CHAPTER 18
Foreign Body, Corneal
Presentation
The patient’s eye has been struck by a falling or an airborne particle, often a fleck of rust loosened while working under a car. Other possibilities include particles from metal grinding, windblown grit, and wood or masonry from construction sites. The patient will complain of a foreign-body sensation and tearing and, possibly over time, will develop constant pain, redness, and photophobia (posttraumatic iritis). Moderate- to high-velocity foreign bodies (fragments chipped from a chisel when struck by a hammer or spray from a grinding wheel) can be superficially embedded on the corneal surface or lodged deep in the corneal stroma, the anterior chamber, or even the vitreous. Superficial foreign bodies may be visualized by simple sidelighting of the cornea or by slit-lamp examination. Deep foreign bodies may be visible on funduscopy only as moving shadows, with a slight or invisible puncture in the sclera.
What To Do:
 Instill topical anesthetic drops (proparacaine [Ophthaine, Alcaine, Ophthetic] or tetracaine [Pontocaine]). This should relieve discomfort and any uncontrollable blepharospasm.
Instill topical anesthetic drops (proparacaine [Ophthaine, Alcaine, Ophthetic] or tetracaine [Pontocaine]). This should relieve discomfort and any uncontrollable blepharospasm.
 Perform a best-corrected visual acuity examination, funduscopy (looking for shadows), and bright-light anterior-chamber examination (slit lamp is best), and check pupil symmetry and anterior chamber cell/flare (for iritis) and conjunctivae (for loose foreign bodies).
Perform a best-corrected visual acuity examination, funduscopy (looking for shadows), and bright-light anterior-chamber examination (slit lamp is best), and check pupil symmetry and anterior chamber cell/flare (for iritis) and conjunctivae (for loose foreign bodies).
 Under magnification, a superficial corneal foreign body (usually metal or grit, but occasionally paint or plastic) will be seen adherent to the corneal surface. Often it is embedded within the corneal epithelium. With iron particles, there will be a halo of particulate debris and rustlike discoloration within the surrounding epithelial tissue (Figure 18-1).
Under magnification, a superficial corneal foreign body (usually metal or grit, but occasionally paint or plastic) will be seen adherent to the corneal surface. Often it is embedded within the corneal epithelium. With iron particles, there will be a halo of particulate debris and rustlike discoloration within the surrounding epithelial tissue (Figure 18-1).
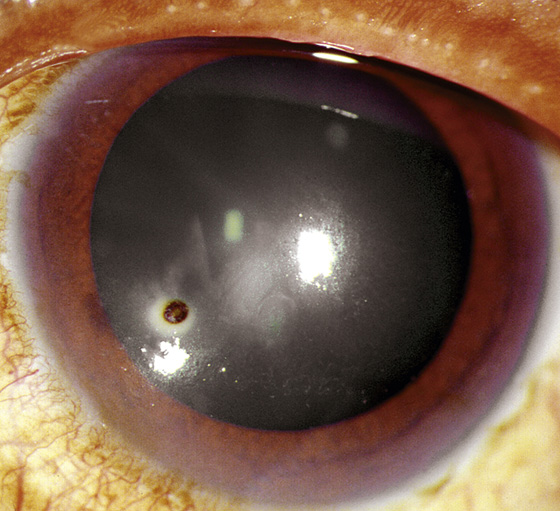
Figure 18-1 Small iron-containing corneal foreign body. (Adapted from Palay DA, Krachmer JH: Primary Care Ophthalmology, ed 2. St Louis, 2005, Mosby.)
 With more serious punctures through the anterior corneal surface penetrating into the anterior chamber, leakage of intraocular fluid from the puncture site might be seen. Streaming of fluorescein dye in this scenario is called the Seidel sign. Such a perforation requires immediate ophthalmologic intervention and application of a protective eye shield.
With more serious punctures through the anterior corneal surface penetrating into the anterior chamber, leakage of intraocular fluid from the puncture site might be seen. Streaming of fluorescein dye in this scenario is called the Seidel sign. Such a perforation requires immediate ophthalmologic intervention and application of a protective eye shield.
 If there is any suspicion of a penetrating intraocular foreign body, because there was a high-velocity mechanism of injury, obtain special orbital radiographs or CT scans to locate it or rule it out. At present, CT scans are considered the gold standard, and have the highest accuracy in diagnosis and localization. The physician should request 3-mm sections through the orbit, unless a foreign body was seen on plain radiography, in which case 6-mm sections are acceptable. Ultrasonography (US) is an increasingly popular modality for detecting intraocular foreign bodies because of its immediate availability for emergency physicians familiar with these techniques. MRI should be used to locate a nonmetallic object. MRI should never be used if a magnetic foreign body is suspected. If an intraocular foreign body is discovered, immediate ophthalmologic consultation and intervention must be obtained. Any intraocular foreign body can lead to infection and endophthalmitis, a serious condition that can lead to loss of the eye.
If there is any suspicion of a penetrating intraocular foreign body, because there was a high-velocity mechanism of injury, obtain special orbital radiographs or CT scans to locate it or rule it out. At present, CT scans are considered the gold standard, and have the highest accuracy in diagnosis and localization. The physician should request 3-mm sections through the orbit, unless a foreign body was seen on plain radiography, in which case 6-mm sections are acceptable. Ultrasonography (US) is an increasingly popular modality for detecting intraocular foreign bodies because of its immediate availability for emergency physicians familiar with these techniques. MRI should be used to locate a nonmetallic object. MRI should never be used if a magnetic foreign body is suspected. If an intraocular foreign body is discovered, immediate ophthalmologic consultation and intervention must be obtained. Any intraocular foreign body can lead to infection and endophthalmitis, a serious condition that can lead to loss of the eye.
 A loosely embedded corneal foreign body might be removed by touching it with a moistened swab, as shown in Chapter 17, but if the object is firmly embedded, it will have to be scraped off (under magnification, preferably with a slit lamp) with an ophthalmic spud or an 18-gauge needle (Figure 18-2). Some emergency physicians recommend using a small needle for scraping, to minimize the possibility of a corneal perforation, but with a tangential approach, the larger needle is less likely to cause harm.
A loosely embedded corneal foreign body might be removed by touching it with a moistened swab, as shown in Chapter 17, but if the object is firmly embedded, it will have to be scraped off (under magnification, preferably with a slit lamp) with an ophthalmic spud or an 18-gauge needle (Figure 18-2). Some emergency physicians recommend using a small needle for scraping, to minimize the possibility of a corneal perforation, but with a tangential approach, the larger needle is less likely to cause harm.
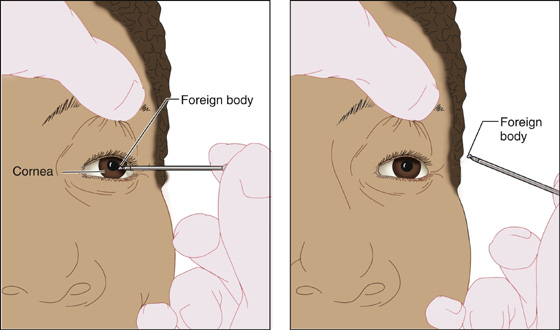
Figure 18-2 Removing a corneal foreign body with an 18-gauge needle.
 Give the patient an object to fixate on so that he will keep his eye still; brace your hand on his forehead or cheek and approach the eye tangentially so that no sudden motion can cause a perforation of the anterior chamber with the needle. Removal of the foreign body leaves a defect that should be treated as a corneal abrasion (see Chapter 16).
Give the patient an object to fixate on so that he will keep his eye still; brace your hand on his forehead or cheek and approach the eye tangentially so that no sudden motion can cause a perforation of the anterior chamber with the needle. Removal of the foreign body leaves a defect that should be treated as a corneal abrasion (see Chapter 16).
 If a rust ring is present, it may appear that a foreign body still remains adherent to the cornea after it has been picked away (Figure 18-3). Use the needle to continue scraping away this rust-impregnated corneal epithelium. A corneal burr, if available, is preferable for this task (Figure 18-4). This mechanical burr should be held in the same tangential manner as the needle, as described earlier. The operator’s hand should also be braced against the side of the patient’s face.
If a rust ring is present, it may appear that a foreign body still remains adherent to the cornea after it has been picked away (Figure 18-3). Use the needle to continue scraping away this rust-impregnated corneal epithelium. A corneal burr, if available, is preferable for this task (Figure 18-4). This mechanical burr should be held in the same tangential manner as the needle, as described earlier. The operator’s hand should also be braced against the side of the patient’s face.
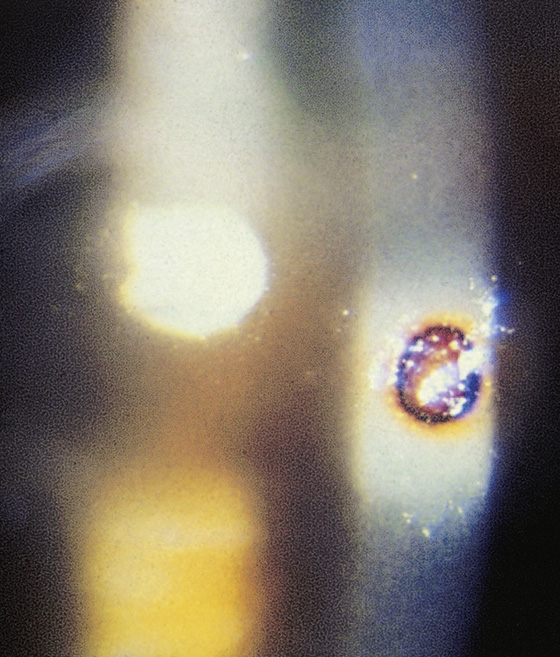
Figure 18-3 Iron-containing corneal foreign body after removal with a residual rust ring. (Adapted from Marx J, Hockberger R, Walls R: Rosen’s Emergency Medicine, vol 6, ed 3. St Louis, 2006, Mosby.)
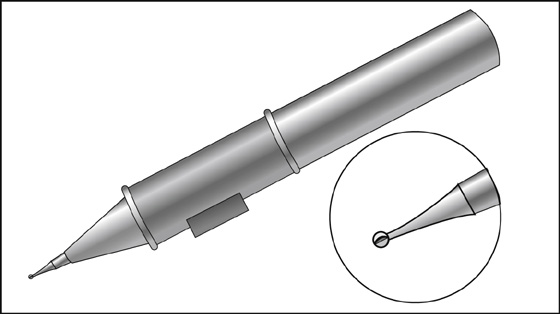
Figure 18-4 Battery-operated corneal burr for rust ring removal.
 If the extent of the corneal defect is unclear, perform an additional fluorescein examination.
If the extent of the corneal defect is unclear, perform an additional fluorescein examination.
 Any large corneal infiltrate or corneal ulcer or significant anterior chamber reaction should be managed as a bacterial keratitis (see Chapter 15).
Any large corneal infiltrate or corneal ulcer or significant anterior chamber reaction should be managed as a bacterial keratitis (see Chapter 15).
 Finish treatment with further irrigation to loosen possible remaining fragments and with instillation of drops of a mydriatic (homatropine 5%) when photophobia and signs of iritis are present (see Chapter 20).
Finish treatment with further irrigation to loosen possible remaining fragments and with instillation of drops of a mydriatic (homatropine 5%) when photophobia and signs of iritis are present (see Chapter 20).
 Instill and prescribe a nonsteroidal anti-inflammatory drug (NSAID) ophthalmologic analgesic drop (diclofenac [Voltaren], 0.1%, 5 mL, or ketorolac [Acular], 0.5%, 5 mL, 1 drop qid).
Instill and prescribe a nonsteroidal anti-inflammatory drug (NSAID) ophthalmologic analgesic drop (diclofenac [Voltaren], 0.1%, 5 mL, or ketorolac [Acular], 0.5%, 5 mL, 1 drop qid).
 Provide for antibiotic eye drops or ointment (polymyxin B/trimethoprim [Polytrim], 10 mL, 1 drop q2-6h while awake, or polymyxin B/bacitracin, 3.5 g, applied inside the lower lid [1- to 2-cm ribbon] qid).
Provide for antibiotic eye drops or ointment (polymyxin B/trimethoprim [Polytrim], 10 mL, 1 drop q2-6h while awake, or polymyxin B/bacitracin, 3.5 g, applied inside the lower lid [1- to 2-cm ribbon] qid).
 Oral analgesic medications should also be provided. The first dose should be given before the patient is discharged from the medical facility.
Oral analgesic medications should also be provided. The first dose should be given before the patient is discharged from the medical facility.
 With deep central corneal foreign bodies, the patient should be advised of the possibility of unavoidable scar formation and subsequent vision impairment. This conversation should be documented.
With deep central corneal foreign bodies, the patient should be advised of the possibility of unavoidable scar formation and subsequent vision impairment. This conversation should be documented.
 Make an appointment for ophthalmologic follow-up in 1 to 2 days to evaluate for complete healing or any residual corneal staining.
Make an appointment for ophthalmologic follow-up in 1 to 2 days to evaluate for complete healing or any residual corneal staining.
What Not To Do:
 Do not use MRI when there is a suspected magnetic intraocular foreign body.
Do not use MRI when there is a suspected magnetic intraocular foreign body.
 Do not overlook a foreign body lodged deep inside the globe; the delayed inflammatory response can lead to blindness or even loss of the eye.
Do not overlook a foreign body lodged deep inside the globe; the delayed inflammatory response can lead to blindness or even loss of the eye.
 Do not leave an iron corneal foreign body in place without arranging for early ophthalmologic follow-up the next day.
Do not leave an iron corneal foreign body in place without arranging for early ophthalmologic follow-up the next day.
 Do not allow a patient to leave without ophthalmologic consultation when there is diffuse or focal corneal opacity, abnormal shape of the pupil, or significant loss of visual acuity.
Do not allow a patient to leave without ophthalmologic consultation when there is diffuse or focal corneal opacity, abnormal shape of the pupil, or significant loss of visual acuity.
 Do not be stingy with pain medication. Large corneal abrasions resulting from foreign-body removal can be quite painful.
Do not be stingy with pain medication. Large corneal abrasions resulting from foreign-body removal can be quite painful.
 If homatropine was instilled, do not forget to tell the patient that he will have blurred near vision and an enlarged pupil for 12 to 24 hours.
If homatropine was instilled, do not forget to tell the patient that he will have blurred near vision and an enlarged pupil for 12 to 24 hours.
Discussion
Superficial corneal foreign bodies are much more common than deeply embedded corneal foreign bodies. Sometimes, the foreign body may not be present at the time of the eye examination. It may have spontaneously dislodged, leaving only the resultant rust ring and/or punctate corneal abrasion with pain and possible photophobia.
Generally, superficial foreign bodies that are removed soon after the injury leave no permanent scarring or visual defect. The deeper the injury, the more the corneal stroma is involved, and the longer the time interval between the injury and treatment, the greater the likelihood of complications. If infection develops, the prognosis will also worsen.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


