FEVER
FRAN BALAMUTH, MD, PhD, MSCE, FRED M. HENRETIG, MD, AND ELIZABETH R. ALPERN, MD, MSCE
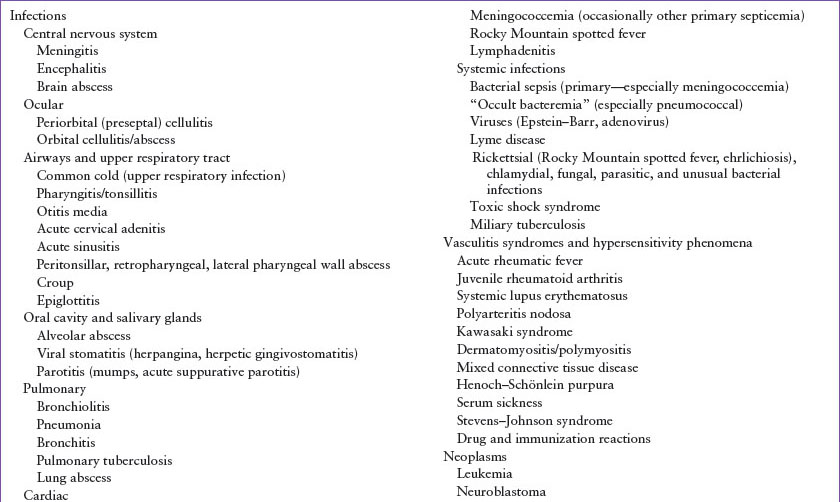
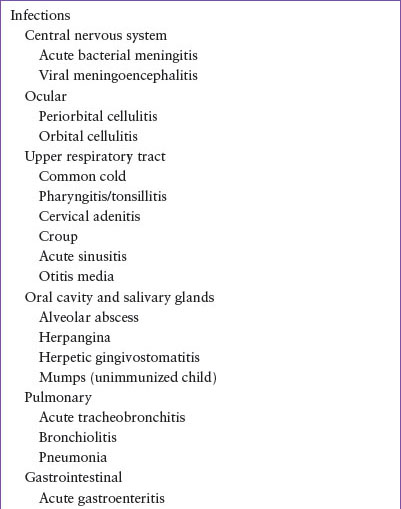
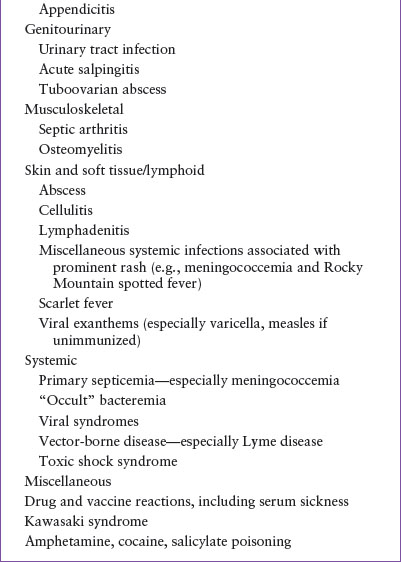
Fever, the abnormal elevation of body temperature, has been recognized for centuries by physicians as a sign of disease. The problem of the febrile child is one of the most commonly encountered in clinical pediatrics, accounting for as many as 20% of pediatric emergency department (ED) visits. The problem of appropriate clinical and laboratory evaluation of febrile children, however, remains a major challenge. The approach outlined in this chapter helps the physician evaluate and treat a febrile child in the ED, proceeding systematically with the appropriate diagnostic steps and management. The principal causes of fever in children are listed in Table 26.1.
PATHOPHYSIOLOGY
Fever is a complex process, involving the highly coordinated interplay of autonomic, neuroendocrine, and behavioral responses to a variety of infectious and noninfectious inflammatory challenges. Fever is believed to be an adaptive response that is ubiquitous in animals. Exogenous pyrogens (e.g., toxins, infectious agents, etc.) from many sources produce fever by inducing the production of endogenous pyrogens (e.g., interleukin-B1, interleukin-6, etc.). These pyrogens interact with specialized receptor neurons of the hypothalamus. This leads to the production of prostaglandins as the critical mediators of the febrile response, resetting the hypothalamic thermostat to elevate body temperature. There is some evidence that increased body temperature impairs replication of microbes and may aid phagocytic bactericidal activity. Additionally, the febrile response includes adaptive neuroendocrine and metabolic effects that further enhance the host’s response to microbial invasion. Rarely, fever results from central nervous system (CNS) dysfunction (e.g., hypothalamic tumor, infarction) that alters the thermostatic set point directly, rather than via pyrogen induction. Finally, sometimes hyperpyrexia is not due to altered hypothalamic regulation, but rather to increased heat production (e.g., stimulant drug overdose; see Chapter 110 Toxicologic Emergencies) or exposure to excess environmental heat (heat stroke; see Chapter 98 Environmental Emergencies, Radiological Emergencies, Bites and Stings).
It is difficult to pinpoint the lowest temperature elevation considered to be definitely abnormal for all children under all circumstances. Some children normally have rectal temperatures as low as 36.2°C (97.2°F) or as high as 38°C (100.4°F). Children, like adults, also have diurnal variations in temperature, with the peak usually occurring between 5 pm and 7 pm. Factors such as excessive clothing, physical activity, hot weather, and ovulation can raise temperature in the absence of disease. For the appropriately dressed child who has been at rest for 30 minutes, a rectal temperature of 38°C (100.4°F) is defined as fever for this discussion.
Using the proper technique to record temperature is important for maximum accuracy. Rectal thermometry combines attributes of being the least invasive way to most approximate core temperature compared to other invasive methods, such as esophageal or bladder thermometry. Optimal technique for rectal thermometry includes appropriate positioning and restraint in infants (prone, supine, or on the side with hips slightly flexed), depth of insertion (about 2 to 3 cm), and time for equilibration (2 to 3 minutes with glass thermometers or several seconds with electronic digital probes). The thermometer should not be placed directly into a fecal mass because the fecal temperature may not have equilibrated with rapid fluctuations in core temperature and thus may be falsely low as temperature rises rapidly. Other noninvasive methods have varying accuracy and precision with most being shown to overestimate at lower body temperatures and underestimate at higher temperatures. Oral and axillary temperatures are usually about 0.6°C (1°F) and 1.1°C (2°F) lower than rectal temperatures, respectively. More recent attempts to measure temperature with less invasive techniques include temperature-sensitive pacifiers and forehead strips, both of which have been found to be unreliable. Infrared tympanic membrane (aural) thermometry, based on the premise that the tympanic membrane shares vascular supply with the hypothalamus, has also shown inadequate accuracy and precision in both afebrile and febrile children and is not useful in healthcare settings. Temporal artery thermometry, which uses similar infrared technology to measure heat produced by the temporal artery, has more recently been studied. The temporal artery technique has been shown to more closely approximate rectal temperatures; however, it has still been found to underestimate high temperatures and overestimate low ones. As even a low-grade fever may be clinically significant in young infants <60 days of age, and as there is at least some doubt about the reliability of axillary, tympanic, or temporal artery measurements in this age group, rectal temperatures should be obtained in this population.
EVALUATION AND DECISION
The importance of fever lies in its role as a sign of disease. The physicians caring for a febrile child should concentrate on discovering the cause of the fever and treating the underlying illness. Although any degree of fever may indicate an important infectious etiology, the risk of serious bacterial infection is slightly higher with hyperpyrexia (defined as a temperature of 41.1°C) in children and a thorough assessment for possible bacterial etiology (e.g., pneumonia, bacteremia, or meningitis) should be seriously considered. However, the magnitude of reduction of fever in response to antipyretics does not distinguish children with serious bacterial illnesses from those with viral diseases. If no specific treatment for the determined diagnosis is necessary, the physician’s goal is then to provide appropriate supportive care and follow-up. Because many parents have “fever phobia,” instructions that explain the importance of fever as an indicator of disease, not as an inherently harmful entity, should be given.
TABLE 26.1
PRINCIPAL CONDITIONS IN CHILDREN ASSOCIATED WITH FEVER
A complete history and physical examination will provide the most important clues in determining the diagnosis of children with febrile illnesses. The age of the infant or child should be carefully considered as it significantly impacts the risk of fever source and etiology. Very young infants’ rate of serious bacterial illnesses is higher than other age groups and children under 24 months have distinct risks of certain infectious causes of fever (see Chapter 102 Infectious Disease Emergencies). The general impression obtained in the first few moments of an evaluation is extremely important in the recognition of potentially life-threatening causes of fever (Table 26.2). A great deal of information can be attained by visual assessment of the child while in the arms or lap of the parent. The severity of the illness may become apparent if the child is agitated or uninterested in the surroundings while in this comfortable, safe position. If the child appears nontoxic, observation of the child while the history of the present illness and medical history is being discussed may provide further insight into the diagnosis. Specifics of fever have different management implications for distinct subsets of children. Therefore, a clear understanding of the degree, mode of measurement, and duration of fever is especially important in the initial evaluation. The physician should ask questions concerning associated signs and symptoms, medications being given (including antipyretics and antibiotics), presence of ill contacts, travel history, and pet or insect exposures. The medical history should focus on recurrent febrile illnesses and the presence of any diseases or drug regimens that would compromise normal host defenses, such as sickle cell anemia, asplenia (functional, congenital, or surgical), malignancy (noting particularly chemotherapeutic or radiation treatments), human immunodeficiency virus (HIV), renal disease, prolonged steroid use, or indwelling catheters or ventriculoperitoneal shunts. Personal immunization status as well as known exposure to unimmunized individuals should also be determined. An understanding of prior evaluation and treatments during this illness may be helpful.
As stated above, the physical examination of the young febrile patient begins during the interview with the caregiver. The physician should note the child’s alertness, responsiveness to persons and objects, work of breathing, color, feeding activity, and age-related appropriateness of social interaction and gross motor functions. The febrile infant who appears irritable and/or lethargic while being held by a parent before the examination has the possibility of having a serious infection such as meningitis or sepsis. The complaint or observation that a child’s crying increases with parental attempts to comfort is critical because “paradoxical irritability” is an important sign of meningitis in infancy.
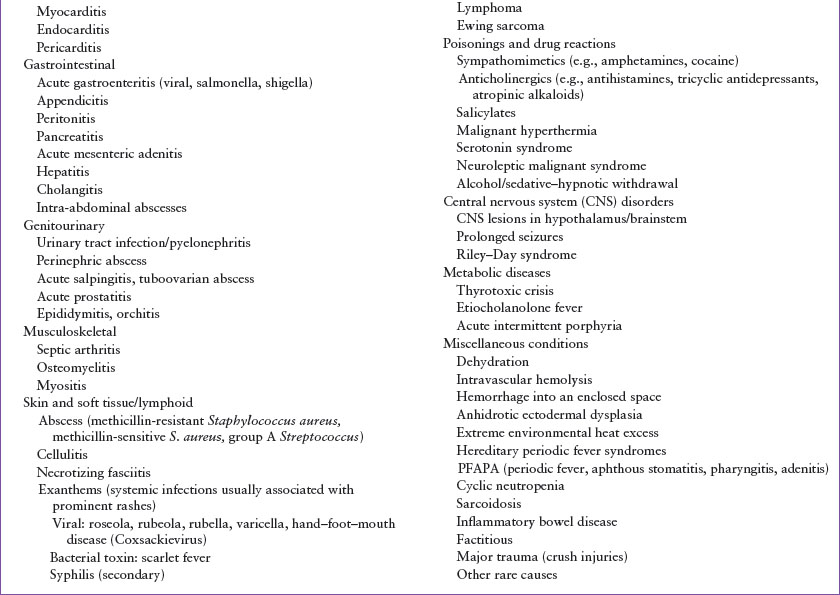
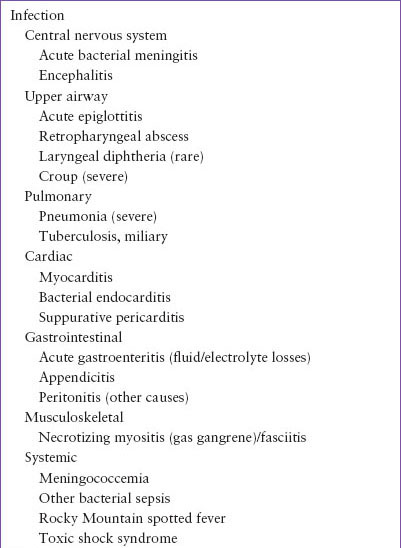
Other signs of severe or life-threatening infections heralded by fever should be sought early in the examination. CNS infections may be marked by fever with altered sensorium, convulsion, meningismus, or focal neurologic deficits. However, infants younger than 2 months of age with meningitis may not have meningismus. They may instead have irritability, somnolence, a bulging fontanel, or nonspecific symptoms such as anorexia, lethargy, or vomiting. Severe upper airway infections may present with stridor, excessive drooling, and tripod positioning. A child with pneumonia, pericarditis, endocarditis, or sepsis syndrome may display tachycardia, dyspnea or tachypnea, cyanosis or pallor, poor perfusion or hypotension, as well as altered mental status. Hemorrhagic rashes may signal bacterial or rickettsial infections such as meningococcemia or Rocky Mountain spotted fever.
TABLE 26.2
LIFE-THREATENING ACUTE FEBRILE ILLNESSES
Careful assessment of the vital signs can provide early important clues to more severe illnesses. Severe sepsis and septic shock are defined as infection with organ dysfunction (see Chapter 5 Shock). It is important to note, however, that hypotension is a late finding in children, and that prompt recognition of the child with compensated septic shock is critical in the ED. That said, recognition of compensated shock can be quite challenging in children, as the prevalence of systemic inflammatory response syndrome (SIRS) defined by fever, tachycardia, and tachypnea is high in pediatric patients, the majority of whom are not critically ill. However, close observation of children with fever and tachycardia is warranted. If the tachycardia resolves with antipyretics and/or oral hydration, and the child is well appearing with normal perfusion and mental status, the child should undergo an evaluation based on the algorithms presented in Clinical Pathway Chapters 87 Fever in Infants and 88 Fever in Children. If tachycardia persists, the child is ill appearing, has a high-risk condition, poor perfusion, or altered mental status, more aggressive treatment for sepsis may be indicated including rapid fluid resuscitation and antimicrobial therapy.
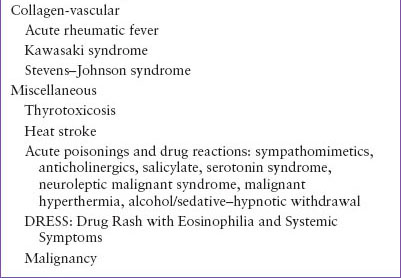
Although the index of suspicion for serious febrile illness must be high throughout the evaluation of each child, most childhood illnesses with fever are minor and self-limiting. Once the physician has ascertained that the child is not in immediate danger, the examination should focus on sites of common pediatric infections, including the ears, nose, and throat; cervical lymph nodes; respiratory, gastrointestinal, and genitourinary tracts; and skin, joints, and skeletal system (Table 26.3). Evaluation of each child is developed with an understanding of the common infectious entities that affect that child’s age group and the presenting signs and symptoms or lack thereof in each infectious entity (see Chapter 102 Infectious Disease Emergencies).
Some febrile exanthems are characteristic enough to be diagnostic (see Chapter 65 Rash: Papulosquamous Eruptions). Varicella, rubeola, scarlet fever, and coxsackievirus can all be identified by their pathognomonic rashes. However, if a child with chickenpox presents several days into the illness with a new fever, the possibility of group A β-hemolytic streptococcal or Staphylococcus aureus superinfection should be considered. Children with fever and petechiae may have invasive meningococcal disease, disseminated streptococcal infection, or Rocky Mountain spotted fever; however, they may simply have a less serious viral infection or streptococcal pharyngitis. Differentiation of these entities is crucial and is based on clinical appearance of the patient and laboratory evaluation. A child with only a few petechiae (especially if only above the nipple line), normal white blood cell (WBC) count, normal platelet count, and well appearance is less likely to have invasive disease. However, any child who appears ill, has distinctly abnormal laboratory results, or has a rapidly progressive petechial rash needs a more complete evaluation for sepsis or meningitis and should receive empiric antibiotics. A patient with fever and diffuse erythroderma should be evaluated carefully for hemodynamic instability or other signs and symptoms of toxic shock syndrome. Fever associated in a young child with severe skin blistering and exfoliation may be toxin-mediated staphylococcal scalded skin syndrome.
On physical examination, acute otitis media is identified by the acute onset of otalgia or fever with changes in the tympanic membranes, such as redness, bulging, decreased mobility, loss of landmarks and light reflex, air–fluid level behind the tympanic membrane, or purulent drainage from a perforation. Careful examination of the head and neck may reveal rhinorrhea and signs of inflammation, suggesting a viral upper respiratory infection (URI). The oropharynx may reveal pharyngitis or stomatitis (see Chapters 47 Oral Lesions and 69 Sore Throat). Children with a history of a recent respiratory infection may have reactive, tender, swollen cervical lymph nodes; asymmetric enlargement of nodes especially with tenderness and overlying erythema might indicate bacterial lymphadenitis. Croup is readily identified by a barky cough with or without stridor in young children, whereas a distinctive “hot potato voice” with unilateral tonsillar swelling in adolescents indicates a peritonsillar abscess. Wheezing, tachypnea, and fever in infants younger than 2 years of age usually mark bronchiolitis. Pneumonia often presents with cough, fever, tachypnea, auscultatory findings, and hypoxemia. Mild abdominal pain or tenderness, vomiting, and/or diarrhea most often suggests viral gastroenteritis but early hepatitis, appendicitis, or pancreatitis should also be considered. More severe findings, particularly the occurrence of peritoneal signs, may indicate appendicitis, intra-abdominal abscess, or peritonitis from other causes (see Chapters 48 Pain: Abdomen, clinical pathway, 82 Abdominal Pain in Postpubertal Girls, 83 Appendicitis (Suspected), and 124 Abdominal Emergencies). However, in children, fever with abdominal pain may also represent lower lobe pneumonia, streptococcal pharyngitis, urinary tract infection (UTI), gastroenteritis, or mesenteric adenitis. Additional findings in UTI may include suprapubic or costovertebral angle tenderness (see clinical pathway Chapter 92 UTI, Febrile). Adolescent girls with pelvic or abdominal pain and fever should be evaluated for pyelonephritis and pelvic inflammatory disease (see clinical pathway Chapter 82 Abdominal Pain in Postpubertal Girls). A close skin examination may reveal an abscess or cellulitis associated with community-acquired methicillin-resistant S. aureus or Streptococcus pyogenes. Differentiation of these diverse diagnoses depends on a thorough history, physical examination, and at times, well-directed laboratory evaluation.
TABLE 26.3
COMMON CAUSES OF FEVER
Continued advancements in immunizations have changed the frequency and risk of certain febrile illness in children. The Centers for Disease Control and Prevention reported that the Haemophilus influenzae type B (Hib) vaccine has drastically changed the risk and causative agents for meningitis in children with a 94% reduction in the incidence of H. influenzae meningitis and a shift in the median age of those affected from 15 months to 25 years of age. The current rarity of epiglottitis in children is also due to this decline in H. influenzae
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







