2 Head Disorders of the mandibular joints and ears, as well as pain referred from the base of the lung, heart, and pericardium Headache due to hypertension and hypotension as well as pain referred from disorders of the pylorus and the intestines Ask patients about grinding teeth at night, blockage, and/or galvanic pain when chewing (if applicable, orthodontic bite guard). ! +++ R2–3 times a week MM, PIR, Orthodont !++ R 2 times a week, up to 3 weeks ThE, MM, Acu, TENS, Chiro, Orthotech ! ++(+) R 2 times a week, up to 4 weeks
 Complex Pain
Complex Pain
Temporal/Parietal Headache
Indications
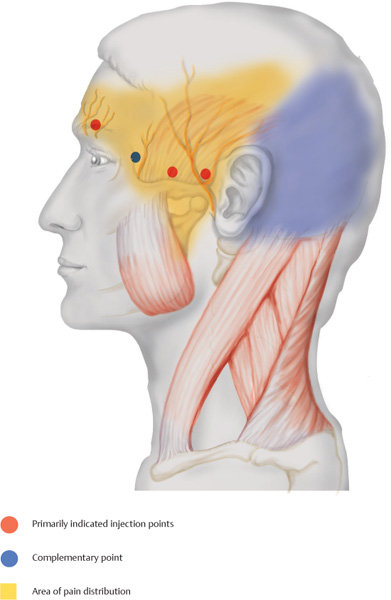
 Temporal headache (yellow corresponds to the area of radiation)
Temporal headache (yellow corresponds to the area of radiation)
 Parietal headache (yellow and blue corresponds to the area of radiation)
Parietal headache (yellow and blue corresponds to the area of radiation)
Differential Diagnoses
 Temporal (yellow pain area)
Temporal (yellow pain area)
 Parietal (yellow and blue pain area)
Parietal (yellow and blue pain area)
Material
 Local anesthetic: 2–3mL
Local anesthetic: 2–3mL
 Needle: 0.4 × 20 mm
Needle: 0.4 × 20 mm
Technique
 The temporal artery is palpated and shielded with the palpating finger. The needle is inserted in front of and behind the artery into the temporalis muscle.
The temporal artery is palpated and shielded with the palpating finger. The needle is inserted in front of and behind the artery into the temporalis muscle.
 Supraorbitally, the notch at the center of the bone above the eye is palpated and the needle is inserted cranially at an angle until bone contact is made.
Supraorbitally, the notch at the center of the bone above the eye is palpated and the needle is inserted cranially at an angle until bone contact is made.
Risks
 Injury to the temporal artery, if the artery is not shielded with the palpating finger, and to the supraorbital artery (avoid by attempting aspiration prior to injection).
Injury to the temporal artery, if the artery is not shielded with the palpating finger, and to the supraorbital artery (avoid by attempting aspiration prior to injection).
 If there is a galvanic response across the antero-lateral part of the skull when the anesthetic is being injected into the anterior temporal region, the needle is inserted slightly more ventrally to avoid injury to the temporoparietal nerve.
If there is a galvanic response across the antero-lateral part of the skull when the anesthetic is being injected into the anterior temporal region, the needle is inserted slightly more ventrally to avoid injury to the temporoparietal nerve.
Concomitant Therapies
 Manual mobilization of the temporomandibular joint, if indicated
Manual mobilization of the temporomandibular joint, if indicated
 Complemented by temporalis relaxation and relaxation therapy
Complemented by temporalis relaxation and relaxation therapy
Remarks
Occipitoparietal Headache
Indications
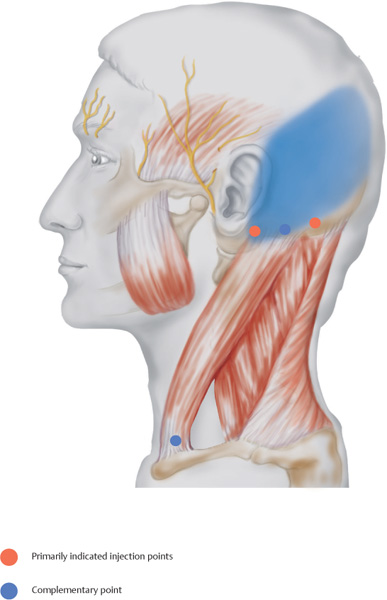
 Occipitoparietal headache (blue corresponds to the pain area)
Occipitoparietal headache (blue corresponds to the pain area)
Differential Diagnoses
 Craniovertebral joints, disorders in the area of the cervical vertebrae, disorders of the nasal and maxillary sinuses and the pharyngeal tonsils
Craniovertebral joints, disorders in the area of the cervical vertebrae, disorders of the nasal and maxillary sinuses and the pharyngeal tonsils
 Referred pain from liver, intestines, ovaries, and testicles
Referred pain from liver, intestines, ovaries, and testicles
Material
 Local anesthetic: 3 mL
Local anesthetic: 3 mL
 Needle: 0.4 × 20 mm
Needle: 0.4 × 20 mm
Technique
 The insertion of the sternocleidomastoid and the palpable protuberance of the mastoid process is located; less than 1 finger width behind the posterior base of the ear the needle is inserted vertically until bone contact is made; the second injection is performed 2 finger widths toward the occiput where the muscles of the neck insert (directly above the hairline).
The insertion of the sternocleidomastoid and the palpable protuberance of the mastoid process is located; less than 1 finger width behind the posterior base of the ear the needle is inserted vertically until bone contact is made; the second injection is performed 2 finger widths toward the occiput where the muscles of the neck insert (directly above the hairline).
 Complementary injection sites are located at and between the caudal insertions of the sterno-cleidomastoid at the end of the clavicle and the superior edge of the sternum.
Complementary injection sites are located at and between the caudal insertions of the sterno-cleidomastoid at the end of the clavicle and the superior edge of the sternum.
Risks
 The occipital insertion point away from the ear is close to the course of the occipital vein and artery. Avoid intra-arterial injection through prior aspiration.
The occipital insertion point away from the ear is close to the course of the occipital vein and artery. Avoid intra-arterial injection through prior aspiration.
 For the injection at the distal insertion of the sternocleidomastoid, the needle is inserted almost 1 cm. To recognize injury to the jugular or transverse cervical vein in time and to prevent excessively deep injection, aspiration is mandatory.
For the injection at the distal insertion of the sternocleidomastoid, the needle is inserted almost 1 cm. To recognize injury to the jugular or transverse cervical vein in time and to prevent excessively deep injection, aspiration is mandatory.
Concomitant Therapies
 Complemented by traction treatments, for example, Glisson traction and manual mobilization techniques
Complemented by traction treatments, for example, Glisson traction and manual mobilization techniques
 Acupressure
Acupressure
 Transcutaneous electrical nerve stimulation therapy
Transcutaneous electrical nerve stimulation therapy
 Chiropractic treatment
Chiropractic treatment
Remarks
 Severe occipitoparietal headache in the morning indicates faulty sleeping position.
Severe occipitoparietal headache in the morning indicates faulty sleeping position.
 Abdominal sleeping position must be avoided. Try special neck cushions, if applicable.
Abdominal sleeping position must be avoided. Try special neck cushions, if applicable.
Parietal Lock
Indications
 Chronic parietal headache
Chronic parietal headache
 Pulsating temporal headache
Pulsating temporal headache
 Pain accompanying ear disorders
Pain accompanying ear disorders
 Tension headache
Tension headache
 Headache triggered by hormones
Headache triggered by hormones
 Posttraumatic headache
Posttraumatic headache
Differential Diagnoses
 Disorders of the mandibular joints, upper and lower jaw, nasal and frontal sinuses, disorders involving the zygomatic arch, inflammatory changes of the scalp
Disorders of the mandibular joints, upper and lower jaw, nasal and frontal sinuses, disorders involving the zygomatic arch, inflammatory changes of the scalp
Material
 Local anesthetic: 4–5mL
Local anesthetic: 4–5mL
 Needle: 0.4 × 20 mm
Needle: 0.4 × 20 mm
Technique
 It is recommended that the parietal lock be implemented from two separate injection sites. The first injection site is located by placing the palpating finger slightly less than 1 cm supra-orbital and carefully moving it toward the upper rim of the ear, where it will slide into a shallow depression. At this site, the needle is inserted toward the anterior upper rim of the ear. At the same time, the other hand tightens the skin toward the forehead. Now the needle is advanced parallel to the skull, almost up to the anterior rim of the ear. The local anesthetic is injected at intervals while the needle is being retracted.
It is recommended that the parietal lock be implemented from two separate injection sites. The first injection site is located by placing the palpating finger slightly less than 1 cm supra-orbital and carefully moving it toward the upper rim of the ear, where it will slide into a shallow depression. At this site, the needle is inserted toward the anterior upper rim of the ear. At the same time, the other hand tightens the skin toward the forehead. Now the needle is advanced parallel to the skull, almost up to the anterior rim of the ear. The local anesthetic is injected at intervals while the needle is being retracted.
 The second injection takes place approximately 3 cm behind the posterior base of the ear. At the upper edge of the lateral occiput, the needle is inserted toward the ear. From there it is advanced until it almost reaches the posterior base of the ear. The local anesthetic is injected at intervals while the needle is being retracted.
The second injection takes place approximately 3 cm behind the posterior base of the ear. At the upper edge of the lateral occiput, the needle is inserted toward the ear. From there it is advanced until it almost reaches the posterior base of the ear. The local anesthetic is injected at intervals while the needle is being retracted.
Risks
 The frontal arch of the superficial temporal artery may be injured in the area of the anterior injection site. Fortunately, the pulsation of the artery is easily palpable. Aspiration prior to injection avoids unintentional intravascular administration.
The frontal arch of the superficial temporal artery may be injured in the area of the anterior injection site. Fortunately, the pulsation of the artery is easily palpable. Aspiration prior to injection avoids unintentional intravascular administration.
 Injury to the auricle must be avoided during injection behind the ear.
Injury to the auricle must be avoided during injection behind the ear.
Concomitant Therapies
 In ear disorders, a quaddle may be placed at the Ear Gate, acupuncture point TB-21.
In ear disorders, a quaddle may be placed at the Ear Gate, acupuncture point TB-21.
 In migraines, an additional injection may be performed at the exit of the supraorbital nerve.
In migraines, an additional injection may be performed at the exit of the supraorbital nerve.
 In tension headaches, autogenic training, biofeedback therapy, muscle relaxation techniques, for example, according to Jacobson, acupressure, and reflexotherapy of the feet are recommended.
In tension headaches, autogenic training, biofeedback therapy, muscle relaxation techniques, for example, according to Jacobson, acupressure, and reflexotherapy of the feet are recommended.
 If applicable, systemic myotonolysis by means of medication.
If applicable, systemic myotonolysis by means of medication.
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Anesthesia Key
Fastest Anesthesia & Intensive Care & Emergency Medicine Insight Engine