Gastrointestinal Bleeding: Introduction
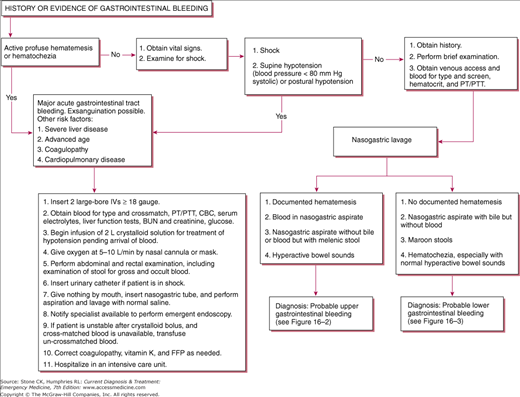
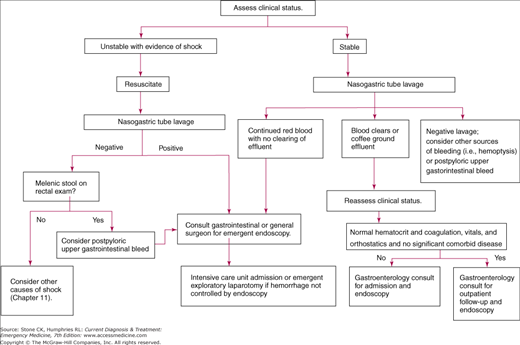
For the majority of patients presenting with gastrointestinal (GI) bleeding, hematemesis, hematochezia, or melena will be the chief complaint. Occasionally, patients may present with only dizziness, weakness, or syncope. If no obvious cause of shock is present, gastric lavage and a rectal examination should be performed promptly as part of the initial assessment. The severity of blood loss must be assessed quickly so that lifesaving therapeutic interventions can be instituted. Factors that increase the morbidity and mortality are hemodynamic instability, ongoing symptoms, inability to clear bleeding with lavage, age over 60, and other comorbidities.
Immediate Management of Life-Threatening Bleeding
Any patient presenting to the emergency department with ongoing hematemesis or hematochezia is at significant risk of exsanguination, and prompt volume resuscitation must begin at once. Proceed with initial stabilization procedures as described below.
Place the patient in a monitored bed and obtain a full set of vital signs including oxygen saturation. If the initial systolic blood pressure is greater than 100, and the pulse is less than 100 beats/min in the supine position, consider obtaining orthostatic blood pressure and pulse rate measurements.
Signs, symptoms, or history that may indicate ongoing hemorrhage are as follows:
- Profuse hematemesis or hematochezia
- Hypotension, tachycardia, or signs of shock
- Postural hypotension, tachycardia, or lightheadedness
- Possible aortoenteric fistula (history of abdominal aortic aneurysm repair or palpable pulsating abdominal mass)
- Known or suspected esophageal varices
- Previous history of GI bleeding
- History of diverticulosis
As with any emergency, always address your patient’s ABCs first.
Consider endotracheal intubation for patients with ongoing massive hematemesis or if signs and symptoms of shock are present, If immediate airway control is not needed, provide supplemental oxygen as needed to maintain oxygen saturation at greater than 93%.
Insert two large-bore intravenous catheters (18 gauge or larger) into peripheral veins. If peripheral access cannot be obtained, consider placement of a central venous line.
Rapidly bolus either warmed lactated Ringer’s or normal saline to restore intravascular volume.
For persistent hypotension despite the infusion of 2 L of crystalloid, consider immediate transfusion of cross-matched blood if available. If not, then transfuse O-negative blood until cross-matched blood is available. There should be a lower threshold to transfuse for elderly patients or those with known cardiac dysfunction. Continue transfusion to maintain systolic blood pressure at greater than 90 mm Hg.
Send blood for complete blood count. Type and cross-match blood for two to six units, depending on the extent of bleeding and the patient’s status. Measure prothrombin and partial thromboplastin time to assess for any coagulopathy. Measure serum electrolytes and renal and liver functions. Blood urea nitrogen is elevated in many patients with upper GI bleeding. Venous blood gas and lactate may be helpful in assessing tissue perfusion status. Whenever possible, draw the patient’s blood for analysis prior to transfusion for accurate coagulation studies.
Obtain an electrocardiogram (ECG) for any patient older than 50 years; for any patient with a history of ischemic heart disease or significant anemia; and for any patient with chest pain, shortness of breath, or severe hypotension. If the initial ECG demonstrates ongoing ischemia in the face of ongoing GI bleeding, then consider immediate transfusion of packed red blood cells. If a patient’s initial hematocrit is less than 30% and he or she has a history of ischemic heart disease, consider early transfusion. Maintain a low threshold of suspicion for myocardial infarction (MI), as patients suffering MIs subsequent to massive bleeding may not experience chest pain.
Perform a complete physical examination, including general appearance and mental status; cardiac examination; pulmonary examination; abdominal examination (including noting surgical scars, distention, auscultation for bruits that may indicate an aneurysm, palpating organ size); and skin changes such as pallor, moisture, telangiectasia, ecchymoses, and petechiae. Rectal examination for hemorrhoids or fissures and stool examination for occult blood are essential.
If hematemesis has not been documented, prepare the nasal passageway and posterior pharynx with topical anesthetic, place a nasogastric tube, and lavage with room temperature normal saline (cold fluids may impede normal coagulation) until aspirate is clear. Persistent bleeding during lavage indicates potential life-threatening upper GI bleeding, and immediate consultation with a gastroenterologist or surgeon should be obtained. Lavage prior to endoscopy may improve visualization during endoscopic procedure, especially in the fundus.
If persistent bleeding is noted and the endoscopist gives instructions to do so, place a nasogastric tube for gastric lavage with increments of 200–300 mL of either saline or tap water. The patient should be in the left lateral decubitus position with the bed in the reverse Trendelenburg position. Lavage until the return is clear. Administration of erythromycin IV will stimulate gastric motility and will also help to clear the stomach of blood prior to endoscopy to improve visualization during the procedure.
If a patient is in shock or has a history of cardiac or renal dysfunction, insert a Foley catheter into the bladder to monitor urinary output. Order a urine analysis to assess for hematuria, which may indicate an abdominal aneurysm.
Patients waiting for endoscopy should receive nothing by mouth. Antacids may impair adequate visualization during endoscopy.
Patients taking Coumadin or those who show signs of hepatic failure (eg, jaundice) may require vitamin K and fresh frozen plasma to correct coagulopathy before bleeding can be controlled.
After initial stabilization of the patient, contact the on-call general surgeon or gastroenterologist for either immediate endoscopy and therapy or further instructions. If emergent endoscopic services are unavailable at the treating facility, the emergency physician should find an accepting physician at a facility capable of providing these services and arrange rapid transport.
On the basis of certain clinical criteria such as age, co-morbid disease, presenting vital signs, laboratory data, and availability of next-day follow-up, a subgroup of patients with GI hemorrhage can be discharged home. This decision should be made with the gastroenterologist. Intensive care unit admission should be reserved for patients with continued bleeding, abnormal vital signs, significant co-morbid disease, or need for transfusion therapy and for those at increased risk for rebleeding (ie, esophageal varices).
Once the patient is stabilized, attempt to determine the bleeding site if it is not already obvious. In 90% of patients presenting with GI hemorrhage, the bleeding has an upper GI source (ie, proximal to the ligament of Treitz). In about 80–85% of patients with GI hemorrhage, the bleeding will cease prior to the patient’s arrival in the emergency department.
(See Figure 16–2) The incidence of upper GI bleeds is 50–150/100,000 with a predominance in males and the elderly.
Hematemesis (excluding hemoptysis or swallowed blood from epistaxis) is observed during upper gastrointestinal bleeding. Nasogastric lavage usually reveals aspirate which is grossly bloody or guaiac positive.
The aspirate will be negative in approximately 10% of patients with a duodenal source of GI hemorrhage. A duodenal source cannot be excluded unless gastric lavage contents reveal bile. Even if bile is returned, the bleeding may have resolved spontaneously prior to arrival. If a patient reports unwitnessed hematemesis and gastric lavage is inconclusive, consultation with a gastroenterologist for early endoscopy is warranted.
Melena is usually due to bleeding from an upper GI source. Hematochezia from an upper source usually indicates severe hemorrhage and corresponds with significant increases in mortality, need for transfusion, complications, and need for surgery.
The incidence of lower GI bleeds is 20/100,000 and are again more frequent in males and the elderly.
Hematochezia is usually due to bleeding distal to the Ligament of Treitz. An upper GI source is found for suspected lower GI bleeding in up to 15% of patients presenting with hematochezia. In these instances, consider aortoenteric fistula (in patients with abdominal aortic aneurysm repair) or duodenal ulcer.
Melena is rarely associated with lower GI bleeding except when motility in the intestinal tract is decreased. Bismuth salicylate and iron supplementation may also result in black stools or pseudo-melena.
When seen as streaks on stool or on toilet paper after wiping, bright red blood usually indicates a hemorrhoidal or anal fissure source of bleeding. If the patient complains of painful bowel movements anal fissures are most likely.
Spontaneous cessation of bleeding occurs in about 80–85% of cases without intervention, although cessation can be intermittent, and bleeding can restart at any time.
Further Evaluation of Gastrointestinal Bleeding
The unstable patient should be rapidly resuscitated and stabilized prior to completing a detailed history and physical examination. Once the patient’s hemodynamic status has stabilized, a more thorough examination should be done. For the patient not in extremis and those otherwise stable, this examination can be performed during the initial assessment.
Inquire about history of GI bleeding, esophageal varices, alcohol or non-steroidal anti-inflammatory drug (NSAID) use, oral anticoagulation, recent weight loss, change in caliber of stools, abdominal aneurysm repair, liver disease, or abdominal surgery. Recent vigorous retching or vomiting prior to onset of hematemesis suggests the presence of Mallory–Weiss tears. Inquire about history of hemorrhoids, anal fissures, or rectal trauma (eg, rectal intercourse, placement of foreign objects in rectum).
In immunocompromised patients, bleeding may be related to Kaposi sarcoma, lymphoma, or cytomegalovirus ulcerations. Visceral Kaposi sarcoma is usually associated with cutaneous lesions.
Reassess vital signs every 15 minutes or more frequently as needed.
Evaluate the patient for any evidence of cardiac dysfunction (ie, murmurs, rubs, gallops, arrhythmias). Listen to the lungs for abnormal sounds that may be suggestive of heart failure or an infectious process.
Tenderness to palpation in the epigastrium is common with gastritis or peptic ulcer disease. Any patient who has had multiple episodes of vomiting may also have diffuse tenderness of the abdomen. Any elderly patient whose complaints of abdominal pain are out of proportion to the examination should be suspected of having mesenteric ischemia. Significant tenderness or peritoneal signs may indicate perforation and warrant immediate surgical consultation. Auscultation of hyperactive bowel sounds may be observed in an upper GI bleed as the presence of blood will stimulate peristalsis.
Examine the patient for signs of chronic liver disease (hepatosplenomegaly, ascites, spider angiomas, enlarged abdominal vessels, jaundice, hepatojugular reflux, asterixis, palmar erythema). Although the presence of liver disease constitutes a higher likelihood of esophageal varices, one should make no assumptions regarding the etiology of the bleeding. GI bleeding will be from another identifiable source in 50% of patients with known esophageal varices. Inspect the patient for surgical scars that indicate previous abdominal surgery or possible vascular repair.
The presence of telangiectasias of the skin (particularly the digits) and lips may indicate Osler–Weber–Rendu disease (hereditary hemorrhagic telangiectasia), which causes GI bleeding secondary to vascular malformations.
Obtain a stool sample for hemoccult testing, and check for evidence of hemorrhoids or anal fissures.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree