Genetics of Cluster Headaches
Michael Bjørn Russell
Richard C. Trembath
Up until 10 years ago little evidence to support a genetic component to the etiology of cluster headache had been identified. More recently, a number of studies have indicated that genetic determinants are likely to be important in the etiology of cluster headache.
Cluster Headache and Migraine
Cluster headache, migraine without aura, and migraine with aura are likely to be distinct headache disorders. Each is characterised by distinct clinical features (12,47). The prevalence of migraine is similar in cluster headache as is seen in the general population (31). Furthermore, brain activation occurs in different areas, namely the ipsilateral hypothalamic gray area in cluster headache and the contralateral side of the brainstem in migraine without aura (19,52).
Gender Ratio
The ratio between men and women is 1.2:1 in familial cluster headache, but 4.4:1 in clinic populations (1,8,10,14, 15,18,28,29,31,49). The ratio in clinic populations has decreased in the last decades, possibly due to increased awareness that women also can suffer from cluster headache (8,18). A recent British study reported the ratio between men and women was 2.5:1 (1). The different gender ratio observed in familial cluster headache from that seen in clinic populations may suggest different etiologies.
Genetic Studies
Twins
The literature reports six concordant and two discordant monozygotic twin pairs and one concordant (unlike sex) and nine discordant (four same and five unlike sex) dizygotic twin pairs (3,7,25,33,37,38,45). The concordant twin pairs were all case reports, except for two twin pairs from clinic populations, while the discordant twin pairs were from a population-based twin study. Interpretation of the twin data should take into account the limited sample size and publication bias (21).
Positive Family History
Probands from 12 clinic population-based studies from 1947 to 1985 reported that 47 first-degree relatives were affected in 1182 families (31). This suggests an increased family risk, even though the diagnosis may not have been confirmed in all families. More recently, an Italian and a Dutch survey with physician-confirmed diagnoses reported familial occurrence in 2.3% (5/222) and 4.1% (70/1720) of the families, respectively (20,51).
Genetic Epidemiologic Surveys
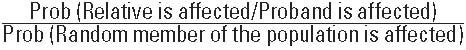
Four genetic epidemiologic surveys provide more complete information about the relatives (10,14,15,28,29). Table 86-1 illustrates the risk to first- and second-degree relatives based upon a population prevalence of cluster headache of 1 per 500 inhabitants. The first-degree relatives had a five- to 18-fold increased risk of cluster headache compared to the general population. Second-degree relatives had a one- to threefold increased risk. Varying observations may, at least in part, be explained by methodologic differences. The French survey acquired a more comprehensive dataset, as all first-degree relatives were directly interviewed by a physician (10). A physician interviewed possibly affected relatives in the Danish survey (28,29). This causes the risk of cluster headache to be a minimum figure, as probands may fail to report about affected relatives. The American survey was based on probands reports only (14). This can cause either under-or overestimation of the risk of cluster headache depending on whether the probands misclassify their relatives more or less than they fail to report about the affected.
The Danish probands reports were inaccurate, as the diagnosis of cluster headache was confirmed in only 57% while the remaining 43% had migraine (29). The Italian survey was based on probands reports, and possibly affected relatives were interviewed by a physician (15). Eleven of the 57 affected relatives had probable cluster headache. This is either an under- or overestimation of the risk of cluster headache, depending on whether the number of those with probable cluster headache is more or less than those affected not reported by the probands. The significantly increased familial risk strongly suggests that cluster headache has a genetic cause. Theoretically, a shared environment can produce relative risks of the magnitude observed for cluster headache only under extreme conditions (13).
The Danish probands reports were inaccurate, as the diagnosis of cluster headache was confirmed in only 57% while the remaining 43% had migraine (29). The Italian survey was based on probands reports, and possibly affected relatives were interviewed by a physician (15). Eleven of the 57 affected relatives had probable cluster headache. This is either an under- or overestimation of the risk of cluster headache, depending on whether the number of those with probable cluster headache is more or less than those affected not reported by the probands. The significantly increased familial risk strongly suggests that cluster headache has a genetic cause. Theoretically, a shared environment can produce relative risks of the magnitude observed for cluster headache only under extreme conditions (13).
TABLE 86-1 Age and Gender Standardized Risk of Cluster Headache and Gender Standardized Risk Only* | |||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree