Healthy Growth and Development of the Newborn/Infant
Renee Dellarose Kimball MD
INTRODUCTION
The first year of a child’s life is one of the most exciting periods of growth, development, and exploration both for infant and parents. It is an exciting time of “firsts.” The primary care provider is seen not only as the physical expert but also as an expert in mental health, development, parenting, and other psychosocial issues. Most of the questions parents bring to the primary care provider during office visits concern psychosocial or “nonillness” issues. The expectation that primary care providers are sources of information, support, and understanding for psychosocial and developmental concerns mandates that the health professions produce primary care providers who are adept and comfortable responding to and counseling parents about such issues.
GROWTH AND DEVELOPMENT
A discussion of “normal” must consider an individual’s variability throughout the day or week and according to culture. Individual variability means the individual’s different responses as he or she adapts to environmental changes. An example of individual variability to environmental stimuli can be seen when comparing an introverted child’s quiet withdrawal in social situations to an extroverted child’s attention-grabbing antics. Cultural variability is vast and includes philosophy, expectations, and traditional practices. A classic example of cultural variability is an Asian family investigated for child abuse when marks are noted on a child’s back that are a result not of abuse, but of the tradition of “cupping” to rid disease. Thus, what is normal must be interpreted in the context of each particular individual in each particular environment.
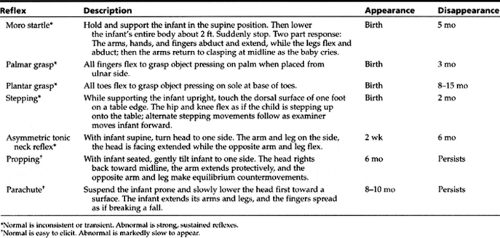
Although all children go through orderly, predictable sequences of neurodevelopment and physical growth, both intrinsic and extrinsic factors make each baby unique. Gross generalizations can be made to help illustrate the child’s progress during this time. Physical growth changes depending on stage of life. Prenatally, the growth of the head predominates, reaching the peak in the third trimester. The mother’s prepregnancy weight and pregnancy weight gain and placental function and gestational age at birth primarily determine the infant’s birth weight. During infancy, the growth of the trunk predominates, and weight gain continues at a rapid but less steep rate. Fat content in infancy accelerates until approximately age 9 months. Development progresses from generalized reflexes to stimuli (Table 8-1), to voluntary discrete actions that are asymmetric and precise toward stimuli (eg, grasping with one hand and examining with the other). Developmental control progresses from cephalad to caudal and proximal to distal. Development also progresses from dependence to independence.
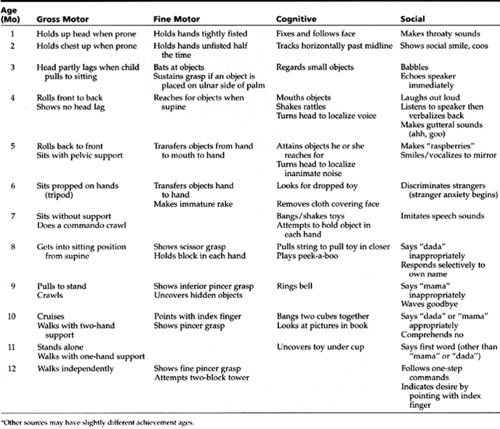
Development frequently is divided into four categories for discussion: gross motor, fine motor, cognitive, and social. Table 8-2 outlines the common milestones for each category and their expected age of mastery. Social development varies most because it depends more on environmental than genetic factors and represents the steps necessary to form interpersonal relationships. Delays in achieving milestones should be assessed in the context of the domains affected. One mild delay affecting only one domain may be monitored carefully, while delays affecting several domains are more worrisome. Development delayed 30% from expected norms should prompt referral for formal evaluation (Johnson & Blasco, 1997). The scope of developmental pediatrics encompasses not only motor skills, but also the mental, sensory, and emotional function of a child. Parents are not reliable historians for retrospective development but are highly reliable for current accomplishments.
• Clinical Pearl
A delay in achieving milestones does not always indicate an abnormality, because there is no age at which failure to achieve a skill is abnormal. Most late talkers and walkers turn out to be normal. Likewise, achieving a milestone at a given time does not always indicate normalcy. A child with cerebral palsy or Down syndrome may meet early milestones on or ahead of schedule. Developmental testing is not a substitute for the physical examination. Testing is merely an adjunct to aid in forming a complete picture about the patient.
HISTORY AND PHYSICAL EXAMINATION
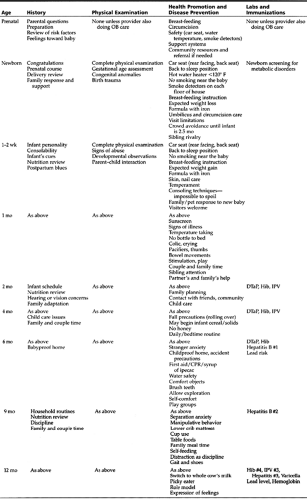
The purpose of the periodic scheduled well child visit is the promotion of wellness and the prevention of disease through anticipatory guidance, evaluation of growth and development, and immunizations. The American Academy of Pediatrics (AAP) recommends a preventive health care schedule for healthy, appropriately growing and developing children. If a child is not well physically or developmentally, more frequent and sophisticated visits are required. The recommended schedule for well child visits and immunizations is summarized in Table 8-3.
History
History taking and anticipatory guidance during the first year should concentrate on general health since the last visit, prevention of injury and illness, nutrition, infant care issues, parent–infant interactions, family relationships, community interactions, and any parental concerns. A wealth of evidence
supports the immense role the family plays in shaping a child’s physical, emotional, mental, and behavioral health. Family dysfunction is a strong risk factor for childhood disorders. Prenatal and postnatal visits may allow for observations that help identify families at risk. During all well child care visits, observation of the parent–child interaction is important. The parents’ manner of handling and holding the infant, their response to the infant’s discomfort, and their affect when speaking of the infant should be noted to identify maladaptive nurturing that contributes to health problems. Often stressors at home are seen in the office as somatic symptoms; in severe cases, this may present as failure to thrive. An emotionally deprived infant will not produce growth hormone, but once the infant is given attention that provides both physical and emotional warmth, growth begins again as growth hormone is produced.
supports the immense role the family plays in shaping a child’s physical, emotional, mental, and behavioral health. Family dysfunction is a strong risk factor for childhood disorders. Prenatal and postnatal visits may allow for observations that help identify families at risk. During all well child care visits, observation of the parent–child interaction is important. The parents’ manner of handling and holding the infant, their response to the infant’s discomfort, and their affect when speaking of the infant should be noted to identify maladaptive nurturing that contributes to health problems. Often stressors at home are seen in the office as somatic symptoms; in severe cases, this may present as failure to thrive. An emotionally deprived infant will not produce growth hormone, but once the infant is given attention that provides both physical and emotional warmth, growth begins again as growth hormone is produced.
Physical Examination
Before approaching the infant to do the physical examination, the primary care provider first should observe the infant at rest or play. The child should become acclimated to the primary care provider. A gentle, friendly approach with a quiet voice and interaction at the child’s level for both age and development are important. A complete physical examination with the infant unclothed is essential at each visit. The infant is examined in parts, with areas exposed and covered to avoid chill. The primary care provider progresses from areas needing a child’s cooperation (lungs) to painful or unpleasant areas (ears). The examining table is convenient, but a parent’s arms or lap will provide security for the young infant. The primary care provider should face the parent with the knees touching the parent’s to create a makeshift table on which the entire examination can be performed.
Neonate-Specific Considerations (Birth-30 Days)
The care of a new family ideally begins prenatally to help build rapport and to focus on the particular family’s concerns, fears, and desires regarding the upcoming birth. For a family that is new to the primary care provider’s practice, the prenatal visit also begins the relationship and provides an opportunity to foster trust in the primary care provider before birth. This is particularly important if a problem arises prenatally or perinatally, because establishing rapport is difficult in times of urgency or stress. This also is an opportune time to review the effects of environmental tobacco smoke on the fetus and on children in the home (Display 8-1) (AAP, 1997a).
DISPLAY 8–1 • Environmental Tobacco Smoke Hazards
Infants who live with smokers are doubly likely to have bronchitis or pneumonia in first 5 years of life.
They are four times more likely to be admitted for bronchitis and pneumonia.
They are 1.5 times more likely to have acute nasopharygitis and sinusitis in first 5 years.
Risk for recurrent otitis media during first year of life is significant.
Infants who live with smokers are 50% to 60% more likely to develop middle ear effusion requiring myringotomy and tubes.
Symptoms are more frequent and severe in asthmatic children who live with smokers.
Risk of SIDS is increased.
Infants who live with smokers have greater ratio of total cholesterol to high-density lipoprotein (HDL) and lower HDL levels by adolescence.
Risks for lung cancer, leukemia, and lymphoma as an adult are increased.
Source: American Academy of Pediatrics. (1997). AAP policy statement: Environment and tobacco smoke.
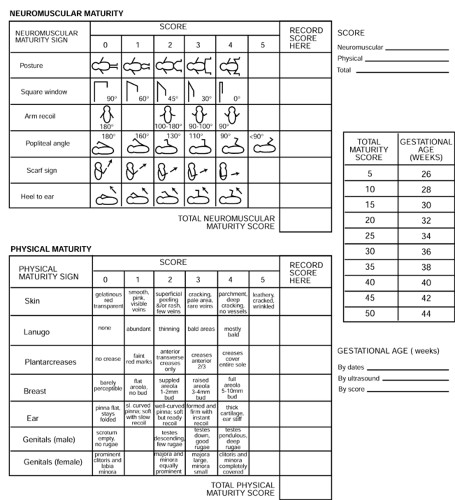
Gestational age is essential for evaluating whether an infant’s developmental progress and growth are appropriate and for predicting increased risks of morbidity or mortality. Gestational age also allows for a description of a newborn’s fetal growth pattern and size in three categories. Small for gestational age (SGA) is a weight percentile less than 10th, appropriate for gestational age is 10th to 90th percentile, and large for gestational age (LGA) is more than 90th percentile. SGA and LGA newborns are predisposed to increased risks, which are compounded further if such infants are born premature (< 37 weeks’ gestation) or postterm (> 41 weeks’ gestation). To this end, various scoring systems have been
developed to assess physical and neurologic signs of maturity. The Ballard exam (Fig. 8-1), a common tool used for this purpose, is accurate to within 2 weeks of assigned gestational age.
developed to assess physical and neurologic signs of maturity. The Ballard exam (Fig. 8-1), a common tool used for this purpose, is accurate to within 2 weeks of assigned gestational age.
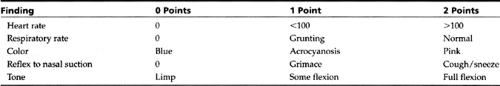
The APGAR score is unique to the newborn (Table 8-4); it indicates the newborn’s in utero, intrapartum, and immediate postnatal experience. It estimates the severity of respiratory and neurologic depression at 1 minute and 5 minutes of age. The 1-minute APGAR score is less predictive than the 5-minute score for residual neurologic damage. A cord-blood pH less than 7.20 is the direct measurement of perinatal asphyxia.
Vernix covers the infant at birth, protecting the baby from amniotic fluid. Vernix consists of sebum and cornified epidermis and is removed by the bathing process in the nursery. Lanugo is the fine silky hair seen on the newborn, particularly on the shoulders and back. It usually is shed by 10 to 14 days of life. Transient puffiness lasting 2 to 3 days, which has no identifiable cause, is of no concern and can be seen in the newborn’s eyelids, hands, feet, legs, pubis, genitalia, or sacrum.
Physiologic jaundice is due to numerous factors and is present in two thirds of infants by 48 hours after birth. Jaundice begins in the face and progresses caudally. It is most easily
seen in the sclera, particularly in dark-skinned infants. Jaundice that presents within the first 24 hours is pathologic and must be investigated appropriately to rule out hemolytic disease, liver disease, or severe infection. Newborns have an increased red blood cell mass per kilogram, shorter red blood cell life span, and an immature liver with decreased hepatic uptake and conjugation. Newborns also have decreased intestinal catabolization of unconjugated bilirubin and increased hydrolyzation of conjugated bilirubin to the unconjugated form. The result is more unconjugated bilirubin in the intestine for reabsorption. These combined factors result in increased enterohepatic circulation of bilirubin. Physiologic jaundice is associated with a relatively rapid increase in indirect bilirubin, which usually peaks at a mean unconjugated bilirubin of 5 mg/dL by 3 to 4 days and then declines to adult levels by 11 to 14 days (Gartner & Lee, 1999). The peaks and rate of resolution, however, vary by race and mode of feeding, suggesting that “normal” physiologic jaundice also may have to be interpreted within the context of an individual and situation. Bilirubin levels are the same from birth to 4 days in breastfeeding and formula-fed infants but diverge at 5 to 6 days. Bilirubin levels decline rapidly to adult levels in formula-fed infants, while they decline slower in breastfed infants, with two thirds of these infants having an elevated bilirubin level at 8 weeks (Gartner & Lee, 1999). African American and Caucasian infants reach a peak bilirubin level at 2 to 3 days, while Asian infants reach a peak at 4 to 5 days.
seen in the sclera, particularly in dark-skinned infants. Jaundice that presents within the first 24 hours is pathologic and must be investigated appropriately to rule out hemolytic disease, liver disease, or severe infection. Newborns have an increased red blood cell mass per kilogram, shorter red blood cell life span, and an immature liver with decreased hepatic uptake and conjugation. Newborns also have decreased intestinal catabolization of unconjugated bilirubin and increased hydrolyzation of conjugated bilirubin to the unconjugated form. The result is more unconjugated bilirubin in the intestine for reabsorption. These combined factors result in increased enterohepatic circulation of bilirubin. Physiologic jaundice is associated with a relatively rapid increase in indirect bilirubin, which usually peaks at a mean unconjugated bilirubin of 5 mg/dL by 3 to 4 days and then declines to adult levels by 11 to 14 days (Gartner & Lee, 1999). The peaks and rate of resolution, however, vary by race and mode of feeding, suggesting that “normal” physiologic jaundice also may have to be interpreted within the context of an individual and situation. Bilirubin levels are the same from birth to 4 days in breastfeeding and formula-fed infants but diverge at 5 to 6 days. Bilirubin levels decline rapidly to adult levels in formula-fed infants, while they decline slower in breastfed infants, with two thirds of these infants having an elevated bilirubin level at 8 weeks (Gartner & Lee, 1999). African American and Caucasian infants reach a peak bilirubin level at 2 to 3 days, while Asian infants reach a peak at 4 to 5 days.
Jaundice seen in breastfeeding infants may be described as either “early onset,” due to inadequate milk and calorie intake and representing an exaggeration of physiologic jaundice, or “breast milk” (“late onset,” “prolonged”) caused by not yet identified factors in transitional and mature milk. Early-onset breastfeeding jaundice may precede breast milk jaundice. Both processes result in increased enterohepatic circulation from increased intestinal bilirubin absorption. The AAP discourages the interruption of breastfeeding in healthy term newborns with early-onset breastfeeding or late-onset breast milk jaundice. Early-onset jaundice can be prevented by establishing optimal breastfeeding through frequent nursing (> 10 nursings in 24 hours) and careful observation to identify and correct any suckling difficulties. Taking the infant off the breast will result in decreased breast stimulation, a decreased milk supply, and continuation of the problem. Formula supplementation is not recommended unless the serum bilirubin is greater than 20 mg/dL or the infant is experiencing significant starvation or dehydration. These infants can continue to nurse at the breast while using a supplemental nursing system to obtain sufficient calories while continuing to suckle and stimulate breast milk production. A supplemental nurser is a device in which a bottle filled with formula is hung around the mother’s neck with one or two small, soft, pliable tubes attached to the end of the bottle with the other ends at the mother’s nipples. As the baby suckles at the breast, he or she also sucks on the tubes, thus receiving both breast milk and formula during a feeding. Glucose water supplementation is not indicated, because it does not decrease bilirubin levels (bilirubin is excreted through the stool, not the urine). It also negatively affects the volume of breast milk by interfering with nursing. These infants should be evaluated 48 to 72 hours after discharge from the hospital to ensure that successful breastfeeding has been established.
Infants who have breast milk jaundice may have elevated unconjugated bilirubin levels that persist for 3 to 4 weeks and sometimes up to 12 weeks of life. In the infant with prolonged hyperbilirubinemia, breast milk jaundice is a diagnosis of exclusion. Infants with breast milk jaundice are thriving, vigorous, and gaining weight appropriately without clinical or laboratory signs of disease. The peak bilirubin occurs between days 5 and 15 in these infants. Cessation of nursing will lead to a precipitous drop in serum bilirubin; however, this is not recommended, because the bilirubin concentration will decline on its own.
Prolonged hyperbilirubinemia has other causes besides breast milk jaundice that should be ruled out. These include hemolytic disease of the newborn; polycythemia; glucuronyl transferase defects; metabolic disorders, such as hypothyroidism and galactosemia; hematomas; and intestinal obstruction. Workup of a jaundiced infant often includes total, indirect, and direct bilirubin levels; complete blood cell count with peripheral smear; blood type, Rh, and antibody profile (mother and newborn); direct and indirect Coombs’; and reticulocyte count (>5% suggests hemolysis). Treatment levels are based on studies from Caucasian, formula-fed infants. The concern about neonatal jaundice stems from its action as a cell toxin that can be deposited in various tissues, ultimately causing necrosis of the cells. The evidence for kernicterus is based on studies of preterm, low–birth-weight infants or those with hemolytic disease. In determining the effect on normal term infants without hemolysis, several collaborative long-range studies were done. These studies found that hyperbilirubinemia had little or no effect on IQ, mental development, neurologic abnormality, speech, language, or hearing tests at least to a total serum bilirubin level of 20 in term babies without hemolysis. This does not mean that infants will not have toxicity due to bilirubin if they have other risk factors (eg, acidosis, hypoxia, anoxia, or sepsis). Treatment consists primarily of phototherapy when the total serum bilirubin reaches 15 to 20 mg/dL and can be discontinued when the total serum bilirubin drops below 14 to 15 mg/dL (Bland, 1996). Breastfeeding can continue throughout phototherapy. Phototherapy can be accomplished safely in the low-risk infant with a Wallaby blanket, even as an outpatient, to reduce adverse effects on breastfeeding, mother–infant relationship, and cost.
Considerations for All Infants (Birth-12 Months)
Growth charts of height, weight, and head circumference should be done at all well child visits to monitor ongoing
growth. Normal growth is one of the most reassuring findings during a well child examination, because it implies health, adequate nutrition and genetic makeup, and absence of major chronic disease. A pattern of growth abnormalities can help narrow the differential diagnosis of growth failure. Congenital, constitutional, familial, or endocrine causes of growth abnormalities appear as a decrease in the height curve before or at the same time as the decrease in the weight curve so that the weight-to-height curve is either normal or increased. Starvation initially appears as a decrease in weight and weight-for-height curves. In chronic starvation, there is a decrease in the height curve and possibly a return toward normal weight-for-height curve.
growth. Normal growth is one of the most reassuring findings during a well child examination, because it implies health, adequate nutrition and genetic makeup, and absence of major chronic disease. A pattern of growth abnormalities can help narrow the differential diagnosis of growth failure. Congenital, constitutional, familial, or endocrine causes of growth abnormalities appear as a decrease in the height curve before or at the same time as the decrease in the weight curve so that the weight-to-height curve is either normal or increased. Starvation initially appears as a decrease in weight and weight-for-height curves. In chronic starvation, there is a decrease in the height curve and possibly a return toward normal weight-for-height curve.
Measurements and Temperature
Length should be measured with the child in the supine position until he or she is 24 to 36 months. Birth lengths average 18 to 22 in (45–55 cm), and length increases 30% by age 5 months and 50% by the first birthday. Weight should be measured on an infant scale using ounces or grams. Birth weights average 5 lb 8 oz to 8 lb 13 oz (2500–4000 g), and weight generally doubles by 4 to 5 months and triples by 12 months. Based on Department of Health, Education, and Welfare growth charts with reference percentiles, a healthy term infant can be expected to gain approximately 1 oz/d for the first 3 months of life and 0.5 oz/d for the remainder of the first year. Weight often is considered the fifth vital sign in children. A weight that falls off the growth curve often is the first sign of a psychosocial or physical disorder. Head circumference should be measured at each visit until the child is 24 months old. Correct placement is essential for accurate data interpretation. The measuring tape should be placed snugly around the head at the occipital protuberance and the supraorbital prominence to find the largest circumference. Birth head circumferences average 13 to 14 in (33–35 cm) and are usually two thirds of adult size by age 2 years. Delayed growth suggests premature suture closure or microcephaly, while too rapid growth suggests hydrocephalus or intracranial mass. Chest circumference is not universally done.
Accurate measurement and monitoring of body size are especially important in infants, because deviations may be the first or only sign of disease, such as in chronic renal disease, hyperthyroidism, or parental deprivation syndrome. All infant measurements should be plotted on the appropriate growth curve for comparison with population means. The most important aspect of the growth curve is following the individual’s progress. Any curve within the 5th to 95th percentiles is “normal.” Values that begin to deviate from the infant’s growth curve history are of concern (ie, is the child falling off or rising above the curve). Growth parallel to but below the 5th or above the 95th percentile is more than likely normal; however, an increased prevalence of developmental disabilities associated with many genetic syndromes is found in these two groups. Knowing the stature of the parents is helpful when assessing deviation from the norm. Rectal temperature is the most accurate means of assessing core body temperature in infants.
• Clinical Pearl
The body temperature of infants and young children is more variable and higher than that of adults. In normal infants, the average rectal temperature usually does not fall below 99°F and may be as high as 101°F in the afternoon after a busy or anxious day. Conversely, young infants may have normal or subnormal temperatures even with severe infections.
Skin, Hair, and Nails
Newborns have very little subcutaneous fat at birth, a large body surface area, and an inability to shiver. Thus, they are predisposed to hypothermia. Infants lose four times more body heat per unit weight than adults do (Seidel et al., 1997). Body fat is only 12% at birth but increases fairly rapidly to 25% at 6 months and then less rapidly to 30% by 12 months. Infants also are at increased risk of dehydration due to high surface area, turnover rate, and relative amount of body water. Infants have 80% body water at birth; this amount does not drop to the adult level of 60% until after the first birthday.
Infant skin lacks coarse terminal hair and appears much smoother and softer than adult skin. Newborn skin also lacks appocrine function, and eccrine function does not begin until after the first month of life. Thus, infant skin is less oily than adult skin.
The color of an infant’s skin is inversely related to the amount of subcutaneous fat: the less fat, the more red and transparent the skin. Dark-skinned infants often appear less pigmented at birth than they will look when they are 2 to 3 months old. Skin color can be estimated by looking at the scrotum and nail beds.
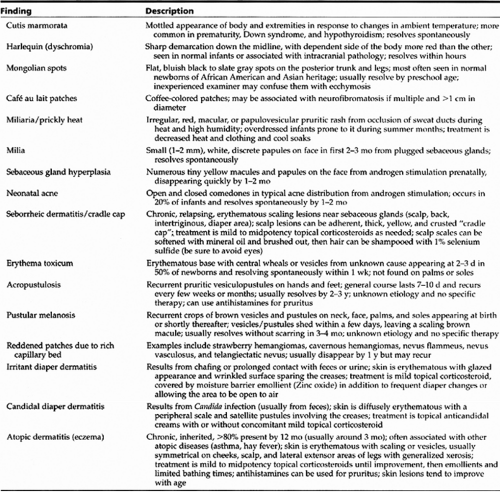
Acrocyanosis (cyanosis of the hands and feet) is normal in newborns and in older infants who are chilled. Central cyanosis should be investigated for an underlying cardiac defect. Other color and common neonatal and infant skin conditions are listed in Table 8-5.
Skin creases can give clues to maturity and are associated with certain abnormalities. The older the baby is, the more creases will appear on the palms and soles. One of the best known abnormal palmar creases is the Simian crease frequently seen in trisomy 21; however, it also may be seen in normal children.
Skin turgor should be inspected to assess nutritional and hydration states. Severe dehydration or malnutrition will result in prolonged skin tenting. Tenting in an infant is best observed by pinching a fold of skin on the abdomen or thigh.
No matter how much hair is on the infant’s head at birth, most hair is lost (transient plagiocephaly) by age 2 to 3 months and replaced by permanent hair. Permanent hair may be of a different texture or color than the birth hair.
Lymphatics
The infant’s immune system is immature at birth, leaving the baby vulnerable to serious infections during the first few months of life. This is true even though the amount of lymphoid tissue is greater than during adulthood. Lymph nodes usually are not palpable in infants but do respond briskly to mild stimuli, such as viral infections or infections in the associated drainage area (eg, otitis media), particularly in the cervical and postauricular chains. It is not unusual to find these nodes enlarged in children younger than 2 years. Generally, discrete, movable, and nontender nodes less than 1 cm in the cervical, axillary, or inguinal chains or less than 0.5 cm elsewhere are of little concern.
Head and Neck
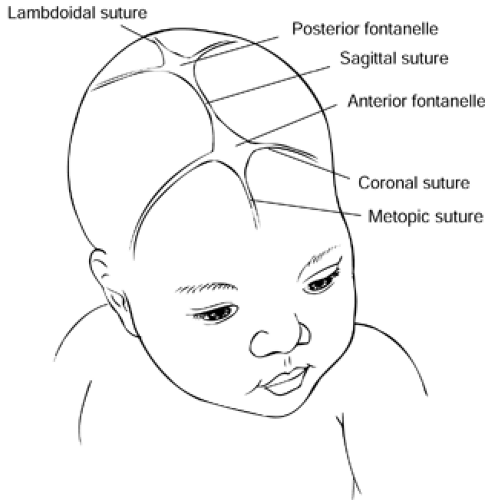
An infant’s skull consists of seven soft bones separated by sagittal, coronal, and lamboidal sutures. The sutures allow the skull to expand, permitting brain growth, and can be palpated as ridgelike lines until age 6 months. At this time, they usually become nonpalpable. The fontanelles are located at the intersection of the sutures and begin to ossify in the first year of life (Fig. 8-2). The fontanelles should feel
somewhat depressed and have minimal pulsation. The posterior fontanelle usually closes by 2 months; the anterior fontanelle may remain open until 18 to 24 months, though in 90% of infants it closes by 7 to 19 months. An anterior fontanelle that is greater than 4 to 5 cm in diameter or bulging with marked pulsation may indicate increased intracranial pressure, either from infection or hydrocephalus. This clinical sign, however, often is not present in infants younger than 3 months and thus should not be used to predict the presence of meningitis. Ultrasound of the skull is recommended in infants suspected of having an intracranial lesion or a rapidly enlarging head circumference on serial examinations.
somewhat depressed and have minimal pulsation. The posterior fontanelle usually closes by 2 months; the anterior fontanelle may remain open until 18 to 24 months, though in 90% of infants it closes by 7 to 19 months. An anterior fontanelle that is greater than 4 to 5 cm in diameter or bulging with marked pulsation may indicate increased intracranial pressure, either from infection or hydrocephalus. This clinical sign, however, often is not present in infants younger than 3 months and thus should not be used to predict the presence of meningitis. Ultrasound of the skull is recommended in infants suspected of having an intracranial lesion or a rapidly enlarging head circumference on serial examinations.
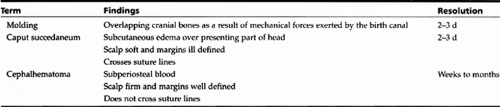
Birth-related findings can be identified during the newborn examination and are described in Table 8-6 and Figure 8-3. The head, face, and neck are inspected for shape, symmetry, and abnormalities that may give clues to congenital or chromosomal disorders. Asymmetry of the head, or a “flat spot,” is common in infants due to positioning, particularly because the “Back to Sleep” campaign has increased the number of infants who sleep in the supine position. If a thorough examination does not reveal any other abnormalities when a flat spot is found, parents should try changing the infant’s positions over a 4- to 6-week period (Liptak & Serletti, 1998). Position changes can be accomplished easily by alternating the infant’s line of vision to outside activities during supine sleeping (ie, turn the infant so that the head is at the other end of the crib). Prone positioning is encouraged during awake times to stimulate upper body strength and development and limit the time spent supine. If the asymmetry resolves, positional deformity is extremely likely, and no further workup is required. If the asymmetry persists, a
plain radiograph or computed tomography scan of the head should be obtained to examine the sutures, which should be patent.
plain radiograph or computed tomography scan of the head should be obtained to examine the sutures, which should be patent.
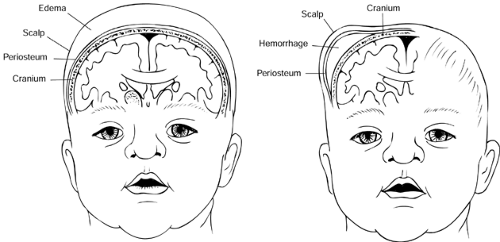 Figure 8-3 (A) Caput succedaneum. (B) Cephalhematoma. Note that the swelling does not cross suture lines. |
The neck should be inspected and palpated to check for muscle tone and masses. Torticollis may be present and is easily treated with physical therapy. A cystic mass in the upper neck may be a thyroglossal duct or branchial cleft cyst. A mass in the lower portion of the sternocleidomastoid muscle may represent a hematoma. A mass over the clavicle that changes size with respiration may be a cystic hygroma.
Eye
Infants are hyperopic when born, with visual acuity of 20/200 and a field of vision only about the distance from a cradled arm to a parent’s face. Visual acuity, dependent on nervous system maturation, continues to develop and matures enough for an infant to be able to discern colors by 8 months. Most children do not achieve 20/20 acuity until 6 years. Infants begin to have voluntary control of the eye muscles at 5 to 6 weeks but are unable to see a single image until around 9 months due to incomplete coordination. Visual acuity can be assessed through observation of the infant’s reaction to the environment (eg, focusing on a face, tracking objects, or responding to a bright light). Nystagmus in any direction is common at birth, but persistence after several days may indicate blindness. Infant lacrimal ducts begin carrying tears at 2 to 3 months. A blocked nasolacrimal duct is common and identified by constant tearing or accumulation of mucous material at the inner canthus. Most blocked ducts result from incomplete development. The majority of blocked ducts spontaneously open by age 6 months, while the remainder open by 12 months when development is complete. Massage of the sac (with or without a warm compress) at the root of the nose with the proximal end blocked may result in spontaneous opening of the duct. If the condition persists for more than 1 year, referral to an ophthalmologist for probing can be pursued.
The external eye structures; the size, eyelid, sclera, conjunctiva, pupil, and iris of each eye; and the distance between the eyes are inspected (AAP, 1996a). Abnormalities in any of these may be associated with various syndromes. For all infants, the red reflex should be elicited with an ophthalmoscope to observe for symmetry, any opacities, and white or dark spots in the red circle, which may indicate congenital cataracts or retinoblastoma. Congenital glaucoma should be ruled out by checking the cornea’s diameter (<1 cm is normal). Eye color does not stabilize until age 6 years, and in about 10% of individuals it continues to change into adulthood (Bito et al., 1997). For more information, see Chapter 52.
Strabismus is the inability to focus both eyes on an object simultaneously. This normally may be seen intermittently up to 6 months of age as the infant develops extraocular muscle control. It can be detected by an asymmetric light reflex test or with the cover test, in which the examiner detects the child’s dominant eye by watching the movement of the infant’s eyes while they focus on a near object. The nondominant eye will move to focus if the dominant eye is covered. Amblyopia (reduced visual acuity) occurs in the nondominant eye as a result of suppressing its image to avoid diplopia.
Any hint of constant or persistent intermittent squint in a child older than 6 months warrants referral to an ophthalmologist. Failure to detect and treat strabismus and its resultant amblyopia within the first few years of life can lead to permanent visual loss.
Ear, Nose, and Throat
The ear, nose, and throat area is a frequent site of congenital malformations and should be examined thoroughly. Fetal insults during the first trimester (when the inner ear is developing) may result in impaired hearing. Prematurity also increases the risk for hearing impairment. Children who experienced these conditions require close follow-up and
testing. The Joint Committee on Infant Hearing has recommended universal screening for hearing loss in the newborn period. Hearing can be assessed, though not completely accurately, by observing the infant’s response to the environment. Signs of normal hearing may include display of the startle reflex to a loud noise, changes in the respiratory pattern to sound, and turning toward and localizing sound.
testing. The Joint Committee on Infant Hearing has recommended universal screening for hearing loss in the newborn period. Hearing can be assessed, though not completely accurately, by observing the infant’s response to the environment. Signs of normal hearing may include display of the startle reflex to a loud noise, changes in the respiratory pattern to sound, and turning toward and localizing sound.
• Clinical Pearl
Parental perception of their child’s hearing usually is correct. Concerns from a parent should prompt investigation.
The external ear should be examined for shape, presence of landmarks, and position. Abnormalities of the external ear often are associated with renal disorders. The external canal is short with a downward curve, so examination may require traction of the pinna down to straighten the canal to view the tympanic membrane.
• Clinical Pearl
Assessing the tympanic membrane of an infant younger than 3 months is fraught with difficulty and at best a challenge for even the most experienced provider.
The eustachian tube has three functions: equilibration of pressures in the middle ear, protection from nasopharyngeal secretions, and provision of a route for drainage of middle ear secretions into the nasopharynx. Dysfunction of the eustachian tube’s ability to equalize pressure results in a greater negative middle ear pressure than normal. When the eustachian tube then opens, nasopharyngeal secretions may be aspirated into the middle ear. Obstruction of the eustachian tube also can result in impaired drainage of middle ear secretions, creating an environment conducive to infection. In children, the eustachian tube is wide and short with a more horizontal lie and poorer equilibration function than found in adults, placing the child at increased risk for otitis media. As the child grows, the eustachian tube lengthens, reducing the predilection to otitis media.
Infants are obligate nose breathers. Patent nares, therefore, are essential. They can be assessed after delivery by alternating compression of the nares and observing the respiratory pattern or by passing a small catheter into each nare to the posterior nasal opening to detect choanal atresia. Maxillary and ethmoid sinuses are very small at birth. The frontal sinus does not develop until early childhood, and the sphenoid sinus does not fully develop until puberty. The lips should be complete without a cleft. Sucking calluses on the upper lips or circumoral cyanosis may be present at birth but should not persist. The buccal mucosa should be pink, and white patches should be scraped with a tongue blade to see if they are adherent, indicating thrush (candidiasis), or nonadherent, indicating milk deposits. The infant may be exposed to Candida in the birth canal, but infection often does not show up as thrush until the second week of life. Thrush often is associated with candidal diaper rash, because the gastrointestinal (GI) system may serve as a reservoir. Treatment consists of nystatin suspension for 7 to 10 days or crystallized lactobacillus solution by mouth. All pacifiers, bottle nipples, and teething rings should be boiled daily to prevent reinfection. Breastfeeding moms may develop candidal infection on their nipples from the infant. Mothers with Candida should apply mycostatin suspension to the nipple after nursing. Thrush is not an indication to discontinue breastfeeding.
Salivation increases at a greater rate than swallowing control, so an infant commonly drools between 2 and 6 months. Infants have 20 deciduous teeth that begin to calcify by 3 months of age but do not erupt until they are calcified enough to withstand chewing (generally between 6 and 24 months). Newborns may have natal teeth, which pose a choking threat if loose and should generally be removed. Epstein pearls may be seen on the gum line; these pearl-like retention cysts will disappear in 1 to 2 months. The tongue should be examined for size, such as in macroglossia, which may be associated with congenital hypothyroidism or other anomalies. Ankyloglossia (tongue-tied) also may be seen, but feeding or speech problems are not expected if the tongue is able to protrude beyond the alveolar ridge. Frenulectomy rarely is indicated. Both the hard and soft palates should be examined for clefts and shape. Cleft of the palate may occur with or without cleft of the lip. High arching and narrow palates are associated with congenital anomalies
and affect tongue placement, leading to feeding and speech problems.
and affect tongue placement, leading to feeding and speech problems.
• Clinical Pearl
The palates should be palpated with the examiner’s fingerpad, and the strength of the infant’s suck can be assessed at this time. A strong coordinated suck should be expected. A weak suck may be associated with congenital anomaly, illness, or sedation. A gag reflex should be elicited as well.
Chest and Lungs
The change in the newborn’s lungs from collapsed alveoli prenatally to functional air exchange sacs postnatally is rapid. Blood flow through the lungs increases as the blood is rerouted from the placenta with clamping of the umbilical cord. The increased blood flow causes the pulmonary arteries to expand and relax, creating a decrease in resistance of the pulmonary circulation compared with the systemic circulation, which causes closure of the foramen ovale within minutes. The increased oxygen in the pulmonary arterial blood stimulates contraction and closure of the ductus arteriosus within 24 to 48 hours. These changes complete the transformation from fetal to extrauterine circulation.
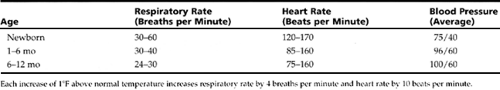
The respiratory rate should be counted for a full minute to get an accurate count, because the rate may vary appreciably each moment. Infants use their diaphragms predominantly, so the abdomen is synchronous with chest movements during respiration. Age-appropriate rates are found in Table 8-7. The rate depends on numerous factors, including room temperature, fever, feeding, and sleep. The newborn rate may be depressed because of the transfer of drugs given to the mother during labor or more rapid than usual if the baby was delivered by cesarean section. Periodic breathing, vigorous respiratory effort followed by apnea lasting 10 to 15 seconds, diminishes as the fetus matures and resolves within a few hours after birth in the term infant. Apnea periods lasting longer than 20 seconds are seen in premature infants and some term infants, which may put them at risk for sudden infant death syndrome (SIDS). Respiratory distress is detected by stridor (inspiratory high pitch as a result of proximal respiratory obstruction), grunting (positive and expiratory pressure [PEEP] to keep alveoli open), accessory muscle use (intercostals or sternoclavicular), or nasal flaring.
The chest wall should be inspected for size and shape, including nipple placement and number. Supernumerary nipples are seen 11 times more commonly in African Americans than in Caucasians; they are more often associated with congenital abnormalities in Caucasians if present. Infants of both sexes may have enlarged breast buds, usually 1 to 3 cm, as a result of transferred maternal estrogen during pregnancy. The breasts also may express a small amount of clear or milky white fluid. Both conditions usually resolve by 2 to 4 weeks, rarely extending beyond age 3 months. No treatment is required. Palpation of the chest should focus on identifying birth trauma, such as crepitus, tenderness, or swelling around a fractured clavicle, which occurs in 1% to 3% of vaginal deliveries. Greenstick type fractures are the most common in infants. The thick periostium around the clavicle prevents severe displacement and angulation, so complications such as pneumothorax are highly unusual.
• Clinical Pearl
Most fractured clavicles will be asymptomatic with minimal physical examination findings. They heal very well within 2 to 3 weeks and generally require no specific treatment. Percussion of the chest is unreliable as the infant’s thorax is too small to isolate changes in pitch.
Expansion of the chest should be symmetrical unless a diaphragmatic hernia or pneumothorax compromises one lung. Auscultation is sometimes difficult, because the small size of an infant’s chest results in hyper-resonance and transmission of sounds from one area to another. Any asymmetry of sound should prompt investigation.
• Clinical Pearl
Sneezing is frequent and not always indicative of a problem or infection.
Transient coughing can occur when drinking a new consistency or feeding too rapidly. This problem should resolve as the infant becomes accustomed to a new feeding pattern. Persistent coughing is always significant and should signal an investigation of respiratory disease or gastroesophageal reflux.
Tracheomalacia, lack of rigidity of the trachea, may present as “noisy breathing” or wheezing in infancy. This condition generally is benign and resolves as the child gets older. Fixed lesions, such as vascular rings, tracheal stenosis, or foreign body, should be ruled out in cases of recurrent or persistent stridor.
Heart
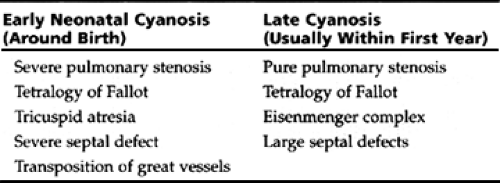
The circulatory system in children is very dependent on respiratory function. Most alterations are responses to respiratory changes as can be seen at birth (described previously). The right and left ventricles are equal in size at birth. The left ventricle grows as its work increases postnatally, finally reaching the adult ratio, compared with the right ventricle, of 2:1. Cardiac abnormalities may cause subtle findings in young infants, such as tiring easily or increased breathing effort during feeding, perioral or prolonged cyanosis during feeding or crying, hepatomegaly from congestion, or lack of expected weight gain. Thus, examination of heart function involves the skin, lungs, and liver in addition to cardiac auscultation as described elsewhere in this chapter. Cyanosis distinguishes the two types of congenital heart disease, and the timing of its appearance helps to distinguish between the types of cyanotic heart disease, as seen in Table 8-8.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree