Chapter 68 Flail Chest and Pulmonary Contusion
4 What is a flail chest, and how is it diagnosed?
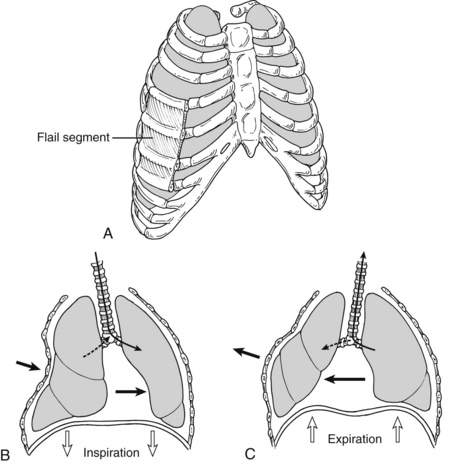
Flail chest is defined as fractures of three or more consecutive ribs or costal cartilages fractured in two or more places (Fig. 68-1). These fractured segments give rise to a free-floating portion of the thorax, which moves paradoxically throughout the respiratory cycle, with inward motion with inspiration and outward motion with exhalation. Although rib fractures may be diagnosed radiographically, flail chest is a clinical diagnosis. Patients often present with chest wall pain, tenderness, bruising, and palpable step-offs of the ribs, but flail chest is distinguished from other chest trauma by noting the paradoxical movement of the chest wall during spontaneous respiration. Patients receiving positive pressure ventilation usually do not demonstrate the classic paradoxical movements. Respiratory dysfunction usually does not arise from the paradoxical chest motion but rather is due to underlying contusions and splinting from pain.
6 What is the role of radiographs in the diagnosis of pulmonary contusion?
Pulmonary contusions are diagnosed radiographically. Although initial chest radiographs may be unremarkable, a nonsegmental infiltrate typically develops over a 6-hour period. If the contusions are visible on the initial chest radiograph, the injury is likely to be more severe, and enlargement of the contused area on the radiograph over the next 24 hours is a poor prognostic sign. Classic radiograph patterns include irregular consolidations or a diffuse patchy pattern (Fig. 68-2). Even after development of chest radiograph findings, plain radiographs may underestimate the severity of the contusions. CT scan is more sensitive for diagnosis of pulmonary contusions and can quantify the volume of lung involved.
8 What is the relationship between pulmonary contusions and acute respiratory distress syndrome (ARDS)?
9 What is the mortality rate and cause of death for patients with flail chest and pulmonary contusions?
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree