INTRODUCTION AND EPIDEMIOLOGY
Heat emergencies represent a continuum of disorders from heat cramps to heat stress that, when severe, culminate in heat stroke. In most circumstances, heat emergencies can be avoided through common sense, public education, and prevention.
The incidence of heat-related emergencies varies with the weather, although this is not an absolute requirement.1 During heat waves and severe droughts, fatality rates spike.1 Heat stroke is likely seen less among persons who live in warmer climates than travelers to these areas because of physiologic acclimatization and cultural adaptation of the former to heat.
From 1999 to 2003, an average of 688 heat-related deaths per year from exposure to extreme heat were reported in the United States.1 The heat wave during the summer of 2003 is estimated to have caused 14,800 deaths in France.2 In the Russian heat wave in July/August 2010, there were an estimated 15,000 deaths, with additional morbidity from associated forest fires and smoke injury.3
PATHOPHYSIOLOGY
Body temperature is regulated through the delicate balance of heat production, accumulation, and dissipation. Heat is generated by cellular metabolism and the mechanical work of skeletal muscle. Heat accumulates from radiation from the sun and direct contact with hot objects and is absorbed when the ambient temperature rises above body temperature. As core temperature rises, the autonomic nervous system is stimulated to promote sweating and cutaneous vasodilatation.
The body has several mechanisms for dissipating heat to the environment, including radiation (the transfer of heat by electromagnetic waves from a warmer object to a colder object), conduction (heat exchange between two surfaces in direct contact), convection (heat transfer by air or liquid moving across the surface of an object), and evaporation (heat loss by vaporization of water, or sweat).
Radiation and evaporation dissipate most body heat at lower ambient temperatures (<35°C [<95°F]). Conduction of heat into a layer of ambient air surrounding the skin ends rapidly as soon as that layer acquires similar temperature as the skin surface. This results in creation of an “insulator zone” of warmed air through which little heat may be lost. Removing the warmed air next to the skin and replacing it with cooler air may increase conductive heat loss by convection. When conduction is coupled with convection, rates of heat energy transfer from the body increase. Conduction of heat into water is many times more efficient than conduction into air of the same temperature.
The effect of wind on heat loss depends on wind velocity. Wind moves heat away from the skin by convection, but above 32.2°C (90°F) and 35% humidity, convection does not remove heat well.4 This is why the use of fans alone is not effective in preventing heat stroke during periods of high environmental temperature and humidity.
When the external temperature rises to >35°C (>95°F), the body can no longer radiate heat to the environment and becomes dependent on evaporation for heat transfer. As humidity increases, the potential for evaporative heat loss decreases. Sweat that drips from the skin does not provide any cooling benefit and only exacerbates dehydration. As a result, the combination of high temperature and high humidity essentially blocks the two main physiologic mechanisms that the body uses to dissipate heat.
The body maintains a core temperature between 36°C and 38°C (96.8°F and 100.4°F). Native thermal regulation mechanisms begin to fail at core temperatures of <35°C (<95°F) and >40°C (>104°F).5 It is possible to maintain core temperatures of 40°C to 42°C (104.0°F to 107.6°F) for short periods without adverse effect.5
The physiologic response to heat stress consists of four primary mechanisms: dilatation of blood vessels, particularly in the skin; increased sweat production; decreased heat production; and behavioral heat control. As the core temperature of the body rises, the sympathetic outflow of the posterior hypothalamus is inhibited, which leaves unopposed the sympathetic outflow from the anterior hypothalamus. Sympathetic flow from the anterior hypothalamus results in decreased vascular tone throughout the body, particularly in the cutaneous circulation.
During exercise in conditions of hyperthermia, the heart rate increases to compensate for the decrease in stroke volume from the cutaneous vascular dilation and to maintain cardiac output.6 Patients with underlying cardiovascular disease or pharmacologic or physiologic impairment of these mechanisms may not be able to elevate cardiac output. Heat stress may also result in arrhythmias, myocardial ischemia, and exacerbation of congestive heart failure.
Elevated cholinergic stimulation to the skin results in increased sweat production. Sharp increases in the rate of sweat production normally occur with core temperature elevations above 37°C (98.6°F). As a general rule, for every pound of weight lost by sweating, 500 mL of fluid should be consumed. Endurance athletes can perspire at a rate of up to 1.5 L/h.7 Cutaneous vascular dilation and sweating increase as the body temperature rises until a homeostatic stall of heat production and input with heat dissipation is reached and the body’s temperature stops rising.8 Interestingly, sweating activation in older individuals begins at 1.5°C (34.7°F) higher than that in younger individuals.9
Medications often interfere with heat-removal mechanisms. NoTable drugs are anticholinergic agents, diuretics, phenothiazine, β-blockers, calcium channel blockers, and sympathomimetic agents.10 Anticholinergic agents impair sweating and the cardiovascular response to heat. Diuretics lead to volume depletion and decreased cardiac output. Phenothiazines have anticholinergic properties and deplete central stores of dopamine, which interfere with the hypothalamic thermoregulatory center. Medications such as β-blockers and calcium channel blockers decrease the cardiovascular response to heat and reduce peripheral blood flow and the ability to sweat. Sympathomimetics cause cutaneous vasoconstriction and inhibit sweating. Alcohol inhibits secretion of antidiuretic hormone, which leads to dehydration, and blunts the psychological heat-avoidance response. Heroin, cocaine, and amphetamines disrupt the function of endogenous endorphins and adrenocorticotropic hormones that are involved in heat adaptation mechanisms. Amphetamines and cocaine increase muscle activity and lead to heat production. Lysergic acid diethylamide and phencyclidine act on the CNS to induce a hypermetabolic state.10
Acclimation is the adaptation of the body to environmental changes. It involves a number of physiologic and biochemical adjustments that allow an individual to withstand heat stresses that would otherwise result in substantial morbidity and mortality.
Acclimation lowers the thermal set point in the hypothalamus, which triggers the onset of sweating at lower core temperatures in the acclimated human. In addition, the maximal rate of sweat production is dramatically increased to 1.5 to 3.0 L/h and can be sustained for longer periods.7 Aldosterone secretion is boosted, and sodium conservation results from more efficient reabsorption from the sweat. Plasma volume expands, heart rate decreases for any given heat load, and exercise tolerance improves. Dilation of cutaneous blood vessels occurs at a lower core temperature to promote earlier cooling.
In most individuals, acclimation can be achieved over 7 days to several weeks.11,12,13 Moderate exercise in a hot, dry environment for 60 to 100 minutes each day is probably the optimal approach to achieve acclimation. To maintain heat and exercise-induced adaptive responses, heat exposure needs to continue intermittently at least on 4-day intervals. Simple exposure to a hot environment for 1 to 4 hours a day also may result in acclimation within 2 weeks. Once removed from the hot environment, the body will de-acclimate to the original physiologic parameters within 1 to 2 weeks.12
The pathology of heat stroke is not completely understood, and although heat stroke is triggered by hyperthermia, there is evidence that secondary endotoxemia triggers a systemic inflammatory response, coagulopathy, and multiorgan failure.14,15
Heat exhaustion and heat stroke occur when the body’s thermoregulatory responses are impaired or overwhelmed and are no longer capable of maintaining homeostasis. Excessive heat is directly toxic to cells, causes an acute-phase reaction with release of inflammatory cytokines, and damages vascular endothelium. Nearly all cells respond to sudden heating by producing heat stress proteins, whose mechanism of action is still not completely understood.14,15
Escalating cellular temperature results in denaturation of proteins, interruption of cellular processes, and cell death. Temperatures of >41.6°C (>106.9°F) can produce cellular injury in hours. As temperature rises, cellular damage occurs more quickly and extensively. Temperatures >49°C (>120.2°F) typically result in immediate cell death and tissue necrosis.15 The enhanced vascular permeability due to damaged vascular endothelium results in activation of the coagulation cascade and disseminated intravascular coagulation.
Classic heat injury occurs during periods of high environmental heat stress. Physical exertion is not required if the heat gain occurs at environmental temperatures and humidity levels that overwhelm the native heat loss mechanisms. The increase in core temperature seen in this setting is often slow, occurring over a period of hours to days. Because of this slow rise in heat burden, volume and electrolyte abnormalities are common. High-risk populations include the elderly, the young, and those with psychological, physiologic, and pharmacologic impairments of heat loss mechanisms (e.g., diabetes; Raynaud’s disease; drugs such as anticholinergics, diuretics, antipsychotics, cocaine). Epidemiologic studies of classic heat injury typically identify the elderly, living alone or without social support and without air-conditioning.16
Exertional heat injury usually affects individuals who are participating in athletic events or performing jobs under conditions of high heat stress. Risk factors include dehydration, concurrent illness, obesity, wearing too much clothing, and poor cardiovascular fitness. In this setting, heat production and heat gain from the environment exceed the capacity of heat removal processes. Physical exercise is the most common single source of internal heat production. Without an efficient cooling mechanism, progressive dehydration and hyperpyrexia continue to the level of cardiovascular and metabolic failure.
Confinement hyperpyrexia is a special category of nonexertional hyperpyrexia and can occur in several circumstances, such as when children are left inside cars, when stowaways are abandoned inside closed vehicles or railroad cars, and when workers are occupationally exposed to heat inside enclosed spaces. Between July 2000 and June 2001 in the United States, 1960 nonfatal heat injuries and 78 fatalities were reported in children who were left intentionally in motor vehicles during hot days.17 Nonventilated vehicle compartments in a hot environment may reach temperatures of 54°C to 60°C (129.2°F to 140.0°F) in <10 minutes.17 Infants have less capacity than adults to deal with heat stress and, if left in motor vehicles for only a matter of minutes, may accumulate a critical heat burden. During 2000, nearly 500 individuals died attempting to cross the Mexico-U.S. border through the desert, locked in closed vehicle compartments and then abandoned by smugglers, with >50% of these deaths due to heat stroke. A particularly dangerous region is southern Arizona, which accounts for 22% of all southwest border deaths of illegal immigrants. In the August 2003 heat wave in France, a risk factor for heat stroke mortality was heat exposure at home or in a non–air-conditioned healthcare facility.18
CLINICAL FEATURES AND TREATMENT
Heat emergencies comprise a range of disorders from minor (heat edema, prickly heat, heat cramps, and heat exhaustion) to major (heat stroke).
Heat Edema Heat edema is a self-limited process manifested by mild swelling of the feet, ankles, and hands that appears within the first few days of exposure to a hot environment. Heat edema is due to the cutaneous vasodilatation and orthostatic pooling of interstitial fluid in gravity-dependent extremities. An increase in the secretion of aldosterone and antidiuretic hormone in response to the heat stress contributes to the mild edema. In general, heat edema is found in elderly nonacclimatized individuals who are physically active after a period of sitting while traveling in a vehicle or airplane. Occasionally, heat edema occurs after prolonged standing. It is commonly seen in healthy travelers just arriving from a colder climate. The edema is mild and does not impair or interfere with normal activities. Very rarely, pitting edema of the ankles may develop but does not progress to the pretibial region.
History and physical examination are usually sufficient to exclude systemic causes of edema, and no further testing or treatment except removal from heat source is needed. In the elderly, new pedal edema from heat should be differentiated from early congestive heart failure or deep venous thrombosis. Heat edema usually resolves spontaneously in a few days. No special treatment is necessary, but elevation of the legs and the use of support hose facilitate removal of the interstitial fluid. Diuretics are not effective and can predispose to volume depletion, electrolyte abnormalities, or more serious heat emergencies.8
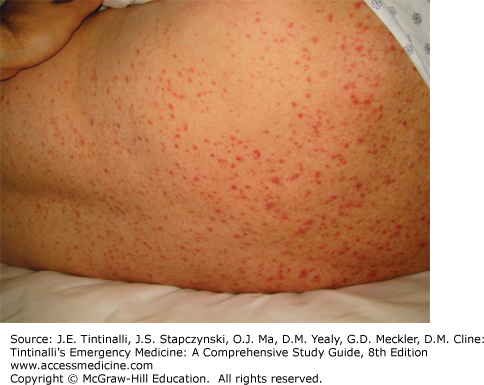
Prickly heat is a pruritic, maculopapular, and erythematous rash over normally clothed areas of the body. Also known as lichen tropicus, miliaria rubra, or heat rash, it is an acute inflammation of the sweat ducts caused by blockage of the sweat pores by macerated stratum corneum (Figure 210-1). The sweat ducts become dilated under pressure and ultimately rupture, producing superficial vesicles in the malpighian layer of the skin on a red base. Itching is the predominant clinical feature during this phase and can be treated successfully with antihistamines. Wearing clean, light, and loose-fitting clothing and avoiding sweat-generating situations can prevent prickly heat. Calamine lotion or topical steroids can be of benefit. Chlorhexidine in a light cream or salicylic acid cleaning may provide some relief.19
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree