Critical Care Medicine
Adult Critical Care
CPAP for acute cardiogenic pulmonary oedema from out-of-hospital to cardiac intensive care unit: a randomised multicentre study
Ducros L, on behalf of the CPAP collaborative study group (Hôpital Universitaire Lariboisiére, Paris, France; et al) Intensive Care Med 37:1501-1509, 2011§
Evidence Ranking
• A
Expert Rating
• 3
Abstract
Conclusion
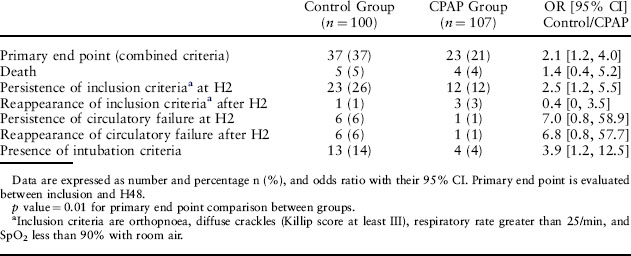
Immediate use of CPAP in out-of-hospital treatment of CPE and until CPE resolves after admission significantly improves early outcome compared with medical treatment alone (Tables 2–4).
Table 2 Physiological Parameters at Study Entry and Echocardiographic Findings
| Parameters | Control Group (N = 100) | CPAP Group (N = 107) |
|---|---|---|
| SpO2 in air (%) | 84 [78, 88] | 84 [80, 88] |
| pH | 7.30 [7.22, 7.36] | 7.30 [7.25, 7.37] |
| PO2 (mmHg) | 127 [86, 177] | 114 [79, 183] |
| PCO2 (mmHg) | 49 [41, 57] | 46 [39, 55] |
| Bicarbonates (mmol/L) | 23 [20, 26] | 24 [20, 26] |
| Respiratory rate (per min) | 35 [30, 40] | 36 [30, 40] |
| Systolic arterial blood pressure (mmHg) | 170 [143, 193] | 170 [150, 195] |
| Diastolic arterial blood pressure (mmHg) | 97 [80, 103] | 95 [82, 110] |
| Heart rate (bpm) | 101 [90, 116] | 102 [83, 116] |
| Encephalopathy | 7 (7) | 13 (12) |
| Circulatory failure | 18 (18) | 17 (16) |
| Echocardiographic findings LVEF | 35 [30, 60] | 45 [35, 60] |
| Syst. PAP (mmHg) | 40 [32, 45] | 38 [31, 43] |
| E/A ratio | 0.9 [1, 1] | 0.9 [1, 2] |
Data are expressed as median with 25th and 75th interquartile range [Q1, Q3] or number and percentage n (%); SpO2 pulse oximetry; arterial blood gases were sampled under O2 mask with a reservoir at 15 L/min. LVEF left ventricular ejection fraction, Syst PAP systolic pulmonary arterial pressure (mmHg); E/A ratio flow velocity ratio across the mitral valve between early diastole and atrial contraction.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree