CHAPTER 29
Foreign Body, Nose
Presentation
Most commonly, a child may admit to his parents that he has inserted something into his nose or someone observed him doing this. Sometimes, however, the history is obscure, and the child presents with local pain; a purulent, unilateral nasal discharge; epistaxis; a nasal voice change; or foul breath. The most commonly encountered nasal foreign bodies are beans, peanuts or other foodstuffs, beads, toy parts, pebbles, paper wads, and eraser tips. Most foreign bodies (FBs) can be seen on direct visualization using a nasal or otoscope speculum. These objects usually lodge on the floor of the nose just below the inferior turbinate or immediately anterior to the middle turbinate.
What To Do:
 There are various techniques available for removal of nasal FBs. These include suction, air pressure, ear curettes, curved hooks, alligator forceps, bayonet forceps, balloon catheters, irrigation and glue. The choice will depend of the shape, makeup, and depth of the FB as well as the age and cooperation of the patient.
There are various techniques available for removal of nasal FBs. These include suction, air pressure, ear curettes, curved hooks, alligator forceps, bayonet forceps, balloon catheters, irrigation and glue. The choice will depend of the shape, makeup, and depth of the FB as well as the age and cooperation of the patient.
 Before attempting removal techniques in an uncooperative patient, consider use of sedation. Be aware of the higher risk of aspiration of the FB when sedation is used.
Before attempting removal techniques in an uncooperative patient, consider use of sedation. Be aware of the higher risk of aspiration of the FB when sedation is used.
 Because of the potential for spraying of body fluids from the nose, always practice universal precautions and wear appropriate eye and splash protection.
Because of the potential for spraying of body fluids from the nose, always practice universal precautions and wear appropriate eye and splash protection.
 Before any of the removal procedures, explain in detail what you are about to do to the patient and or parent. Advise that the procedure will be a little uncomfortable, may cause some bleeding and that there is a small risk the FB body could be aspirated. Have advanced airway equipment in the room, including a McGill forceps.
Before any of the removal procedures, explain in detail what you are about to do to the patient and or parent. Advise that the procedure will be a little uncomfortable, may cause some bleeding and that there is a small risk the FB body could be aspirated. Have advanced airway equipment in the room, including a McGill forceps.
 After initial inspection with a nasal speculum and bright light, suction out any discharge, and insert a small cotton pledget soaked in 4% cocaine or alternatively a 1:1 mixture of phenylephrine (Neo-Synephrine) and tetracaine (Pontocaine), which will shrink the nasal mucosa and provide topical anesthesia.
After initial inspection with a nasal speculum and bright light, suction out any discharge, and insert a small cotton pledget soaked in 4% cocaine or alternatively a 1:1 mixture of phenylephrine (Neo-Synephrine) and tetracaine (Pontocaine), which will shrink the nasal mucosa and provide topical anesthesia.
 Be careful to avoid pushing the FB posteriorly when inserting the pledget. Remove the pledget after 5 to 10 minutes. If you cannot safely insert a pledget, drip or spray the same solution into the nose.
Be careful to avoid pushing the FB posteriorly when inserting the pledget. Remove the pledget after 5 to 10 minutes. If you cannot safely insert a pledget, drip or spray the same solution into the nose.
 After vasoconstriction, some FBs can be blown out of the nose by a cooperative patient or suctioned out, using Frazier tip suction. Further suctioning success may be obtained by placing a piece of soft plastic tubing over the end of the suction tip. Placing water-soluble lubrication on the end of this tubing will also help achieve a better vacuum seal.
After vasoconstriction, some FBs can be blown out of the nose by a cooperative patient or suctioned out, using Frazier tip suction. Further suctioning success may be obtained by placing a piece of soft plastic tubing over the end of the suction tip. Placing water-soluble lubrication on the end of this tubing will also help achieve a better vacuum seal.
 In infants and children who will not blow their nose on command, a parent may blow a sharp puff of air into the child’s mouth while holding the opposite nostril closed. A tight-fitting Ambu mask over the mouth and a bag-valve device is an alternative means for producing the positive pressure required to force the FB out of the nose.
In infants and children who will not blow their nose on command, a parent may blow a sharp puff of air into the child’s mouth while holding the opposite nostril closed. A tight-fitting Ambu mask over the mouth and a bag-valve device is an alternative means for producing the positive pressure required to force the FB out of the nose.
 Another air pressure technique is to place oxygen tubing, running at 10 to 15 L/min, into the contralateral nostril to the FB (Beamsley Blaster) (Figure 29-1). This technique, along with the other positive-pressure ones, reduces the risk for forcing the FB posteriorly, thereby reducing the risk of aspiration. These methods may not work as well for FBs that have produced edema or infection.
Another air pressure technique is to place oxygen tubing, running at 10 to 15 L/min, into the contralateral nostril to the FB (Beamsley Blaster) (Figure 29-1). This technique, along with the other positive-pressure ones, reduces the risk for forcing the FB posteriorly, thereby reducing the risk of aspiration. These methods may not work as well for FBs that have produced edema or infection.
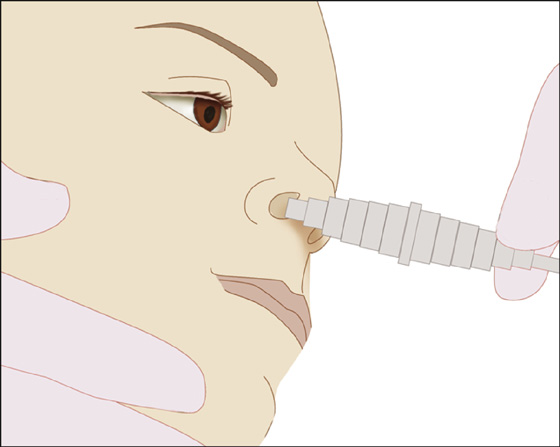
Figure 29-1 Beamsley Blaster technique.
 Alligator forceps may be used to remove cloth, cotton, or paper FBs. Pebbles, beans, and other hard FBs are most easily grasped using bayonet forceps.
Alligator forceps may be used to remove cloth, cotton, or paper FBs. Pebbles, beans, and other hard FBs are most easily grasped using bayonet forceps.
 If an object cannot be grasped, it may be rolled out of the nose by using an ear curette or right-angle ear hook to get behind it. After sliding the tool past the FB, twist until it catches the FB and then pull anteriorly. A soft-tipped hook can be made by bending the tip of a metal Calgiswab to a 90-degree angle.
If an object cannot be grasped, it may be rolled out of the nose by using an ear curette or right-angle ear hook to get behind it. After sliding the tool past the FB, twist until it catches the FB and then pull anteriorly. A soft-tipped hook can be made by bending the tip of a metal Calgiswab to a 90-degree angle.
 A less intrusive approach is to bypass the FB with a lubricated 5-Fogarty biliary balloon probe or small Foley catheter, inflating the balloon with 1 mL of air and gently pulling the catheter and FB out of the nose (Figure 29-2). A commercially available FB remover, the Katz Extractor (InHealth Technologies, Carpinteria, Calif.), may offer an easier balloon catheter technique, but not necessarily be the least expensive device.
A less intrusive approach is to bypass the FB with a lubricated 5-Fogarty biliary balloon probe or small Foley catheter, inflating the balloon with 1 mL of air and gently pulling the catheter and FB out of the nose (Figure 29-2). A commercially available FB remover, the Katz Extractor (InHealth Technologies, Carpinteria, Calif.), may offer an easier balloon catheter technique, but not necessarily be the least expensive device.
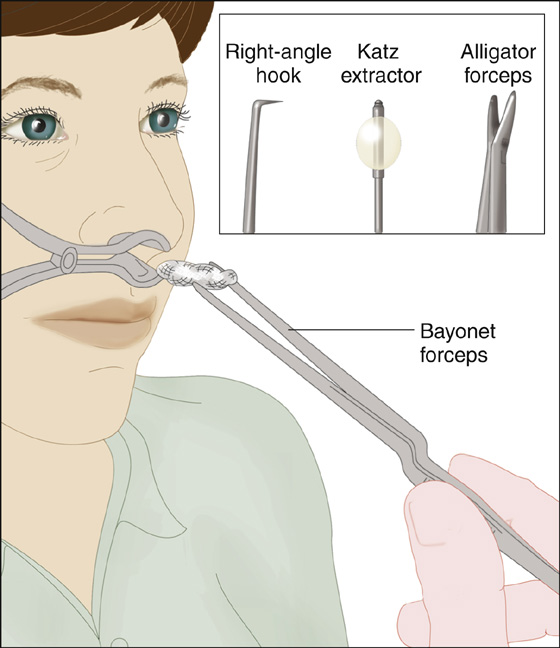
Figure 29-2 Remove foreign bodies with bayonet forceps, right-angle hook, Katz extractor, or alligator forceps.
 One can also try the glue technique. After drying the exposed surface of the FB, a drop of cyanoacrylate (Super Glue, Dermabond) can be applied to the cotton end of a regular cotton-tipped applicator, which is then touched to the FB, held there for 1 minute, and used to pull the attached FB out of the nose.
One can also try the glue technique. After drying the exposed surface of the FB, a drop of cyanoacrylate (Super Glue, Dermabond) can be applied to the cotton end of a regular cotton-tipped applicator, which is then touched to the FB, held there for 1 minute, and used to pull the attached FB out of the nose.
 Button batteries can cause serious local damage through liquefaction necrosis and should be removed quickly. Button batteries of all sizes have a distinctive double contour on radiographs; therefore, with a high index of suspicion, radiographs can help assist with an uncertain diagnosis.
Button batteries can cause serious local damage through liquefaction necrosis and should be removed quickly. Button batteries of all sizes have a distinctive double contour on radiographs; therefore, with a high index of suspicion, radiographs can help assist with an uncertain diagnosis.
 Earring magnets that become stuck together across the nasal septum must also be removed as soon as possible because of the risk for pressure necrosis leading to septal perforation. Ideally, the septum should be lubricated. Using the balloon catheter technique bilaterally, both magnets should be removed simultaneously to prevent a lone magnet from dropping back into the nasopharynx and being aspirated.
Earring magnets that become stuck together across the nasal septum must also be removed as soon as possible because of the risk for pressure necrosis leading to septal perforation. Ideally, the septum should be lubricated. Using the balloon catheter technique bilaterally, both magnets should be removed simultaneously to prevent a lone magnet from dropping back into the nasopharynx and being aspirated.
 Bleeding, which will often occur during FB removal, can usually be stopped by reinsertion of a cotton pledget soaked in the topical solution used prior to the procedure.
Bleeding, which will often occur during FB removal, can usually be stopped by reinsertion of a cotton pledget soaked in the topical solution used prior to the procedure.
 Small, particulate material may be irrigated from the nasal cavity by insertion of an irrigation syringe into one nostril while the patient sits up, leans forward, and repeats “eng” as you irrigate. The “eng” sound will close the back of the throat during irrigation. Slowly flush the debris out the opposite nostril (Figure 29-3).
Small, particulate material may be irrigated from the nasal cavity by insertion of an irrigation syringe into one nostril while the patient sits up, leans forward, and repeats “eng” as you irrigate. The “eng” sound will close the back of the throat during irrigation. Slowly flush the debris out the opposite nostril (Figure 29-3).
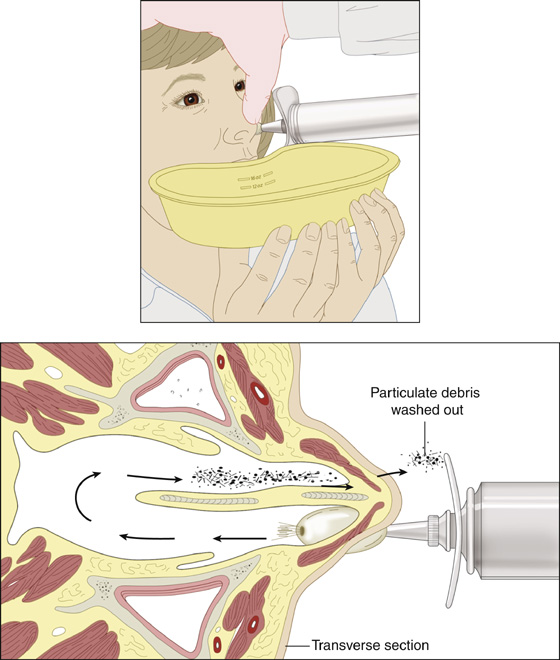
Figure 29-3 Nasal irrigation.
 After FB removal, inspect the nasal cavity again, checking for additional objects. Always look in the other nostril, and it may be wise to check the ears.
After FB removal, inspect the nasal cavity again, checking for additional objects. Always look in the other nostril, and it may be wise to check the ears.
 If a foreign body cannot be located, but is suspected, or if attempts to remove a visible FB have failed, an ear-nose-throat (ENT) consultation is warranted.
If a foreign body cannot be located, but is suspected, or if attempts to remove a visible FB have failed, an ear-nose-throat (ENT) consultation is warranted.
What Not To Do:
 Do not inspect the nasal cavity by opening the nasal speculum in the horizontal plane. The speculum should be opened in the vertical plane and not pressed against the nasal septum.
Do not inspect the nasal cavity by opening the nasal speculum in the horizontal plane. The speculum should be opened in the vertical plane and not pressed against the nasal septum.
 Do not ignore unilateral nasal discharge in a child. It must be assumed to be caused by the presence of a FB until proven otherwise.
Do not ignore unilateral nasal discharge in a child. It must be assumed to be caused by the presence of a FB until proven otherwise.
 Do not push a FB down the back of a patient’s throat by attempting to remove a large, solid, smooth FB with alligator or bayonet forceps. It may be aspirated into the trachea.
Do not push a FB down the back of a patient’s throat by attempting to remove a large, solid, smooth FB with alligator or bayonet forceps. It may be aspirated into the trachea.
 Do not attempt to remove a FB from the nose without first using a topical anesthetic and vasoconstrictor.
Do not attempt to remove a FB from the nose without first using a topical anesthetic and vasoconstrictor.
 Do not leave a button battery in the nose or magnets across the nasal tissue. These objects can cause quick tissue necrosis and must be removed as soon as possible. If you suspect a button battery in the nose but cannot find it, consider a radiograph for confirmation.
Do not leave a button battery in the nose or magnets across the nasal tissue. These objects can cause quick tissue necrosis and must be removed as soon as possible. If you suspect a button battery in the nose but cannot find it, consider a radiograph for confirmation.
The symptoms produced by a nasal FB will vary with its size, composition, location, and the length of time it has been present. Most nasal foreign bodies can be removed easily and safely by emergency clinicians. There is generally no need for emergent intervention. There is time available to provide procedural sedation, if necessary, as well as to assemble all of the supplies and instruments necessary to help ensure the success of this procedure. Because nasal FBs have different sizes, shapes, and locations within the nares, the emergency clinician should be familiar with several removal techniques.
The mucous membrane lining the nasal cavity allows the tactical advantages of vasoconstriction and topical anesthesia. The patient who has unsuccessfully attempted to blow an FB out of his nose may be successful after instillation of an anesthetic vasoconstrictive solution.
If a patient has swallowed a foreign body that was pushed back into the nasopharynx, this is usually harmless, and the patient and parents can be reassured (see Chapter 72). If the object has been aspirated into the tracheobronchial tree, it may produce coughing and wheezing, and bronchoscopy under anesthesia is required for retrieval.
Animate foreign bodies (myiasis) of the nose are common in warm tropical climates and are associated with poor hygiene. The most common of all infestations is the fly maggot. These maggots can cause varying degrees of inflammatory reaction, including local tissue destruction, fetid discharge, and pain. The symptoms tend to be bilateral. Inspection after suctioning may reveal constant motion and masses of different worms. These worms are firmly attached and difficult to extract. An ENT consultation is required.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


