GASTRIC OUTLET OBSTRUCTION
CASE SCENARIO
A 60-year-old woman presents with a several-week history of worsening non-bilious emesis and epigastric abdominal pain. She also reports several months of early satiety and decreased appetite and a 15-pound unintentional weight loss over the past 6 months.
Upon examination, the patient is afebrile with normal vital signs. She is a very thin and frail-appearing woman. Her abdomen is soft with focal tympany and tenderness to palpation in the left upper quadrant. There are no palpable abdominal masses. Her laboratory studies are notable for a hypokalemic, hypochloremic metabolic alkalosis.
EPIDEMIOLOGY
The incidence of gastric outlet obstruction (GOO) is not precisely known, though it is likely lower in recent years due to the decrease in peptic ulcer disease (PUD). The clinical entities that cause GOO are generally categorized into two well-defined groups—benign and malignant. Before the identification of Helicobacter pylori (H. pylori) and the advent of H2-receptor antagonists, when PUD was more prevalent, benign causes of GOO were more common than malignant causes. Today, this ratio is reversed, with recent reviews reporting that 50% to 80% of all cases are attributable to an underlying malignancy.1–3 The leading benign cause of GOO remains PUD, although the incidence is very low, with GOO occurring in only approximately 2% of patients with PUD.4,5 In contrast, the incidence of GOO complicating primary pancreatic, gastric, or duodenal malignancy is reported to be as high as 15% to 25%.6
PATHOPHYSIOLOGY
GOO results from either an intrinsic or an extrinsic obstruction of the pyloric channel or duodenum. The underlying disease process dictates the precise mechanism of the obstruction.
In benign causes, the obstruction is typically the result of inflammation, edema, or scarring in the region of the pyloric channel or duodenal bulb. With PUD, the obstruction typically results from acute inflammation and edema or chronic fibrosis and scarring of the pyloric channel or duodenal bulb. Similarly, gastroduodenal involvement with Crohn’s disease can lead to a Crohn’s-related stricture. With pancreatitis, intense peri-pancreatic inflammation and edema can result in inflammation and fibrosis of the adjacent duodenum. In contrast, obstruction secondary to a large gastric polyp, gastric bezoar, gastric volvulus, or migration of a gastrostomy tube represents a discrete mechanical problem.
In the case of gastric and duodenal malignancies, GOO typically results from intrinsic obstruction by the primary tumor. With pancreatic malignancies, GOO is usually secondary to extrinsic compression by the primary tumor, or by metastatic disease at the gastroduodenal junction.
CLINICAL PRESENTATION
Emesis and epigastric pain are the cardinal symptoms of GOO, with each occurring in over 90% of patients. Other commonly seen symptoms include early satiety, abdominal distention, and weight loss.7 Initially, patients have intermittent symptoms that then progress until the obstruction is complete. Malnutrition is a late sign, but can be very profound, particularly in patients with a concomitant malignancy.
The onset of symptoms varies depending on the etiology of the obstruction. Symptoms generally occur abruptly when the obstruction is secondary to conditions such as gastric volvulus, prolapse of a large gastric polyp, or migration of a gastrostomy tube. In contrast, other causes such as ulcer disease and malignancy tend to follow a more indolent course.8
On physical examination, there may be distention or tenderness in the left upper quadrant or epigastrium. A “succussion splash,” elicited by resting the stethoscope over the left upper abdomen and rocking the patient back and forth at the hips, may be heard in the epigastrium and is indicative of retained gastric material.
In both acute and chronic phases of obstruction, persistent emesis can result in severe dehydration and, oftentimes, profound electrolyte abnormalities. The classic electrolyte abnormality that results from nonbilious emesis is a hypokalemic, hypochloremic metabolic alkalosis.
DIFFERENTIAL DIAGNOSIS
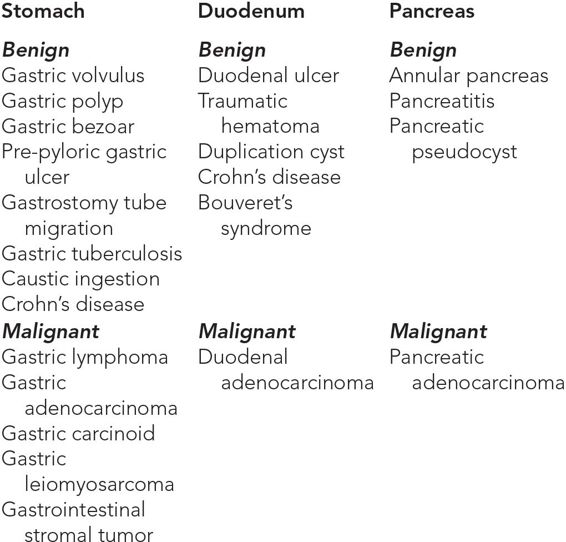
There are several benign and malignant causes of GOO, the most common of which are listed in Table 11–1.
WORKUP AND CHOICE OF IMAGING
The initial management of all patients with suspected GOO should include fluid resuscitation, gastric decompression with a nasogastric tube, and correction of electrolyte abnormalities.
A plain roentogram of the abdomen is a reasonable, inexpensive, and expeditious first imaging study in a patient suspected of having GOO. Plain films of the abdomen classically demonstrate an enlarged gastric bubble, a dilated proximal duodenum, and a paucity of air in the small bowel. However, the plain film is minimally informative in determining the precise underlying etiology of the obstruction.
Water-soluble or barium contrast studies can be useful in the diagnosis of a GOO. A contrast study can provide information regarding the degree of obstruction, with failure of any contrast to pass into the small bowel being suggestive of complete GOO, and may also provide clues to the underlying cause of the obstruction. However, these findings are nonspecific, and this is often a time-consuming examination that many medical centers are not equipped to perform 24 hours a day.9 The risk of aspiration must be considered, and care should be taken to decompress the stomach prior to a proceeding with a contrast study. In the absence of intraperitoneal free air, the contrast agent of choice is barium, with water-soluble contrast being relatively contraindicated due to the morbidity of aspiration pneumonitis.10
Abdominal computed tomography (CT) scan is the most commonly obtained imaging modality and can be extremely informative about the underlying etiology.9,11 Use of appropriately timed oral and intravenous contrast in combination with multi-detector CT scanners allows for a very detailed evaluation of the stomach and pyloric region such that gastric volvulus, gastric polyps, malignancy, and even inflammatory conditions of the stomach and duodenum can be accurately diagnosed on CT scan.
Upper endoscopy can be a useful diagnostic adjunct in cases where the precise etiology of the GOO remains unclear despite radiographic imaging. Upper endoscopy also provides an avenue for certain therapeutic interventions, which will be discussed in further detail later in the chapter. When using endoscopy for diagnostic purposes, the endoscopist will commonly encounter a stomach filled with fluid and undigested food that requires aggressive endoscopic suctioning. Once this has been accomplished, the goal is to visualize the location of the obstruction, at which point the underlying disease process dictates further diagnostic measures. For example, if a gastric or duodenal mass lesion is identified, endoscopic biopsy may confirm or exclude a diagnosis of malignancy. However, such biopsies are not useful if the mass causing obstruction is extraluminal, or if the mucosa is not involved.
IMAGING FINDINGS
 Plain Roentogram
Plain Roentogram
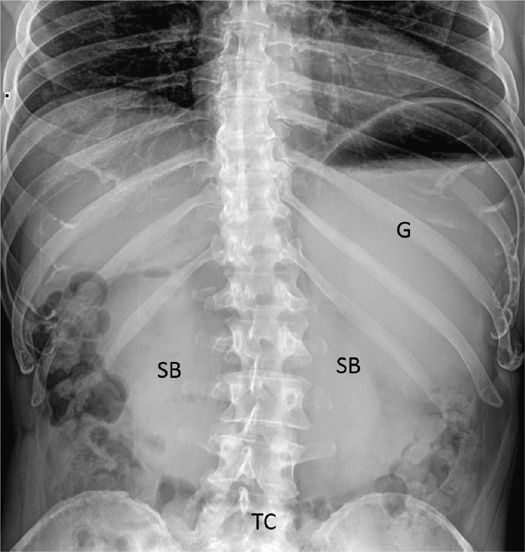
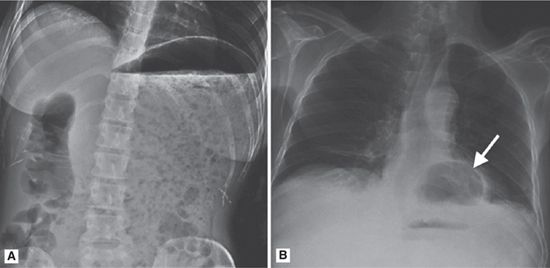
In the case of GOO, a plain film of the abdomen classically demonstrates an enlarged gastric bubble, a dilated proximal duodenum, a paucity of air in the small bowel, and downward displacement of the transverse colon. In certain situations, the plain film may suggest an underlying diagnosis. For example, in the case of a gastric bezoar, particulate matter can be seen filling the stomach. In Bouveret’s syndrome, a calcified gallstone may be seen obstructing the gastric outlet, and in the case of gastric volvulus, a large air bubble and the tip of the nasogastric tube may be visualized in the thorax. However, most commonly, the plain film is minimally informative in determining the precise underlying etiology of the obstruction12 (Table 11–2 and Figures 11–1 through 11–3).
Figure 11–1 Classic plain radiographic of GOO with evidence of massive gastric distention (G), a paucity of gas in the small bowel (SB), and downward displacement of the transverse colon (TC).
Figure 11–2 In certain cases a plain radiograph may provide insight into the etiology of the GOO. (A) In this case the patient has a very dilated stomach and GOO secondary to a pasta bezoar. (B) In this plain radiograph, there is a large air bubble in the chest (arrow) indicative of a herniated stomach and possibly a gastric volvulus.
Figure 11–3 Note the abnormal nasogastric tube location in these plain radiographs of patients with GOO. (A) In this case, the tip of the nasogastric tube is in the left lower quadrant (arrow) indicating massive gastric distension. Another clue is the downward displacement of the transverse colon (TC). (B) In this case of gastric volvulus, the tip of the nasogastric tube (arrow) is located in the mid thorax overlying the herniated and volvulized stomach.
 Contrast Series
Contrast Series
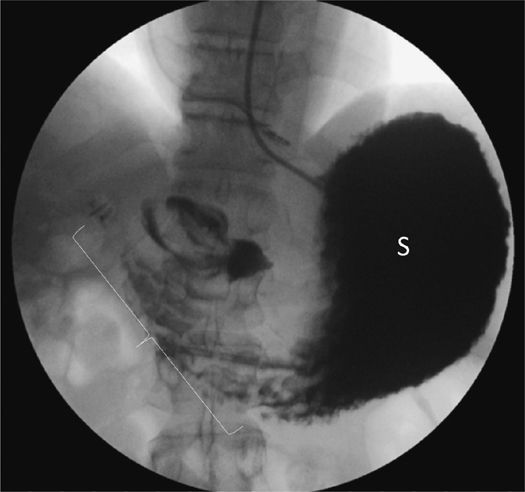
A fluoroscopic contrast study or upper gastrointestinal series may demonstrate an enlarged stomach with a narrowing of the pyloric channel. The degree of obstruction can be ascertained based on how much contrast passes through the gastric outlet. The contrast study is particularly helpful in the case of a gastric volvulus, as it will demonstrate the herniated stomach above the diaphragm and may also provide information regarding which type of volvulus is present (organoaxial versus mesenteroaxial) (Table 11–3 and Figures 11–4 through 11–6).
Figure 11–4 Barium contrast study demonstrating an enlarged stomach (S) with narrowing of the pyloric channel (bracket) secondary to scarring and fibrosis from an antral ulcer.
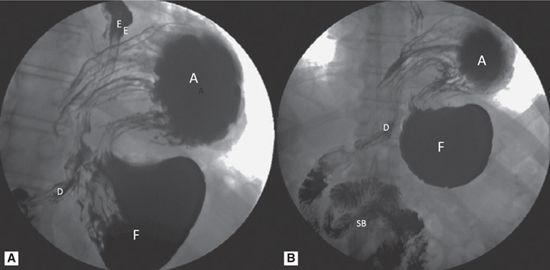
Figure 11–5 Contrast study demonstrating GOO secondary to a paraesophageal hernia with the antrum (A) herniated through the diaphragm into the chest. There are two types of gastric volvulus that can occur, namely, organoaxial and mesenteroaxial. In organoaxial volvulus (shown here), which accounts for about 60% of all cases,13 the twist occurs along a line connecting the cardia and the pylorus or along the long axis of the stomach. In mesenteroaxial volvulus, the twist occurs around a plain perpendicular to the long axis of the stomach from the lesser to the greater curvature. D, duodenum; E, esophagus; F, fundus; SB, small bowel.
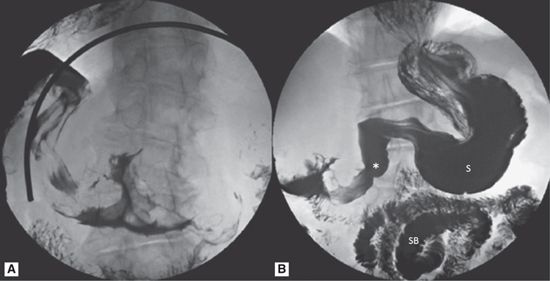
Figure 11–6 Contrast study demonstrating GOO secondary to a duodenal lymphoma. Note that the obstruction is not complete, as contrast is seen passing into the distal duodenum and small bowel. However, there does appear to be a rounded mass in the proximal duodenum (asterisk), causing a partial GOO and dilatation of the first part of the duodenum. S, stomach; SB, small bowel.
 Abdominal Computed Tomography
Abdominal Computed Tomography
In the majority of cases, the abdominal CT scan is the most informative study in the evaluation and diagnosis of GOO. The stomach will appear dilated and filled with fluid or air, sometimes with an air-fluid level. The degree of obstruction can be estimated based on the amount of oral contrast passing beyond the gastric outlet.
In addition to these more general findings of GOO, CT scan can provide information regarding the underlying cause. For example, in peptic ulcer disease there may be significant inflammation seen at the gastric outlet. With a gastric volvulus, the herniated stomach appears in the chest. A particulate matter–filled stomach is a classic finding in gastric bezoar. For Bouveret’s syndrome, a calcified gallstone may be seen obstructing the gastric outlet. Finally, a mass lesion (such as gastric carcinoma, lymphoma, or stromal tumor) may be visible. In these cases, clues in the remainder of the abdomen (such as drop metastases in the case of gastric cancer) should be sought to confirm the diagnosis (Table 11–4 and Figures 11–7 through 11–14).