CHAPTER 3
Health Promotion and Disease Prevention
Robert V. DiGregorio, PharmD, BCACP • Lucille R. Ferrara, EdD, RN, MBA, FNP-BC, FNAP
Health promotion and disease prevention have often been overshadowed by the efforts of the practitioner to restore health and manage disease states. Primary care providers recognize that the old adage “an ounce of prevention is worth a pound of cure” is not only a truism, but imparts significant health, as well as financial, benefits. For example, smoking cessation programs, which may prevent a variety of diseases, could eliminate many of the more than 400,000 deaths and reduce the associated health care costs of more than $65 billion per year in the United States. However, health promotion is often confused with traditional preventive medicine, which has focused on disease prevention and has not fully integrated the concept of overall wellness. While health promotion is about disease prevention, it goes much further. This chapter discusses health promotion from the perspective of patient-centered care, including screening for early indicators of disease and advocating for overall wellness.
 HEALTH PROMOTION IN PATIENT-CENTERED CARE
HEALTH PROMOTION IN PATIENT-CENTERED CARE
The expanded definition of health promotion includes areas of wellness such as injury prevention, healthy eating, and stress reduction, to name a few. The concept of overall wellness and health promotion can be easily coupled to the concept of patient-centered care when viewed as a process of empowerment. Health promotion is a process that enables individuals to improve their quality of life through a partnership with their families/preferred support networks (PSNs; see Chapter 2 for definition and discussion of PSN) and health care providers who assist the individuals in making informed decisions about their health. Once the informed decisions are made by the individual patient and his or her family/PSN, the health care provider moves into a position that provides support for and encourages participation in the individual’s plan for healthy living. This chapter descirbes various aspects of health promotion that could be considered in health promotion or wellness plans that providers develop with their patients.
The concept of patient-centered health promotion is echoed in the current national health and wellness initiative, Healthy People 2020 (HP2020; U.S. Department of Health and Human Services [DHHS], 2014) and the Guide to Clinical Preventive Services (U.S. Preventive Services Task Force [USPSTF], 2012; http://www.ahrq.gov/professionals/cliniciansproviders/guidelines-recommendations/guide/guideclinicalpreventiveservices.pdf). The central purpose of HP2020 is to increase the proportion of Americans who live long and healthy lives by maintaining a full range of functional capacity throughout their lives. The lifestyle promoted in this initiative enables an individual to enter into satisfying relationships with others, pursue career goals, and enjoy recreational activities. The impetus to accomplish these goals and modify behaviors comes from the increasingly health-conscious, responsible public in partnership with their health care providers. Other goals of HP2020 include reducing health disparities among Americans and achieving access to preventive services for all Americans. The Guide to Clinical Preventive Services reflects patient-centered care. It provides detailed guidelines for health care providers in their role as counselors, health facilitators, and patient educators. Many patients have access to an abundance of information both on the Internet and with written material pertaining to their health and are aware of the risks involved with certain behaviors. Despite their knowledge, they continue to partake in a variety of risky behaviors. Information and knowledge are important for promoting a healthy lifestyle: Patients need to motivate themselves and rely more on an overall strategy for changing less-than-optimal health behaviors. Strategies for changing health behaviors can be incorporated into routine health visits, and are outlined in Table 3.1.
Implementing patient counseling in the practice setting raises important issues for providers. Issues regarding the value of screening and the appropriate time to screen patients are discussed later in this chapter and in the individual chapters in Units II through XIII. Other issues may arise as barriers to implementing counseling interventions, such as insufficient reimbursement, patient volume requirements, provider uncertainty about how to counsel effectively, varying interest on the part of patient or staff, and lack of an organizational system of support to facilitate the delivery of patient education (USPSTF, 2014). Many of these issues are addressed by the government publication Guide to Clinical and Preventive Services (USPSTF, 2014). The strategies provided in this chapter can serve as tools to assist the provider in developing an ongoing dialogue to increase patient engagement and to encourage patients at every visit to adapt realistic and achievable personal health practices. Finally, providers should continue to work with patients to develop strategies for sustainability once change occurs.
Strategies Useful in Changing Health Behaviors |
STRATEGY | METHOD |
1. Listen | The provider should elicit the patient’s health care beliefs and concerns and incorporate them into the wellness plan. Cultural sensitivity is also extremely important. |
2. Explain | Fully inform patients of the purposes, benefits, and time frame to reach the goals of the particular intervention. |
3. Encourage reasonable self-management goals | Start slow; small changes are easier to accomplish than large ones. |
4. Be thorough | Be specific and thorough when instructing patients on how to carry out their self-management goals. Patients are less likely to participate in their regimen if they are uncertain of what to do once they leave the provider’s office or clinic. |
5. Establish new behaviors | It is easier to add new positive behaviors than to eliminate established behaviors. |
6. Link behaviors | Combine old and new behaviors so that the patient simply adds another step into an already established practice or routine rather than creating a whole new practice. |
7. Be definitive | Be encouraging and supportive while conveying honest, definitive messages to the patient. |
8. Use an open-ended approach | Patients should be encouraged to describe how they will incorporate their behavior modification into their daily routine. Meanwhile, the provider should be on the lookout for barriers to success for the patient. |
9. Mix resources | In addition to verbal communication, use written materials and integrate support groups, counseling, audiovisual aids, etc. |
10. Involve office staff | Staff members and the overall office environment should communicate consistent positive health care messages. |
11. Refer | If a provider is too busy to work with the patient, the patient should be referred. Patient education and counseling can be provided by many different health care providers, as well as community agencies, voluntary health organizations, instructional materials, and other patients. |
12. Follow-up | Provider-initiated contact is more effective than patient-initiated contact. |
 EVIDENCE-BASED HEALTH SCREENING
EVIDENCE-BASED HEALTH SCREENING
Effectiveness should be the most basic requirement for providing any health care service. This includes health-promotion activities, where the health care provider has the ethical responsibility to “do no harm” to patients. Effectiveness is usually determined from compilations of data or evidence from large randomized clinical trials. The ability to track down, critically appraise, and incorporate this evidence into clinical practice has been referred to as “evidence-based practice.” Evidence of effectiveness alone, however, is not a sufficient reason to perform a particular screening. Factors other than effectiveness, reflecting the trade-offs and broad implications of screening, are relevant to the goals of health promotion.
When deciding on a particular screening instrument, providers must decide to what degree the information from the screening procedure is accurate and reliable. The provider and patient must also determine how the data gained from the screening process will ultimately be applied to patient care. For example, obtaining mammographies in younger women has been the subject of great controversy (Mistry, Barnes, & Ooi, 2013). Mammographic screening, yielding false-positive findings, has caused many women to undergo breast biopsies that uncovered normal tissue. In retrospect, these biopsies were not only unnecessary, but also subjected the women to a painful, invasive procedure and the accompanying anxiety of a possible breast cancer diagnosis. If a younger woman understood this possibility prior to requesting or submitting to a mammogram, she might opt to wait. Even conducting monthly breast self-examination has come under scrutiny for a low predictive yield and is no longer a population-based screening recommendation (USPSTF, 2009). Considerable controversy also exists with regard to screening asymptomatic patients for colorectal cancer (Garcia, Quintero, Nicolas Perez, Hernandez, & Jimenezsosa, 2011) and prostate cancer (Culati, Gore, & Etzioni, 2013).
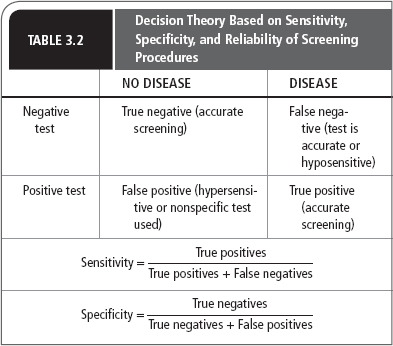
Misinterpretation of screening tests, based on false-positive and false-negative findings, may lead to over- or undertreating patients. While false-positive results may cause undue anxiety and diagnostic workup for a patient, a false-negative finding can give a patient a false sense of security as well as delay treatment. Providers must understand the sensitivity, specificity, and reliability underlying disease prevalence and relative cost of screening before incorporating a screening process into a patient’s wellness plan.
Sensitivity
The ability of a particular test to detect an abnormal condition is referred to as the sensitivity of the test. A test that detects minute variations from the normal condition would be described as a highly sensitive test. Even highly sensitive tests, however, do not always confirm specific disease states. For example, current technology allows for the measurement of gamma glutamyltransferase (GGT) levels within 1 unit/L; thus, a GGT level of 1 unit above normal could be detected. However, this elevated level does not differentiate among alcoholism, hepatitis, smoking, lupus, or a biliary obstruction. In fact, it may not indicate any abnormal condition. In constrast, the smell of a patient’s clothing may reveal the unmistakable odor of cigarette smoke. Of course, this rudimentary test would not reveal how much the person smokes or even if the smell was from the individual or second hand.
Specificity
Specificity refers to the ability of a test or screening procedure to identify the exact problem or condition. In the preceding example, GGT was a highly sensitive but nonspecific screening test. Examples of highly specific screening tests include blood pressure measurement for hypertension, ejection fraction for cardiac function, prostate-specific antigen for prostate cancer, and blood cultures for infectious pathogens. It is important to consider that a positive finding in a highly specific test does not necessarily confirm a disease. The possibility of second-hand smoke in the preceding example illustrates this scenario. Another example of specificity without diagnostic merit would be the use of a blood level to determine drug toxicity. While an elevated level may certainly be specific to the drug product in question, not every patient with an elevated level will exhibit toxic effects. A summary of specificity and sensitivity measures is shown in Table 3.2.
Reliability
Tests used in screening procedures may be highly sensitive and specific, yet remain unreliable. Reliability takes into account the accuracy and precision of the test. Test results may indicate a specific finding marginally above the norm, but because of technical error, expired reagents, or faulty test techniques, it may be inaccurate. Variability in the performance of the test procedure or examination can lead to unreliable results by compromising precision or reproducibility. Blood pressure readings taken incorrectly (e.g., the arm is not at heart level), by inexperienced individuals, or the use of electronic blood pressure measuring devices may increase the amount of blood pressure screening and monitoring data available to providers; however, these data may be imprecise, inaccurate, and therefore unsuitable for making health care decisions.
Cost Factors
In an ideal world of unlimited resources, patients would have infinite access to their health care providers, health technology, and health care products. However, resources are increasingly limited, and screening for conditions, simply because the technology exists, is not appropriate. Even screening that is relatively free may lengthen a health care visit and prevent another patient from obtaining care that day. Extremely specific, sensitive, and reliable testing may be available but not utilized due to disproportionally high costs as compared to an older, less expensive test. Screening for cervical cancer with newer test methods rather than Pap smears is a good example of this phenomenon. For each screening test, the cost of evaluating all susceptible individuals must be weighed against the prevalence of the condition and the cost of treating the condition. In some cases, the relatively low prevalence and low cost of treating a disease may make implementing such a screening program unrealistic. Likewise, therapy leading to an individual’s complete cure of a disease may cost less than screening or immunizing an entire population.
Number Needed to Treat or Harm
The number needed to treat (NNT) or harm (NNH) is an epidemiological calculation that is used to determine the effect of a treatment. It is the number of patients who must be treated in order to see a treatment benefit or adverse effect. It may also be applied to such public health measures as vaccinations, as in the number of individuals who must be vaccinated in order to prevent one hospitalization, or one death. Using NNT also provides a sense of the economic impact of a treatment. For example, if the cost to treat is high and the NNT is also very high, it would not be cost effective to treat with that modality. If the cost is low and the NNT is also low, great benefit may be derived at little cost and thus the modality would be very cost effective. The NNT is conceptually the inverse of absolute risk reduction (ARR) or incidence. Providers should evaluate treatment options, as well as the utility of screening techniques, with this in mind. NNT is often not disclosed directly in the medical literature, but can be easily calculated. To calculate NNT, one must determine the ARR in a clinical trial (event rate in the control group minus the event rate in the treatment group); the NNT is then 1/ARR. In general, NNTs will be smaller if the disease is more prevalent. Highly effective treatments usually have NNTs of less than 10. NNTs are also time dependent, meaning that if the data from a clinical trial were obtained over multiple years, the NNT for the same derived benefit in 1 year must be multiplied by the number of years in the trial. There are limitations to using NNT in practice. These limitations include the potential for bias and lack of reliable confidence intervals, as well as difficulties in ruling out the possibility of no difference between two treatments or groups (Hutton, 2010).
 SCREENING
SCREENING
As a form of health promotion and disease prevention, screening can be as simple as questioning a patient about the common warning signs or symptoms of a disease state, or as complex as subjecting the patient to invasive examinations or testing procedures. The most common areas of health screening include the prevention and early identification of coronary artery disease and a variety of cancers. The warning signs and symptoms and current approaches to this type of screening are covered in detail in the individual chapters of Units II through XIII. Screening for high-risk behaviors, injury prevention, and complementary approaches to wellness are discussed in this chapter.
Medication Misuse and Medication Reconciliation
Inappropriate usage of medications can be described as the nation’s “other drug problem.” The misuse of prescription and over-the-counter medications contributes to an increase in morbidity, mortality, and health care costs (Centers for Disease Control and Prevention [CDC], 2012a). Variations of the term compliance have often been used to describe the appropriate use of a medication by a patient. Patients are often labeled as noncompliant or over compliant for choosing to use medications in a manner other than that recommended by their health care providers or product labeling. While this concept is one of tremendous importance, the term compliance does not foster a patient-centered approach to health care. Because use of the word compliance imparts a message of paternalistic health care, use of the term has been avoided in this text; instead, the authors and contributors have opted to describe how patients may optimally participate in their health care by using medications rationally.
The assumption in patient-centered care is that patients are involved in making the choices for their therapy and are involved in a partnership with their provider for successful therapy. Providers must acknowledge and accept that patients are affected by the act of prescribing in a variety of ways. Often overlooked are the reasons for misuse of medications, including adverse effects of a selected regimen, cost of the regimen, inconvenience of multiple daily dosing, a lack of well-defined symptoms, and the psychological components of taking medications and being “sick.” Patients may be reluctant to discuss their choice to underuse or discontinue their medications because of the possible embarrassment of revealing side effects (e.g., impotence with antihypertensives), unwillingness to disclose financial problems, or for fear of disappointing their provider. Overuse of medications may be related to less-than-expected efficacy or refractory disease (e.g., overuse of ergotamine or sumatriptan for migraine headaches). Rather than discussing these issues with their health care providers, many patients have resorted to alternative therapies or discontinued therapy altogether. To encourage rational and appropriate medication use and participation in therapeutic care plans, providers should provide patients with information regarding the available treatment options (pharmacotherapeutic, surgical, and complementary) for their condition, as well as specific information on the therapy chosen.
The need for reconciling medications with a patient cannot be overemphasized. In an environment where patients seek care from multiple providers and specialists; are admitted to hospitals where medication changes are made for a variety of reasons, including new health issues, lack of efficacy, adverse effects of previous medications, therapeutic interchanges for cost savings, use of generic equivalents, dosing changes, and insurance requirements; and where multiple pharmacies (including mail order) are used, there is a tendency for patients to be confused about their medications. Such confusion often leads to patients taking duplicate medications, taking additive doses of medications, or omitting needed medications. These discrepancies typically occur at three transitions-of-care points: hospital admission to discharge; hospital discharge to other care facilities; and discharge from a health care facility to home. Intentional changes in medication therapy occur in virtually all patients. Unintentional discrepancies in medication management may occur in as many as 86% of patients. Cardiovascular medications represent the greatest number of discrepancies (Sinvani et al., 2013). To avoid such misadventures, reviewing and reconciling the complete medication regimen at each transition point is important. Most importantly, primary care providers should make a point to conduct a thorough reconciliation of medications within the first week of a patient’s discharge from an inpatient setting. Data are still forthcoming, but a 2012 systematic review of 26 inpatient medication reconciliation studies supported the benefit of pharmacist-led medication reconciliation processes (Kwan, Lo, Sampson, & Shojania, 2013).
Counseling and follow-up are appropriate for all members of the health care team; however, if a patient has concerns that cannot be addressed in the time frame of an office visit, or if the quest for information is beyond the scope of the provider’s expertise, the patient should be referred to additional resources for the information. Primary care providers should seek such an interdisciplinary approach to medication management and reconciliation.
 GROWTH AND AGING IN HEALTH PROMOTION
GROWTH AND AGING IN HEALTH PROMOTION
Primary care providers must use their time wisely to provide counseling on high-risk behaviors. It may be inappropriate to counsel certain age groups on certain behaviors. If morbidity and mortality data are considered, a provider might decide that counseling a 70-year-old female in a 45-year marriage on birth control and sexually transmitted diseases might not be prudent. Likewise, counseling the 20-year-old college student of the dangers of falls and polypharmacy may be equally pointless.
Developing health-promotion and disease-prevention plans with patients requires consideration of growth, development, and maturation across the adult lifespan. Milestones of the young adult, middle adult, and older adult stages help to provide a framework for health-promotion and disease-prevention activities.
Young Adult
The young adult stage spans the ages of 18 to 35 years. The physical and emotional changes that occur during this time, and the style of learning, through experimentation and experience, focus on health-promotion and disease-prevention activities. Generally, by the age of 20 years, physical growth is complete. This period is often described as the healthiest time of life. Maintaining proper functioning is a goal for this period of time that will affect the person not only as a young adult, but throughout adult life. Toward this end, health-promotion and disease-prevention activities should be focused on developing healthy lifestyle behaviors; early detection of health problems; and prevention of accidents, injuries, and the morbidity and mortality associated with violence.
Middle Adult
Middle adulthood spans the ages of 35 to 65 years. This period of time is marked by biological changes. It may also be a time of turmoil, reassessment, and change. Leading causes of death during this time are heart disease, lung cancer, cerebrovascular disease, breast cancer, colorectal cancer, and obstructive lung disease. Genetics, as well as other factors that health-promotion and disease-prevention activities can be directed toward, such as nutrition and exercise, contribute to these conditions.
Older Adult
By the year 2050, it is projected that 20.2% of the population will be older than 65 years. Within the older adult age group is the fastest growing segment of the population, those older than 85 years. It is expected that by the year 2050, this group will account for 7.4% of the U.S. population (U.S. Senate Special Committee on Aging, 2009). Age-related changes are inevitable but occur with variability. Chronic illness and functional disabilities are interrelated and increase with age. While the all-cause mortality rate for older Americans has decreased by 19.7% due to drops in heart disease and stroke, lower respiratory disease and diabetes rates have increased. The leading causes of death in this age group are heart disease, cancer, stroke, chronic lower respiratory disease, pneumonia, influenza, and diabetes. However, the mortality rate associated with Alzheimer’s disease has increased 40-fold. Influenza and pneumonia remain in the “top five” causes of death for older Americans (U.S. Senate Special Committee on Aging, 2007). Alcohol and drug abuse, homelessness, and physical abuse are also concerns in the older adult population that must be considered in health-promotion and disease-prevention activities.
Accidents are a common problem of the elderly. With physiological aging comes decreased sensory acuity, reaction time, muscle strength, and impaired balance. As a result, in those older than 65 years, one third will report a fall each year, making falls the greatest cause of accidents in this age group (CDC, 2008).
Risk factors for falls include personal and environmental factors. Personal risk factors include age, functional abilities, and chronic conditions. Environmental factors include tripping hazards, lack of stair railings or grab bars, slippery surfaces, unstable furniture, and poor lighting. Additionally, the use of psychoactive medications (benzodiazepines, antidepressants, sedative/hypnotics), and polypharmacy place the elderly at a high risk of falls. Providers should evaluate the fall potential of patients and develop strategies for fall prevention, which may include minimizing environmental risks, teaching or reteaching adaptive behavior, and reducing accompanying risk factors such as changes in visual acuity (2005 NCOA Falls Free: Promoting a National Falls Prevention Action Plan).
 NUTRITIONAL SCREENING AND ASSESSMENT
NUTRITIONAL SCREENING AND ASSESSMENT
Nutrition is commonly discussed between patient and provider in order to assist patients in establishing healthy nutritional goals and habits. The increase in the incidence of obesity in childhood and adolescents, the prevalence of type 2 diabetes in minorities, a rise in food insecurity among low-income and homeless people, malnutrition in older adult and mental health patients, and addressing the nutritional needs of special populations (e.g., pregnancy and immunocompromised patients) are a few of the challenges that providers confront during patient encounters (Amaral, Antunes, Cabral, Alves, & Kent-Smith, 2008; Champagne & Wroten, 2012; Khan, Pinckney, Keeney, Frankowski, & Carney, 2011; Neelemaat, Meijers, Kruizenga, van Ballegooijen, & van Bokhorstde van der Schueren, 2011; Rist, Miles, & Karimi, 2012; Söderhamn, Flateland, Jessen, & Söderhamn, 2011). In addition, nutritional guidance and counseling is an important preventive and health maintenance measure for healthy patients as well. For these and other reasons, nutritional screening and assessment of all patients is key.
A number of assessment and screening tools exist and can be used to assist the provider with nutritional assessment. Basic screening such as the tracking and trending of weight, body mass index (BMI), and growth and development is invaluable when establishing a baseline assessment of nutritional status. Further assessment, however, may be required when health risks are identified or diseases of chronicity exist. Other screening and assessment tools, such as The Nutritional Form for the Elderly, Mini-Nutritional Assessment short-form (MNA-SF), the Malnutrition Screening Tool (MST), the Malnutrition Universal Screening Tool (MUST), the Short Nutritional Assessment Questionnaire (SNAQ; www.ncbi.nlm.nih.gov), the Nutritional Risk Screening 2002 (NRS-2002), and the Screening Tool for the Assessment of Malnutrition in Pediatric Patients (STAMP, www.stampscreening.org) are standardized assessment questionnaires and tools that can be incorporated into one’s practice or adapted into the electronic health record (EHR).
The United States Department of Agriculture (http://fnic.nal.usda.gov/dietary-guidance), state and local departments of health (www.health.ny.gov), and other disease-specific websites (e.g., American Cancer Society, American Diabetes Association) provide nutrition information and screening tools that can be used for nutritional assessment for all patient populations.
In addition to the screening and assessment tools, the provider can also access a full list of guidelines and recommendations for healthy patients and vulnerable populations such as older adults, pediatrics, patients with chronic disease, and oncologic illnesses. The DHHS’s, Agency for Health Care Research and Quality (AHRQ) (www.ahrq.gov/professionals/clinicians-providers/guidelines-recommendations/index.html) is a U.S. government agency that is committed to the “improvement of patient care quality, safety, efficiency, and effectiveness” (www.ahrq.gov). The information found on this website is geared to both providers and patients. This site has excellent patient education tools that can be downloaded and printed for patients, and the site is also “patient friendly” so that patients can be directed to the site if they have Internet access.
 ADULT IMMUNIZATIONS
ADULT IMMUNIZATIONS
Vaccines are recommended for adults on the basis of age, vaccination history, health conditions, lifestyle, occupation, and travel. Health providers tend to place a high level of importance on pediatric immunizations, but neglect to maintain a healthy immunization status in adults. In particular, adults are in need of tetanus, diphtheria, and acellular pertussis (Tdap) vaccine, influenza vaccine (annually), and pneumococcal vaccine. Certain populations may also benefit from measles, mumps, rubella (MMR), human papillomavirus vaccine (HPV), zoster vaccine, and hepatitis A and hepatitis B vaccines. Guidelines for the administration of vaccines, as well as the immunization schedules, are updated annually by the CDC’s Advisory Committee on Immunization Practices (ACIP) and published in Morbidity and Mortality Weekly Reports (MMWR) and on the Vaccines and Immunizations Internet website (www.cdc.gov/vaccines/schedules/hcp/adult.html). Adults older than 50 years should be offered a one-time immunization against herpes zoster to prevent the reactivation of the virus (“shingles”). Adults older than 65 years should be offered pneumococcal vaccine every 5 years to protect against pneumonia. Influenza vaccine should be offered annually to all adults.
Health Care Decisions
When patients are in good health, matters related to their ability to make health care decisions are generally not of concern. It is, however, important for primary care providers to discuss with patients their right to direct the kind of health care they would or would not want, in the event that they are unable to do so.
Advance directives are broadly defined to include living wills and appointment of a health care agent. A living will is a document created by an individual to authorize in advance withholding or withdrawing artificial life-support measures in the case of terminal or debilitating illness, injury, or irreversible coma; it is signed, dated, and witnessed. Appointing a health care agent differs from state to state and may be referred to as: Durable Power of Attorney for Health Care; Health Care Power of Attorney; Appointment of a Health Care Agent; or health care proxy. Regardless of state mandates, the objective of appointing a health care agent is the same: allowing an individual to appoint someone he or she trusts to control his or her health care through the individual’s written instructions.
Competent adults have the right to create an advance directive regarding treatment decisions, including life-sustaining measures. There are state-mandated forms for advance directives that the patient completes. Patients have the right to change their health care agent, and/or change their written instructions, or cancel their advance directive, at will. If the patient has both a living will and an appointed health care agent, usually the appointment of the health care agent takes precedence.
Discussing advance directives with patients is an important part of proactive primary care. Encouraging patients to appoint a health care proxy and knowing whom the patient has appointed are essential to respecting a patient’s wishes should he or she be unable to make his or her own health care decisions.
 IDENTIFYING AND MODIFYING HIGH-RISK BEHAVIORS
IDENTIFYING AND MODIFYING HIGH-RISK BEHAVIORS
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree