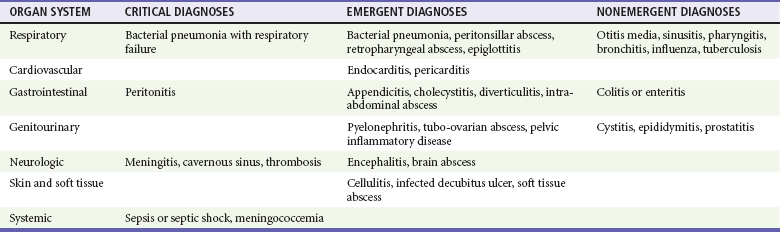
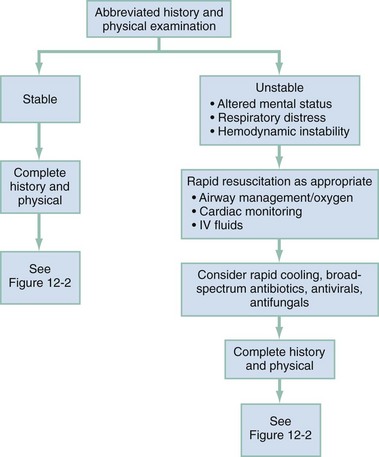
Chapter 12 Fever is a common presenting complaint in both pediatric and adult (aged 18-65 years) emergency department (ED) patients. Patients often confuse fever with a disease process itself, rather than a sign of an illness. Morbidity and mortality rates from febrile illnesses vary dramatically with age. Younger adults with fever usually have benign self-limited disease, with less than 1% mortality. The challenge in this group is to identify the rare meningitis or septic conditions when confronted with a predominance of self-limited viral and focal bacterial diseases. Patients older than 65 years, or those with chronic disease who have fever, represent a group at high risk for serious disease. Morbidity and mortality rates in this group are significant. From 70 to 90% are hospitalized, and 7 to 9% die within 1 month of admission.1 Infection is the most common cause of fever in these patients, and most of these infections are bacterial in nature. Three body systems—the respiratory tract, the urinary tract, and the skin and soft tissue—are the target for more than 80% of these infections.1,2 The relative mortality and morbidity for any given infection are much higher in the geriatric population. For example, elders are at 5 to 10 times greater risk for urinary tract infections and 15 to 20 times for appendicitis.1,3 Even viral illnesses that are generally not fatal, such as influenza, can be highly lethal in elder persons. Moderate elevations of the body temperature may serve to aid the host defense by increasing chemotaxis, decreasing microbial replication, and improving lymphocyte function. Elevated temperatures directly inhibit the growth of certain bacteria and viruses.4 Fever also results in certain increased physiologic costs to the host, including increased oxygen consumption, metabolic demands, protein breakdown, and gluconeogenesis. These costs are particularly problematic in elders, who typically have a smaller margin of reserve for any given body system. It is well established that the ability to develop fever in elders is somewhat impaired. Older individuals also are known to have lower baseline temperatures than younger adults.5 It has not been shown that treatment of fever with antipyretics has a beneficial effect on outcome or prevents complications; however, treatment to reduce the fever makes febrile patients more comfortable.4 The complete differential diagnosis for the patient in the ED with fever is extensive. The major infectious and noninfectious causes are summarized in Table 12-1 and Box 12-1, respectively. The vast majority of serious causes are infectious in origin. Immediate threats to life are from decompensated shock (usually septic), respiratory failure (related to shock or pneumonia), or central nervous system infection (meningitis). Some critical noninfectious causes of fever also exist (see Box 12-1), but these are relatively rare and frequently do not occur with fever as the primary symptom. A primary medical decision in acute febrile illness is based on assessment of patient stability (Fig. 12-1). Patients with life-threatening signs and symptoms, including significant alterations in mental status, respiratory distress, and cardiovascular instability, may require rapid, vigorous treatment. Prompt airway management and initiation of monitoring, intravenous access, fluid resuscitation, supplemental oxygen, and respiratory support are often necessary despite incomplete information concerning the cause of the fever. Sustained temperatures above 41.0° C are rare but can be damaging to neural tissue and require rapid cooling (e.g., misting, fans, cooling blankets).
Fever in the Adult Patient
Perspective
Pathophysiology
Diagnostic Approach
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Fever in the Adult Patient
Only gold members can continue reading. Log In or Register to continue