophthalmic sonographers, the study found a sensitivity of 83% and a specificity of 38%. Interestingly, PEM physicians demonstrated the highest sensitivity at 96%, but poor specificity. This difference in sensitivity may be due to the fact that clinicians were not blinded to the signs and symptoms when performing ultrasound examinations. Further studies are needed in patients with blunt head trauma, intraventricular shunts and suspected shunt malfunction, and altered mental status. Point-of-care ultrasound may play a role as a screening tool in the initial assessment of patients presenting with multisystem trauma.
Anatomy
It is important to recognize the anatomic structures of the eye (Figure 8.1). The soft tissue of the eyelid surrounds the globe itself. The cornea, conjunctiva, iris, lens, anterior chamber, and posterior chamber are easily visualized by sonography. The posterior chamber consists of aqueous humor, retina, choroid, and sclera. At the posterior aspect of the globe is the retina, with the optic nerve exiting the eye posteriorly.
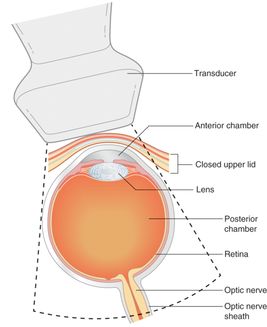
Figure 8.1 Anatomy of the eye. Important structures to become familiar with are the anterior chamber, lens, posterior chamber, retina, and optic nerve. Artwork created by Emily Evans © Cambridge University Press.
Technique
Point-of-care questions
Transducer selection and orientation
Ocular ultrasound is best performed with a linear-array, high-frequency transducer (5–10 MHz). The transducer should be applied gently to avoid pressure and trauma to the eye. The indicator should be oriented initially in the transverse plane (towards the patient’s right) and then the longitudinal plane (towards the patient’s head).
Patient position and preparation
When performing ultrasonography of the eye, particular attention should be paid to patient comfort. In addition, especially when considering a potential globe rupture, very minimal pressure should be placed on the eyelid itself. By resting the operator’s hand on the bony orbital rim, more control, and less pressure, will be transmitted to the eye. A copious amount of gel should be placed on the eyelid prior to performing ultrasonography (Figure 8.2a). Alternatively, it is often recommended to place a non-occlusive dressing over the closed eye. Care should be taken to remove all air between the non-occlusive dressing and the eyelid in order to reduce undesired artifacts. Ultrasound gel is then placed over the non-occlusive dressing to form an anechoic window for the sonographic evaluation of the eye.
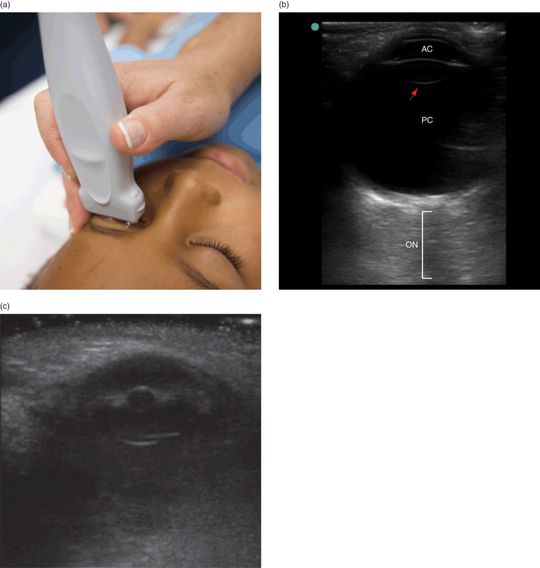
Figure 8.2 Ocular imaging. (a) Transducer placement on a closed eyelid. Note the copious amount of gel, and the clinician resting their hand on the orbital ridge in order to decrease the amount of pressure transmitted to the eye. (b) Ultrasound image of a normal eye, with the anterior chamber (AC), lens (arrow), posterior chamber (PC), optic nerve (ON).
Ultrasound imaging
Scanning through the entire span of the globe in each plane is important to identify pathology. If the patient is cooperative, it may be helpful to have the patient look up and down and side to side. It is important to optimize the gain settings, as too much gain will create hyperechoic artifacts, particularly in the posterior chamber of the eye. Conversely, too low a gain might lead to a missed vitreous hemorrhage or retinal detachment.
Ultrasound provides images of the eye from the globe anteriorly, extending posteriorly to the optic nerve (Figure 8.2b). The lid and cornea are echogenic structures, and the aqueous humor appears anechoic and fills the anterior chamber. In pathologic conditions, echoes may be seen within the aqueous humor. The anterior chamber is usually a shallow structure and, therefore, may not always be clearly visible by ultrasound. The lens of the eye appears as a hyperechoic, reflective, concave structure and, as such, may demonstrate reverberation artifact. The posterior chamber consists of vitreous humor, which, like the anterior chamber, appears anechoic. In pathologic conditions, internal echoes may be visualized here as well (Figure 8.3). Located most posterior are the retina, choroid, and sclera, which cannot be individually distinguished by ultrasound in a normal eye. In pathologic states, such as with retinal detachment (Figure 8.4), the layers may be distinguished. The optic nerve is located posterior to the globe, and appears as a hypoechoic, tube-like structure surrounded by hyperechoic retrobulbar fat. The vasculature of the eye is located parallel to and within the optic nerve, and can be visualized using color flow.
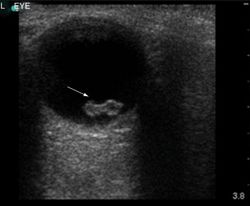
Figure 8.3 Vitreous hemorrhage (arrow). Image courtesy of Dana Sajed, MD.
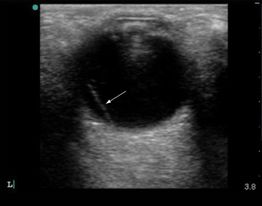
Figure 8.4 Retinal detachment (arrow). Image courtesy of Dana Sajed, MD.
Pathology
Increased intracranial pressure
The measurement of the optic nerve may be performed in order to indirectly evaluate for suspected increased intracranial pressure. For optic nerve measurements, the optic nerve should be aligned directly opposite the transducer, with the diameter width perpendicular to the vertical axis of the scanning plane. Measurement of the optic nerve sheath diameter is made 3 mm posterior to the globe (Figure 8.5). Both eyes should be measured, and the mean value used. The upper limit of normal for ONSD varies according to age (Table 8.1). Papilledema is considered when the mean value is greater than the limit for a child’s age (Figure 8.6a). A rare condition that may be mistaken for papilledema on both physical examination and ultrasonography is drusen, which involves the deposition of calcium at the optic nerve and creates shadowing posterior to the deposition (Figure 8.6b).

Figure 8.5 Optic nerve sheath diameter measurement. The width (B) measures 3.6 mm and is measured 3 mm posterior to the globe (A).
| Age (years) | Measurement (mm) |
|---|---|
| <1 | 4.0 |
| 1–15 | 4.5 |
| Adults | 5.0 |
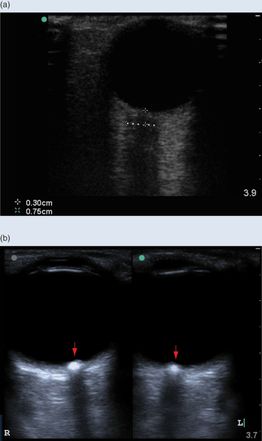
Figure 8.6 Papilledema. (a) Optic nerve sheath diameter measuring 7.5 mm, which is consistent with papilledema and increased intracranial pressure. (b) Rare condition mistaken for papilledema, called drusen, in which there is a calcification at the optic nerve.
Ruptured globe
Patients with potential globe rupture represent a particular diagnostic dilemma for emergency department physicians. While it is often difficult to diagnose with certainty by clinical examination, it is imperative to diagnose rapidly in order to facilitate operative intervention. The use of point-of-care orbital ultrasonography is an invaluable adjunct to the physical examination in these situations. In ocular trauma, a significant amount of pain, tearing, and orbital and periorbital swelling is often present, further limiting the feasibility of visual inspection. In contrast, orbital ultrasonography is not limited by the degree of soft tissue swelling and edema. Further, it can be performed on a closed eyelid, and can rapidly be performed at the bedside by the emergency physician.
Alternative imaging modalities include plain radiographs, CT scans, and MRI. When compared with ultrasound, each of these methods has significant limitations. Conventional radiographs only allow for the evaluation of major bony injury, and the sensitivity is exceedingly low for other diagnoses of concern as mentioned above. Magnetic resonance imaging is frequently unavailable for emergent cases, is time-consuming, and is contraindicated in the setting of potential metallic foreign bodies. A thin-section helical CT is often considered to be the optimal study, but it also requires patient stabilization and transport outside of the emergency department. Additionally, CT scans expose patients to ionizing radiation, which is of particular concern in pediatric patients. While point-of-care ultrasonography has been used in the diagnosis of globe rupture, controversy remains regarding the safety and theoretical increase in intraocular pressure with placement of the transducer on the eye. Recently, Berg et al. measured intraocular pressure during transducer placement in healthy volunteers, showing only a small transient increase in intraocular pressure.
When performing ultrasonography of a patient with a suspected globe rupture, it is imperative that the clinician try to minimize the amount of pressure applied on the eye itself. This may be achieved by resting the operator’s hand on the orbital ridge, and applying a copious amount of gel to a closed eyelid. A globe rupture can be visualized as a decreased size of the globe itself, an asymmetric shape, and most notably a collapsed anterior chamber (Figure 8.7). Both the affected and the unaffected eye should be scanned for comparison.
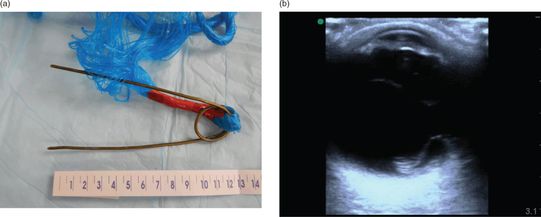
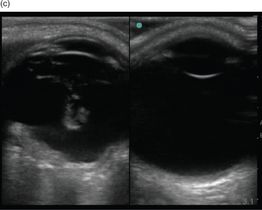
Figure 8.7 Ruptured globe. (a) Object suspected to have punctured a patient’s eye. The physical examination was unclear as to whether there was rupture, as the patient had a normal pupil and gross vision was intact. (b) Ultrasound image showing a flattened anterior chambter, hyperechoic regions within the globe, and posterior retinal detachment. (c) Patient with a bullet through his eye. Both eyes are imaged for comparison. The eye on the left side of the image exhibits retinal detachment and globe rupture. Note the decreased overall size, irregularity, and decreased anterior chamber size when compared with the contralateral eye.
Ocular foreign bodies
Ocular foreign bodies can be metallic, glass, plastic, or wood. They usually become embedded in the conjunctiva or cornea, and are easily appreciated on direct examination. However, occasionally foreign bodies may be small or penetrate deeper through the cornea (Figure 8.8). Ocular foreign bodies can lead to globe rupture, infection, retinal toxicity, and ultimately vision loss. CT scan is the first-line imaging modality of choice. A CT scan can detect metal foreign bodies greater than 1 mm in size. It is also sensitive in detecting glass foreign bodies greater than 1.5 mm in size. However, non-radiopaque materials such as wood are difficult to detect on CT.
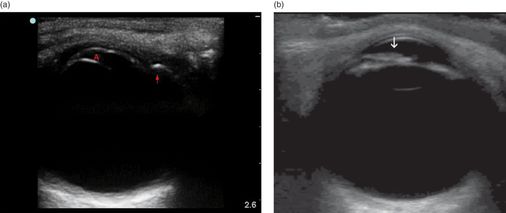
Figure 8.8 Ocular foreign bodies. Glass (arrow) embedded deeply into the cornea, which also led to a globe rupture. Note the small size of the anterior chamber (A).
Hyphema
A common condition in children is blood in the anterior chamber, or a hyphema. While ultrasound imaging is limited due to the shallow nature of the anterior chamber, a hyphema can be visualized as hyperechoic material within the anterior chamber (Figure 8.8b).
Scanning tips
Pitfalls
- Too little or too much gain can lead to false-negative or false-positive findings.
- Point-of-care ultrasound may not be efficacious in examining the anterior chamber of the eye.
- Controversy exists regarding the application of a transducer on the eye with suspected globe rupture.
Tips to improve scanning
Neck Masses
Background
The evaluation of soft tissue neck masses is an important skill in pediatric point-of-care ultrasound, as neck swelling and neck masses are a common complaint, and there are several considerations in the differential diagnosis. Neck masses may be a result of congenital, neoplastic, inflammatory, or infectious conditions. Specifically, it is important to distinguish between surgical and non-surgical diagnoses. In addition to lymphadenopathy and lymphadenitis commonly seen in adult patients, pediatric patients can also present with embryologic remnants previously undiagnosed, which may become acutely enlarged or superinfected. Ultrasound may be used as a first-line modality for the evaluation of these lesions, and in many cases may obviate the need for further imaging.
Ultrasound has been a longstanding first-line imaging tool for radiologists in the evaluation of pediatric neck masses. Radiologists have described the characteristic appearance of inflammatory and non-inflammatory cystic and solid lesions seen in the pediatric neck. Although no studies specific to emergency point-of-care ultrasound for the evaluation of neck masses have been published, there are descriptions in the literature that point-of-care ultrasound is a useful tool for non-radiologists, such as office-based otolaryngologists.
Anatomy
The regions of the neck can be divided into the following scanning areas: the thyroid gland, the paravascular spaces, the anterior and posterior cervical triangles, the supraclavicular fossae, and the major salivary glands. It is important to understand the normal anatomy of the neck before recognizing pathology that may arise in these areas (Figure 8.9a,b).
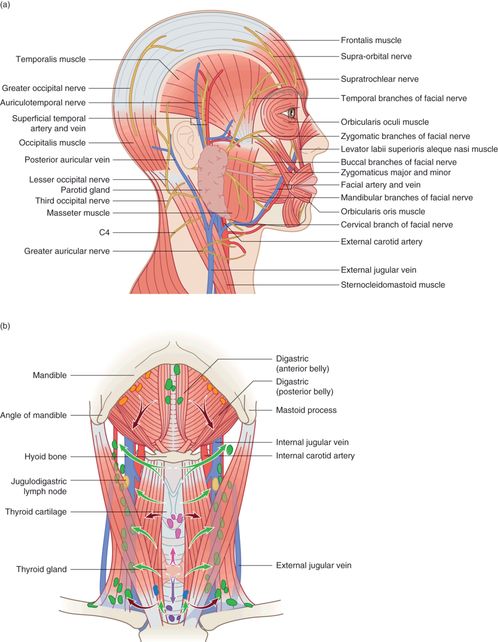
Figure 8.9 Anatomy of the neck. (a) Areas of the neck can be divided into: the thyroid gland, the paravascular spaces, the anterior and posterior cervical triangles, the supraclavicular fossae, and the major salivary glands. (b) Distribution of lymph nodes and lymphatic drainage of the head and neck. Artwork created by Emily Evans © Cambridge University Press.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








