CHAPTER 72
Foreign Body, Swallowed
Presentation
Parents bring in a young child (usually between the ages of 6 months and 6 years) shortly after the child has swallowed a coin, safety pin, or toy. The child may be asymptomatic or have recurrent or transient symptoms of choking, gagging, vomiting, drooling, dysphagia, pain, or a foreign body (FB) sensation. Stridor or dyspnea resulting from tracheal compression may occur in young children. Disturbed or cognitively impaired adults may be brought from mental health facilities to the hospital on repeated occasions, at times accumulating a sizable load of ingested material. Impacted esophageal foreign bodies are more likely to cause the symptoms described, whereas gastric foreign bodies are usually asymptomatic.
What To Do:
 Many patients are able to give a clear history of foreign body ingestion; however, young children, psychotic persons, and the cognitively impaired may be unable to give an accurate history.
Many patients are able to give a clear history of foreign body ingestion; however, young children, psychotic persons, and the cognitively impaired may be unable to give an accurate history.
 Ask capable patients about their symptoms and examine them, looking for signs of airway obstruction (e.g., coughing, wheezing), bowel obstruction, or perforation (e.g., vomiting, subcutaneous emphysema, chest pain, melena, abdominal pain, abnormal bowel sounds).
Ask capable patients about their symptoms and examine them, looking for signs of airway obstruction (e.g., coughing, wheezing), bowel obstruction, or perforation (e.g., vomiting, subcutaneous emphysema, chest pain, melena, abdominal pain, abnormal bowel sounds).
 When a foreign body ingestion is suspected, obtain posteroanterior and lateral radiographic views of the throat and chest to at least the midabdomen to determine if indeed anything was ingested or if the FB has become lodged or produced an obstruction. In small children, this should include the area from the nasopharynx to the upper abdomen, which can often be done with a single large radiographic plate. A lateral view will not be necessary if the FB is in the stomach or if it is discovered that no object has actually been swallowed.
When a foreign body ingestion is suspected, obtain posteroanterior and lateral radiographic views of the throat and chest to at least the midabdomen to determine if indeed anything was ingested or if the FB has become lodged or produced an obstruction. In small children, this should include the area from the nasopharynx to the upper abdomen, which can often be done with a single large radiographic plate. A lateral view will not be necessary if the FB is in the stomach or if it is discovered that no object has actually been swallowed.
 A coin located in the proximal esophagus will be oriented in the coronal plane on an anteroposterior projection. Tracheal foreign bodies align in the sagittal plane on a lateral projection (Figure 72-1). Button batteries, which can be hazardous, can be differentiated from a simple coin by their “double ring” appearance on radiographs.
A coin located in the proximal esophagus will be oriented in the coronal plane on an anteroposterior projection. Tracheal foreign bodies align in the sagittal plane on a lateral projection (Figure 72-1). Button batteries, which can be hazardous, can be differentiated from a simple coin by their “double ring” appearance on radiographs.
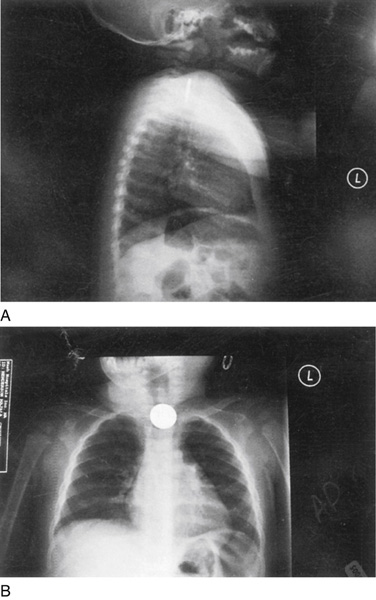
Figure 72-1 Posteroanterior and lateral combined radiograph views of the chest and neck revealing an upper esophageal coin. (Adapted from Nicholson J: Occult ingestion of foreign body. Emerg Phys Monthly April 2005.)
 Many foreign bodies are radiolucent; therefore a negative radiograph does not rule out a foreign body.
Many foreign bodies are radiolucent; therefore a negative radiograph does not rule out a foreign body.
 A foreign body with sharp edges or a blunt FB lodged in the esophagus for more than a day should be removed endoscopically, because it is likely to cause a perforation and is still accessible. Button or disk batteries that are impacted in the esophagus can rapidly cause tissue necrosis and perforation and therefore must be removed on an emergent basis. Once a button battery has cleared the esophagus, it will usually traverse the remainder of the gastrointestinal tract (GI) without difficulty and would only need to be removed if there were signs and symptoms of gastrointestinal injury, if the battery was larger than 20 mm in diameter, or if it failed to pass the pylorus after 48 hours.
A foreign body with sharp edges or a blunt FB lodged in the esophagus for more than a day should be removed endoscopically, because it is likely to cause a perforation and is still accessible. Button or disk batteries that are impacted in the esophagus can rapidly cause tissue necrosis and perforation and therefore must be removed on an emergent basis. Once a button battery has cleared the esophagus, it will usually traverse the remainder of the gastrointestinal tract (GI) without difficulty and would only need to be removed if there were signs and symptoms of gastrointestinal injury, if the battery was larger than 20 mm in diameter, or if it failed to pass the pylorus after 48 hours.
 Many sharp, pointed, and elongated FBs should be removed even if they have passed into the stomach. Examples include toothpicks, medication blister packs, open safety pins, toothbrushes, plastic bag clips, and elongated nails and wires. FBs longer than 6 cm in children (3 cm in infants) and 10 cm in adults should be removed. Toothpicks are shorter than this, but they are associated with a high incidence of perforation. Plastic bag clips have a propensity to attach to the folds of the small bowel with subsequent small bowel ulceration and the potential for hemorrhage, perforation, and healing with fibrosis and obstruction.
Many sharp, pointed, and elongated FBs should be removed even if they have passed into the stomach. Examples include toothpicks, medication blister packs, open safety pins, toothbrushes, plastic bag clips, and elongated nails and wires. FBs longer than 6 cm in children (3 cm in infants) and 10 cm in adults should be removed. Toothpicks are shorter than this, but they are associated with a high incidence of perforation. Plastic bag clips have a propensity to attach to the folds of the small bowel with subsequent small bowel ulceration and the potential for hemorrhage, perforation, and healing with fibrosis and obstruction.
 A child who is brought in immediately after ingesting a coin and is asymptomatic but has a coin impacted in the upper or lower esophagus can initially be fed soft bread with clear fluids and observed for several hours to see if the coin will spontaneously pass into the stomach. If this is unsuccessful, consult with the parents, along with a pediatric endoscopist, regarding further observation for up to 24 hours as an outpatient or inpatient, or possibly performing endoscopic removal as soon as possible.
A child who is brought in immediately after ingesting a coin and is asymptomatic but has a coin impacted in the upper or lower esophagus can initially be fed soft bread with clear fluids and observed for several hours to see if the coin will spontaneously pass into the stomach. If this is unsuccessful, consult with the parents, along with a pediatric endoscopist, regarding further observation for up to 24 hours as an outpatient or inpatient, or possibly performing endoscopic removal as soon as possible.
 When a coin or other smooth object has been lodged in the upper esophagus of a healthy asymptomatic child for less than 24 hours, and endoscopy is not readily available and the parents are supportive about avoiding general anesthesia, the object can often be removed using a simple Foley catheter technique. When available, this can be performed under fluoroscopy; although, to avoid this radiation, it can be safely performed as a blind procedure. With the patient mildly sedated (e.g., midazolam [Versed], 0.5 mg/kg per rectum, intranasally or PO, with a half hour allowed for absorption), position the child with the head down (Trendelenburg) and prone to minimize the risk for aspiration. Alternatively, consider ketamine for procedural sedation (see Appendix E). Have a functioning laryngoscope, Magill forceps, and airway equipment at hand. Test the balloon of an 8- to 12-Fr Foley catheter to ensure that it inflates symmetrically. Lubricate the catheter with water-soluble jelly and insert it through the nose into the esophagus to a point distal to the FB. Inflate the balloon with 5 mL of air and apply gentle traction on the catheter until the foreign body reaches the base of the tongue. Terminate the procedure if you encounter any resistance. The patient will reflexively gag, cough, or spit out the foreign body. Immediately deflate the balloon and remove the catheter (Figure 72-2). If a first attempt at removal fails, consult an endoscopist. When removal is successful, repeat the radiograph to be sure that there are no additional coins, and discharge the patient after a brief period of observation.
When a coin or other smooth object has been lodged in the upper esophagus of a healthy asymptomatic child for less than 24 hours, and endoscopy is not readily available and the parents are supportive about avoiding general anesthesia, the object can often be removed using a simple Foley catheter technique. When available, this can be performed under fluoroscopy; although, to avoid this radiation, it can be safely performed as a blind procedure. With the patient mildly sedated (e.g., midazolam [Versed], 0.5 mg/kg per rectum, intranasally or PO, with a half hour allowed for absorption), position the child with the head down (Trendelenburg) and prone to minimize the risk for aspiration. Alternatively, consider ketamine for procedural sedation (see Appendix E). Have a functioning laryngoscope, Magill forceps, and airway equipment at hand. Test the balloon of an 8- to 12-Fr Foley catheter to ensure that it inflates symmetrically. Lubricate the catheter with water-soluble jelly and insert it through the nose into the esophagus to a point distal to the FB. Inflate the balloon with 5 mL of air and apply gentle traction on the catheter until the foreign body reaches the base of the tongue. Terminate the procedure if you encounter any resistance. The patient will reflexively gag, cough, or spit out the foreign body. Immediately deflate the balloon and remove the catheter (Figure 72-2). If a first attempt at removal fails, consult an endoscopist. When removal is successful, repeat the radiograph to be sure that there are no additional coins, and discharge the patient after a brief period of observation.
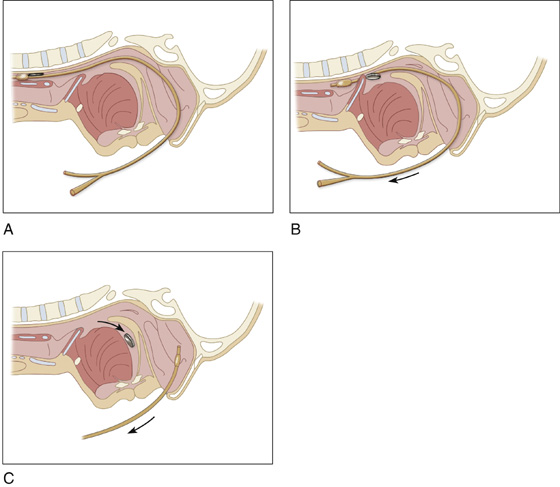
Figure 72-2 Foley catheter technique.
 Also, when there is parental support, esophageal bougienage is a safe, effective, and inexpensive method to advance coins or smooth objects from the distal esophagus into the stomach without sedation. After topical anesthesia of the throat, wrap the patient in a bed sheet with arms at the side and have an assistant hold the child upright. Advance a well-lubricated, blunt, round-tipped Hurst-type esophageal dilator through the mouth and esophagus into the stomach, then remove it. Obtain a postprocedure radiograph of the chest and upper abdomen to document the location of the FB. Esophageal bougienage should be limited to witnessed ingestions of a single coin lodged for less than 24 hours with no previous history of esophageal FB, disease, or surgery and no respiratory compromise. Dilator size should be 28 Fr for ages 1 to 2, 32 Fr for ages 2 to 3, 36 Fr for ages 3 to 4, 38 Fr for ages 4 to 5, and 40 Fr for those older than 5 years of age. These two rapid, simple, cost-effective techniques have been shown in the past to be safe and effective. Because of the lack of direct visual control and the potential for injury or aspiration, however, many clinicians forgo these procedures and take advantage of the widespread availability of flexible endoscopy when dealing with esophageal FBs.
Also, when there is parental support, esophageal bougienage is a safe, effective, and inexpensive method to advance coins or smooth objects from the distal esophagus into the stomach without sedation. After topical anesthesia of the throat, wrap the patient in a bed sheet with arms at the side and have an assistant hold the child upright. Advance a well-lubricated, blunt, round-tipped Hurst-type esophageal dilator through the mouth and esophagus into the stomach, then remove it. Obtain a postprocedure radiograph of the chest and upper abdomen to document the location of the FB. Esophageal bougienage should be limited to witnessed ingestions of a single coin lodged for less than 24 hours with no previous history of esophageal FB, disease, or surgery and no respiratory compromise. Dilator size should be 28 Fr for ages 1 to 2, 32 Fr for ages 2 to 3, 36 Fr for ages 3 to 4, 38 Fr for ages 4 to 5, and 40 Fr for those older than 5 years of age. These two rapid, simple, cost-effective techniques have been shown in the past to be safe and effective. Because of the lack of direct visual control and the potential for injury or aspiration, however, many clinicians forgo these procedures and take advantage of the widespread availability of flexible endoscopy when dealing with esophageal FBs.
 FBs of the esophagus are more difficult to remove when prolonged impaction leads to mucosal edema, swelling, and necrosis. It is for this reason that Foley catheter manipulation and bougienage are not recommended for coins that have been entrapped for more than 24 hours.
FBs of the esophagus are more difficult to remove when prolonged impaction leads to mucosal edema, swelling, and necrosis. It is for this reason that Foley catheter manipulation and bougienage are not recommended for coins that have been entrapped for more than 24 hours.
 Children with distal esophageal coins may be safely observed up to 24 hours before an invasive removal procedure, because most will spontaneously pass the coins.
Children with distal esophageal coins may be safely observed up to 24 hours before an invasive removal procedure, because most will spontaneously pass the coins.
 When an FB has passed into the stomach and there are no symptoms or hazardous circumstances that demand immediate removal, discharge the patient with instructions to return for reevaluation in 3 to 4 days (2 days with button batteries) or sooner if the child develops nausea, vomiting, fever, abdominal pain, rectal pain, or rectal bleeding.
When an FB has passed into the stomach and there are no symptoms or hazardous circumstances that demand immediate removal, discharge the patient with instructions to return for reevaluation in 3 to 4 days (2 days with button batteries) or sooner if the child develops nausea, vomiting, fever, abdominal pain, rectal pain, or rectal bleeding.
 For potentially hazardous radiopaque objects, repeat radiographs every 3 to 4 days to confirm that passage of the object is necessary. This would not be required for small, smooth objects such as coins.
For potentially hazardous radiopaque objects, repeat radiographs every 3 to 4 days to confirm that passage of the object is necessary. This would not be required for small, smooth objects such as coins.
 All subdiaphragmatic coins seem to pass without incident. Metal detectors can be used to follow the elimination of metallic FBs without further radiation exposure. Having parents sift through stools is often unproductive. (One missed stool negates days of hard work.) It may be helpful to give a bulk laxative to help decrease the intestinal transit time.
All subdiaphragmatic coins seem to pass without incident. Metal detectors can be used to follow the elimination of metallic FBs without further radiation exposure. Having parents sift through stools is often unproductive. (One missed stool negates days of hard work.) It may be helpful to give a bulk laxative to help decrease the intestinal transit time.
What Not To Do:
 Do not use ipecac for FB ingestions. Emesis is effective for emptying the stomach of liquid but not for removing FBs from the esophagus or stomach. It may even result in regurgitation of a gastric disk battery into the esophagus, where it will be much more hazardous.
Do not use ipecac for FB ingestions. Emesis is effective for emptying the stomach of liquid but not for removing FBs from the esophagus or stomach. It may even result in regurgitation of a gastric disk battery into the esophagus, where it will be much more hazardous.
 Do not forcefully remove an esophageal FB, especially if it is causing pain. This removal may lead to injury or perforation.
Do not forcefully remove an esophageal FB, especially if it is causing pain. This removal may lead to injury or perforation.
 Do not worry about the corrosive properties of pennies minted in the United States since 1982, that is, with a high (97.5%) zinc content. Although concerns have been raised in the medical and popular press, they are not associated with more esophageal mucosal injuries than other coins are.
Do not worry about the corrosive properties of pennies minted in the United States since 1982, that is, with a high (97.5%) zinc content. Although concerns have been raised in the medical and popular press, they are not associated with more esophageal mucosal injuries than other coins are.
 Do not automatically assume that an ingested FB should be surgically removed. Most potentially injurious FBs pass through the alimentary tract without mishap. Operate only when the patient is actually being harmed by the swallowed FB or when there is evidence that it is not moving down the alimentary tract.
Do not automatically assume that an ingested FB should be surgically removed. Most potentially injurious FBs pass through the alimentary tract without mishap. Operate only when the patient is actually being harmed by the swallowed FB or when there is evidence that it is not moving down the alimentary tract.
 Do not miss additional coins after removing one from the proximal esophagus. Take a repeat radiograph after removal of one coin.
Do not miss additional coins after removing one from the proximal esophagus. Take a repeat radiograph after removal of one coin.
 Do not routinely refer children with esophageal coins for an additional investigation to look for underlying disease. This is a common occurrence in normal children.
Do not routinely refer children with esophageal coins for an additional investigation to look for underlying disease. This is a common occurrence in normal children.
 Do not ignore the potential hazards of button battery ingestions (see Discussion). Button batteries in the esophagus demand emergent removal.
Do not ignore the potential hazards of button battery ingestions (see Discussion). Button batteries in the esophagus demand emergent removal.
 In the patient who presents with food (usually meat) bolus impaction, never use meat tenderizer.
In the patient who presents with food (usually meat) bolus impaction, never use meat tenderizer.
Discussion
Older children and fully conscious, communicative adults may be able to identify the material swallowed and point to the location of the discomfort. Localization of the level of impaction, however, is often not reliable. In many instances, the ingestion goes unrecognized or unreported until the onset of symptoms, which may be remote from the time of ingestion. Young children, the cognitively impaired, or psychiatric patients may present with choking, refusal to eat, vomiting, drooling, wheezing, blood-stained saliva, or respiratory distress.
FB ingestion is most common in children 6 months to 6 years of age, who comprise 75% to 80% of all cases. Coins are the most common FBs in children. Other FBs in children include fish bones, marbles, buttons, button batteries, screws, pins, paper clips, crayons, pen and bottle caps, and small toys. In adults, meat boluses, bones, coins, dentures, fruit pits, and toothpicks are commonly encountered. Ingestion of foreign objects occurs most often in edentulous adults and in individuals with psychiatric conditions, mental retardation, or chemical dependency. Intentional ingestion of various FBs is encountered commonly in prisoners and patients with psychiatric disorders.
Although most coins swallowed by healthy children pass through the gastrointestinal tract without difficulty, patients with previous GI tract surgery or congenital gut malformations are at increased risk for obstruction or perforation. As with coins, most other swallowed FBs in children and adults will traverse the GI tract without difficulty and require no intervention.
The narrowest and least distensible strait in the gastrointestinal tract is usually the cricopharyngeus muscle at the level of the thyroid cartilage. Next narrowest is usually the pylorus, followed by the lower esophageal sphincter and the ileocecal valve. Thus anything that passes the throat will probably pass through the anus as well (although all of these sites are potential locations for FB impaction). In general, FBs below the diaphragm should be left alone.
Complications are related to the type of FB and are more common if it remains entrapped more than 24 hours. These include inconsequential mucosal scratches or abrasions, lacerations, esophageal stricture, esophageal necrosis, retropharyngeal abscess formation, hemorrhage, obstruction, and perforation.
A significant portion of children with esophageal FBs are asymptomatic; therefore any child suspected of ingesting an FB requires radiography to document whether or not it is present, and, if so, where it is located.
Large button batteries (the size of quarters) have become stuck in the esophagus, eroded through the esophageal wall, and produced fatal exsanguination, but the smaller variety and batteries that have passed into the gut have not posed such a danger. A button battery lodged in the esophagus should be considered a true emergency and removed immediately by an endoscopist. A button battery found in the stomach should be allowed to pass spontaneously. Smaller batteries need only weekly radiographic follow-up; the larger ones should be checked every 48 hours. Failure to pass the pylorus within 2 days is an indication for endoscopic removal. The maximum GI transit time for such FBs in children is 5 days.
Any child with respiratory distress should have the coin removed promptly. Time will probably not allow this to be done under ideal conditions in the operating room. Rapid removal using a McIntosh laryngoscope blade to expose the esophageal entrance and then extracting the coin from the esophagus has been described. Ketamine has been shown to be effective without significant complications in one study that demonstrated its use in the removal of esophageal FBs in pediatric patients. Under critical conditions, combining these two modalities may be quite helpful.
In adults, esophageal body obstruction is most typically caused by a meat bolus impaction. The upper esophageal sphincter, level of the aortic arch, or the diaphragmatic hiatus are all anatomically narrow and a food bolus may therefore become impacted at any of these sites. Patients with total obstruction, who have inability to pass their secretions, should be treated within 12 hours because of the risk of pulmonary aspiration. A trial of glucagon 1.0 mg IV, administered slowly to avoid nausea and vomiting, may be used in attempt to relax the esophagus. If this is ineffectual, endoscopy allows removal of the impacted food bolus, as well as evaluation of concomitant causative conditions, such as esophageal carcinoma, stricture, achalasia, or eosinophilic esophagitis. Patients who pass a food bolus without endoscopy should be referred for later endoscopy to evaluate for causative conditions.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


