EYE: VISUAL DISTURBANCES
KAREN E. DULL, MD
Sudden loss or deterioration of vision (or diplopia) can be caused by numerous diseases and injuries (Tables 25.1–25.3). A systematic approach is necessary to reach a correct diagnosis and to minimize the risk of permanent visual impairment. The patient’s age, underlying disease conditions, visual history, and history of possible injury must be determined. The extent of the visual impairment, the rapidity of its onset, and the association with other systemic findings are vital pieces of information. It is important to remember that visual acuity improves with age in children. The normal visual acuity for a toddler is 20/40 and gradually improves to the normal adult acuity of 20/20 by age 5 or 6 years. A careful eye examination, including gross and ophthalmoscopic examination, determination of extraocular movement, and visual acuity, together with the history, leads to correct diagnosis and management of the patient.
Few ocular conditions in the pediatric population are truly emergent (Table 25.4), but many are urgent; most can be treated by the emergency physician or can be referred for appropriate follow-up with an ophthalmologist. Many conditions seen by a pediatric ophthalmologist are not discussed here because they rarely are seen in the emergency department (ED). Conditions that are more likely to be seen in the ED are emphasized in this chapter.
PATHOPHYSIOLOGY
Vision may be impaired through interference at any point in the visual pathway. Light must reach the eye, pass through the cornea and the anterior chamber, be focused by the lens, pass through the posterior chamber, and reach the retina. The retina must react to the visual stimuli, generate electrical impulses, and transmit these impulses along the optic nerve and eventually to the visual cortex for interpretation. In addition, for binocular vision, the movement of both eyes must be coordinated and smooth. Loss of clarity of the visual media or damage to the conductive tissues anywhere along the visual pathway can lead to decreased vision.
DIFFERENTIAL DIAGNOSIS
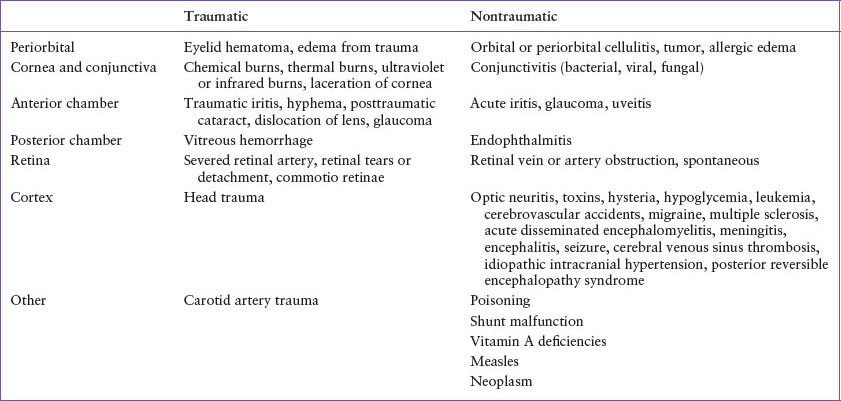
Trauma and infections are the two most common causes of acute visual impairment that can interfere with any part of the visual pathway (Tables 25.1 and 25.2). The total spectrum of diseases that cause visual impairment can be understood best if the visual pathway is divided into its parts, and each part is considered sequentially (Table 25.1).
Vision may be limited by periorbital diseases such as periorbital cellulitis, tumor, infection, or allergic swelling of the eyelids. Orbital cellulitis should be considered if decreased visual acuity, proptosis, ophthalmoplegia, or pain with eye movements is present.
Blunt trauma to the eye may cause a blowout fracture of the orbit. The weakest portion of the orbit, the floor, most commonly breaks, and this may entrap the extraocular muscles. Visual impairment may be limited to double vision when looking in a certain direction, particularly upward. Testing the extraocular movements reveals the limitation. Careful inspection of the globe is also necessary.
Diseases of the cornea that cause visual impairment are predominantly infectious or traumatic. Infections of the cornea and conjunctiva can be caused by bacteria, viruses, and fungi (see Chapters 22 Eye: Red Eye and 131 Ophthalmic Emergencies). All these diseases may present as a unilateral or bilateral process, usually affecting only the conjunctiva and cornea. Onset is variable but usually occurs over 1 or 2 days, and vision is not greatly impaired. In the newborn period, gonococcal, chlamydial, and herpetic infections must be considered. Staphylococcus species are the leading cause of bacterial keratitis. Pseudomonas species is the most commonly isolated bacteria in patients who wear contact lenses. In the United States, the most common corneal infection that causes permanent visual impairment is herpes simplex keratoconjunctivitis, whereas trachoma infection is the most common cause worldwide. A careful ophthalmoscopic or slit lamp examination will reveal the characteristic dendritic ulcers of herpes simplex infection after the eye has been stained with fluorescein. Unless this disease is excluded, steroid-containing medications should not be used. With a recent eye injury or foreign-body intrusion, fungal infections are possible.
There are various types of traumatic injuries to the cornea. Injury secondary to alkali burns constitute one of the true ophthalmologic emergencies. Alkali burns in general carry a worse prognosis than acid burns. Immediate copious irrigation of the eye with normal saline is imperative to prevent permanent visual impairment and to preserve visual acuity. Both ultraviolet and infrared light can cause damage to the cornea, resulting in severe pain and photophobia within 24 hours of exposure. Lacerations with perforation of the cornea usually affect other parts of the eye as well and can lead to significant visual impairment. Careful inspection of the globe with associated lid trauma is mandatory.
The anterior chamber of the eye consists of the aqueous humor, the iris, and the lens. Acute iritis is rare in children, and the cause is often uncertain. There is a sudden onset of pain, redness, and photophobia that usually affects one eye only. The degree of visual impairment varies with the severity of inflammation. Certain diseases, such as juvenile idiopathic arthritis, have associated iritis. Blunt trauma can also cause iritis, but vision is only slightly impaired unless other structures are involved. Traumatic iritis often presents 24 to 72 hours after the trauma.
Trauma can also cause a hyphema or hemorrhage into the anterior chamber. This can result in little to severe visual impairment in the affected eye, depending on the extent of bleeding and associated trauma. Complications of hyphema include rebleeding, which typically occurs within the first 5 days after injury, and increased intraocular pressure potentially leading to glaucoma. Previously, all patients with hyphema were hospitalized on strict bed rest. However, this was not shown to improve outcome, but close follow-up with an ophthalmologist is recommended. Despite lack of definitive evidence, most ophthalmologists recommend cycloplegic and corticosteroid drops to reduce pain and possibly reduce inflammatory complications. Nonsteroidal anti-inflammatory drugs (NSAIDs) should be avoided. The risk of vision loss is highest in patients with sickle cell disease or trait, when greater than 20% of the visual field is affected, with rebleeding, and when residual blood lasts beyond 3 to 4 days duration.
TABLE 25.1
CAUSES OF ACUTE VISUAL DISTURBANCES
Traumatic injuries can lead to cataract formation, usually within a few days of injury, but onset may be delayed for years. Dislocation of the lens after trauma causes significant visual impairment but can be recognized easily with a careful examination. Glaucoma and retinal detachment may be late complications of blunt trauma. Pain around the eye, blurred vision, and occasionally, nausea and vomiting in a patient with glaucoma or with a recent eye injury may represent an acute attack of glaucoma. If any one of these is noted as a primary complaint or an incidental finding, immediate referral is required.
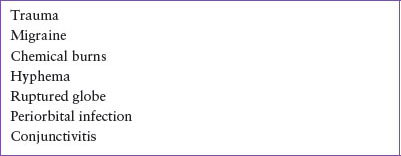
TABLE 25.2
COMMON CONDITIONS THAT CAUSE ACUTE VISUAL DISTURBANCES
The uvea consists of the iris, ciliary body, and choroid. One or all portions of the uvea may become inflamed, causing uveitis. Iritis and iridocyclitis may be called anterior uveitis, whereas inflammation of the choroid is often called posterior uveitis. The etiologies may be divided into infectious and noninfectious. Infectious uveitis may be caused by viruses, bacteria, fungi, or helminths. The most common cause of posterior uveitis in children is toxoplasmosis. Noninfectious causes include juvenile idiopathic arthritis, trauma, ankylosing spondylitis, Behçet disease, idiopathic intracranial hypertension (IIH, pseudotumor cerebri), peripheral uveitis, sarcoidosis, and sympathetic ophthalmia. Vogt–Koyanagi–Harada syndrome is a panuveitis with meningeal and cutaneous findings. Prompt treatment of this syndrome is necessary for optimal visual outcome.
TABLE 25.3
CAUSES OF ACUTE DIPLOPIA
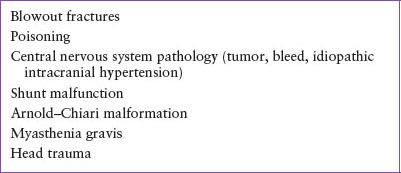
TABLE 25.4
EMERGENT CONDITIONS THAT CAUSE VISUAL DISTURBANCES

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







