Fever: Approach to the Febrile Child
Richard Bachur MD
INTRODUCTION
Fever is one of the most frequently encountered pediatric problems, accounting for 25% of visits to pediatric emergency rooms (Krauss, et al., 1991; Nelson, et al., 1992). In children, most febrile illnesses are benign and self-limited. Because fever is a sign of systemic disease, however, the challenge for primary care practitioners is to determine its specific etiology. In most cases, a viral cause is evident, and careful explanation and proper instructions for supportive care and follow-up are all that parents require to care for their children appropriately. Some children with fever, however, have identifiable or suspected causes requiring specific therapy and either hospitalization or close follow-up. Only rarely, with extreme temperatures above 41.1°C (106°F), does a fever pose a danger to the child. This chapter addresses the general approach to the febrile child and the specific conditions that cause fever. Display 31-1 provides conditions associated with fever, common causes of fever, and life-threatening causes of fever.
DISPLAY 31–1 • Conditions Associated With Fever
Infections
Upper respiratory tract
Common cold*
Pharyngitis/tonsillitis*
Cervical adenitis*
Epiglotittis†
Retropharyngeal abscess/cellulitis†
Peritonsillar abscess
Acute sinusitis*
Tracheitis†
Otitis media*
Lower respiratory tract
Acute bronchitis
Lung abscess
Empyema
Oral cavity and salivary glands
Dental abscess*
Herpangina*
Herpetic gingivostomatitis*
Parotitis*
Central nervous system (CNS)
Gastrointestinal
Pancreatitis†
Peritonitis†
Appendicitis*
Cholangitis
Peritonitis
Hepatitis
Intra-abdominal abscess (include retroperitoneal)
Genitourinary
Urinary tract infection*
Renal or perinephric abscess
Pelvic inflammatory disease*
Acute salpingitis*
Tubo-ovarian abscess*
Epididymitis*
Orchitis
Prostatitis
Musculoskeletal
Ocular
Cutaneous
Cellulitis*
Exanthems
Bacterial: erythroderma with toxic shock syndrome,† scarletina with group A streptococcal infection*
Rocky Mountain spotted fever†
Lyme disease*
Secondary syphillis
Systemic Infections
CNS disorders
CNS lesions or malformations of hypothalamus or brainstem
Familial dysautonomia
Status epilepticus†
Neoplasms
Neuroblastoma†
Sarcoma
Vasculitic syndromes
Juvenile rheumatoid arthritis
Systemic lupus erythematosus†
Polyarteritis nodosa
Dermatomyositis
Henoch-Schönlein purpura*
Serum sickness*
Stevens-Johnson syndrome†
Poisonings/drug reactions
Salicylate toxicity†
Atropine poisoning†
Phenothiazines
Antidepressants with anticholinergic side effects
Malignant hyperthermia† associated with inhaled anesthetics and succinylcholine
Miscellaneous conditions
Confined hemorrhage (eg, hematoma with long bone fracture)*
Heat stroke†
Intravascular hemolysis as with blood transfusion reaction†
Dehydration*
Inflammatory bowel disease
Thyrotoxicosis
Crush injuries
Other rare (familial mediterranean fever, ectodermal dysplasia, intermittent porphyria)
Vaccine reactions*
Footnote
Common conditions (*) and potentially life-threatening conditions (†) are noted.
ANATOMY, PHYSIOLOGY, AND PATHOLOGY
The hypothalamus regulates body temperature with a typical diurnal variation—high in the evening and low in the morning. The “normal” range of temperature varies among individuals. A rectal temperature of 100.4°F (38°C) generally is considered fever. Oral temperatures are 1°F (0.6°C) lower than rectal temperatures, and axillary temperatures are 2°F (1.2°C) lower than rectal measurements.
• Clinical Pearl
Although recent investigations have shown that tympanic temperatures may correlate well with rectal or core temperatures, providers should confirm fever by other traditional measures, such as rectal temperature. This is especially true for young infants, when the presence or degree of fever determines management.
Fever develops when exogenous pyrogens (eg, infectious agents, antibody–antigen complexes, and toxins) induce the production of endogenous pyrogen by phagocytic leukocytes. Endogenous pyrogen, traveling through the circulation, acts on the anterior hypothalamus to signal increased heat production (increased metabolism) and decreased heat loss (cutaneous vasoconstriction). Fever appears to be part of the body’s adaptive response to infectious and noninfectious inflammatory challenges. It has been shown to inhibit efficient replication of many microbes and to increase phagocytic activity. Other changes, including decreased glucose production (preferred energy substrate of pathogens) and production of acute phase reactants, also contribute to this adaptive response. Antipyretics prevent production of prostaglandins, which act as signals to the anterior hypothalamus.
The magnitude of fever reduction from antipyretics does not distinguish those with serious infections from those with simple, uncomplicated illnesses.
The organisms responsible for serious infections in infants younger than 2 months include group B Streptococcus, Escherichia coli (and less frequently other enteric gram-negative bacteria), and Listeria monocytogenes. In older infants and children, Streptococcus pneumoniae, Haemophilus influenzae, and Neisseria meningitidis account for most cases. Thankfully, invasive disease due to H. influenzae type b has all but disappeared due to universal vaccination. Rarely, group A Streptococcus, Staphylococcus aureus, and Salmonella species cause bacteremia or sepsis and usually are associated with focal infections.
HISTORY AND PHYSICAL EXAMINATION
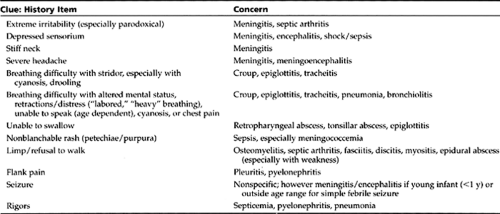
The history and physical examination will provide the most important information in determining the urgency of the situation. Items in the history that suggest “toxicity” or an emergent situation (especially if triaging by phone) are listed in Table 31-1.
• Clinical Pearl
When the patient presents to the office, observation of the child from afar, in the parent’s arms, or on the exam table, may suggest or dismiss concerns of toxicity. The degree of alertness and interaction, response to the parent and examiner, and respiratory status are valuable measures of illness. To the experienced practitioner, this is known as the “look test.”
Because of the predictable “don’t touch me” response of many toddlers and preschoolers, careful observation before attempts at examination may eliminate concerns of meningitis or encephalitis that may be less obvious once the screaming begins.
Providers should ask questions about the onset and duration of the fever, the temperature measurement and how parents obtained it, medications used, associated symptoms and signs, and infectious exposures (eg, family, daycare, school). Past medical history should focus on previous febrile illnesses, immunization status, perinatal course for young infants, and the presence of any immunodeficiency (eg, sickle cell disease, asplenia, hypogammaglobulinemia, malignancy, human immunodeficiency virus [HIV], and steroid use). The clinician should conduct a general review of systems, including feeding history, urinary output, presence of any respiratory symptoms, gastrointestinal symptoms, headache, sore throat, myalgias or arthralgias, and rashes.
During the physical examination, the provider should investigate any signs of severe, life-threatening infections. He or she should obtain a complete set of vital signs in any
ill-appearing child. Stridor, drooling, dysphonia, or leaning forward with the neck hyperextended (“sniffing” position) may be signs of impending upper airway obstruction. Tachypnea, retractions, or cyanosis may suggest severe pneumonia. Altered sensorium, meningismus, or focal neurologic deficits are seen with meningitis and encephalitis. In young infants, a bulging fontanelle may be seen with meningitis, but meningismus is rare before age 1 year. Signs of poor perfusion (eg, tachycardia, altered mental status, weak peripheral pulses, delayed capillary refill, cold or discolored extremities) can be seen with sepsis, pericarditis, myocarditis, endocarditis, as well as with dehydration. Petechial rashes often are seen with streptococccal throat infections and viruses but also may be associated with Rocky Mountain spotted fever and meningococcemia.
ill-appearing child. Stridor, drooling, dysphonia, or leaning forward with the neck hyperextended (“sniffing” position) may be signs of impending upper airway obstruction. Tachypnea, retractions, or cyanosis may suggest severe pneumonia. Altered sensorium, meningismus, or focal neurologic deficits are seen with meningitis and encephalitis. In young infants, a bulging fontanelle may be seen with meningitis, but meningismus is rare before age 1 year. Signs of poor perfusion (eg, tachycardia, altered mental status, weak peripheral pulses, delayed capillary refill, cold or discolored extremities) can be seen with sepsis, pericarditis, myocarditis, endocarditis, as well as with dehydration. Petechial rashes often are seen with streptococccal throat infections and viruses but also may be associated with Rocky Mountain spotted fever and meningococcemia.
In most cases, the provider can focus examination on the common causes of fever in children. Common sites of infection include the eyes, ears, nose, mouth, cervical lymph nodes, chest, abdomen, skin, and skeletal system. Specific viral illnesses, such as gingivostomatitis, herpangina, varicella, bronchiolitis, and mononucleosis, may become evident by examination. Examination of the tympanic membrane, revealing erythema, loss of landmarks, opacification, and decreased mobility, suggests otitis media.
• Clinical Pearl
Providers should not attribute high fever to otitis media alone; most often, a viral illness or other focal bacterial infection coexists with otitis media to produce the high fever.
• Clinical Pearl
Streptococcal pharyngitis is a predominant cause of fever in preschoolers and school-age children; therefore, providers should suspect it in children with pharyngitis (even in the absence of exudate).
Frequently, vomiting, abdominal pain, headache, and tender cervical adenopathy are associated with streptococcal throat infections. Secondary bacterial infections frequently develop following upper respiratory infections (URIs) and include cervical adenitis (often a unilateral, swollen, and tender submandibular node), sinusitis, and otitis media. A characteristic tracheal cough (described as a honking goose or barking seal), hoarseness, and nighttime stridor are typical findings in croup. Respiratory symptoms with lower respiratory tract signs (eg, decreased breath sounds, rales, focal rhonchi, or wheezes) may suggest pneumonia. Abdominal examination is generally innocent with gastroenteritis. Tenderness, especially if focal, can be seen with gastroenteritis, but providers also should consider mesenteric adenitis, appendicitis, and intussusception. Suprapubic pain or flank tenderness implies a urinary tract infection (UTI). Point tenderness over bone or a swollen, warm joint can be found with osteomyelitis or septic arthritis, respectively. With the exception of UTIs and pneumonias in young children, the common bacterial causes of febrile illness usually have localizing signs.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree