EYE: UNEQUAL PUPILS
ELIZABETH S. JACOBS, MD AND ALEX V. LEVIN, MD, MHSc, FRCSC
Abnormalities of the pupils can be helpful diagnostically when assessing central nervous system, autonomic nervous system, orbital, and ocular problems. Pupillary disorders can be divided into two categories: Disorders in which the size of one or both pupils is abnormal and disorders in which the shape of one or both pupils are abnormal. The pupil can also be malpositioned (corectopia). Congenital or acquired (e.g., after trauma) corectopia generally requires ophthalmology consultation. When the pupils are different in size, the term applied is anisocoria. An abnormally dilated pupil is called mydriasis. Miosis refers to an abnormally constricted pupil. Figure 24.1 represents a flowchart for an approach to anisocoria.
PATHOPHYSIOLOGY
The pupillary dilator muscle receives sympathetic innervation. The pupillary sphincter receives parasympathetic innervation that also supplies the ciliary muscle of the eye that governs focusing (accommodation) of the lens.
The first-order sympathetic neurons extend from the hypothalamus through the midbrain, pons, and medulla into the spinal cord, where they synapse with the second-order neurons just before exiting the cord at roots C8–T2. The cervicothoracic sympathetic trunk then travels over the apex of the lungs to the superior cervical ganglion in the neck, where synapses are made with the third-order neurons. Sympathetic innervation to the face departs from the superior cervical ganglion or at the bifurcation of the common carotid artery. Therefore, complete unilateral anhidrosis in association with unilateral miosis suggests damage to the second-order neurons or superior cervical ganglion. The third-order neurons travel with the internal carotid artery into the cranial vault, where the fibers gain access to the orbit via the nasociliary branch of the first division of the trigeminal nerve. They then travel through the ciliary ganglion in the orbit without synapse. Fibers extend to the iris dilator via the ciliary nerves. Disruption of sympathetic innervation anywhere along its course results in ipsilateral miosis (Horner syndrome) and is often accompanied by mild ptosis, enophthalmos, with or without ipsilateral anhidrosis. The lower lid may be higher than the contralateral side (“upside down ptosis”).
Parasympathetic neurons originate in the Edinger–Westphal nuclei, located on the dorsal aspect of the third cranial nerve nucleus. These neurons travel with the third cranial nerve, exiting the midbrain on its ventral aspect and passing between the posterior cerebral artery and the superior cerebellar arteries at the circle of Willis. The nerve then runs anteriorly and enters the cavernous sinus superiorly and laterally. Just before entering the posterior orbit through the superior orbital fissure, the third cranial nerve splits into a superior and an inferior division. The latter contains the parasympathetic fibers that then pass into the ciliary ganglion, where they synapse. Short ciliary nerves then carry the postsynaptic fibers to the pupillary sphincter muscle and the ciliary muscle (behind the iris). Unilateral mydriasis can be caused by damage to the parasympathetic fibers anywhere along their course. With the exceptions noted next, it is distinctly unusual for the parasympathetic fibers to be damaged without other evidence of third cranial nerve palsy (a deficit in the ability of the eye to adduct, look upward, and/or look downward, and/or ptosis; see Chapter 23 Eye: Strabismus).
Local factors can also cause physical changes in the iris or in the surrounding structures that may result in miosis or mydriasis.
EVALUATION AND DECISION
When testing pupillary size, it is essential that the patient be instructed to look at a distant target that does not involve reading letters or numbers. This prevents the eyes from needing to accommodate. Because the innervation for accommodation is the same as that for the pupillary sphincter, the accommodating patient also has reflex contraction of the pupils, particularly when focusing at near. Focusing on a near object also stimulates convergence of the eyes toward each other. Crying or forced eyelid closure may also induce miosis.
ANISOCORIA
When evaluating the patient with anisocoria, the emergency physician must answer two critical questions: (1) Which pupil is abnormal, the smaller or the larger? and (2) Is this abnormality acute or chronic?
To establish which pupil is abnormal, the relative difference in pupillary size should be noted under conditions of bright and dim illumination. Using the largest diameter circle of the direct ophthalmoscope or a bright penlight, both pupils should be illuminated simultaneously in a room with the lights on. The room lights should then be turned off and the handheld light source held tangentially from below or from above so the eyes are illuminated only enough that the examiner can note the pupillary size.
Normally, the pupils constrict equally in response to bright illumination and dilate equally in dim illumination. If the relative difference in pupillary size increases under bright illumination, the larger pupil is the abnormal pupil: The larger pupil is not constricting normally (Fig. 24.2). If the relative difference in pupillary size increases under dim illumination, the smaller pupil is the abnormal pupil: The smaller pupil is not dilating normally. If the relative difference in pupillary size is the same in both dim and bright illumination, the patient does not have an abnormal pupil (Fig. 24.3). Rather, the patient has physiologic anisocoria. Approximately 20% of people with normal pupils have a difference in the size of their pupils in excess of 0.4 mm.
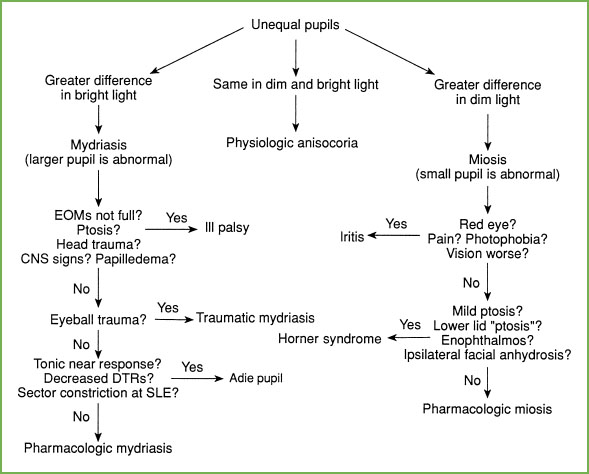
FIGURE 24.1 Unequal pupils. EOM, extraocular muscle movement; CNS, central nervous system; III, third cranial nerve; DTR, deep tendon reflex; SLE, slit lamp examination.
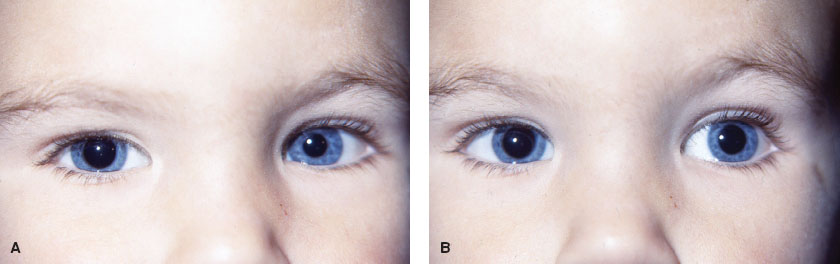
FIGURE 24.2 Patient with right mydriasis. Relative difference between the pupil size is greater in bright illumination (A) than in dim illumination (B).
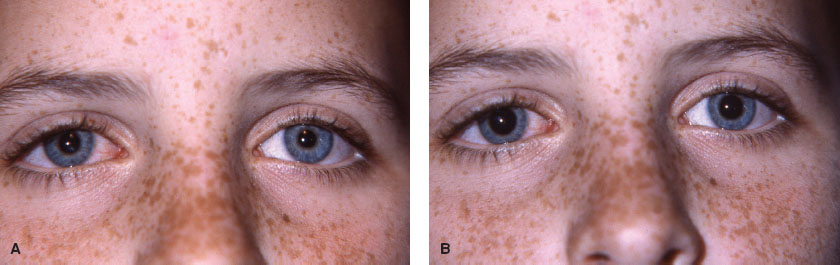
FIGURE 24.3 Physiologic anisocoria. Relative difference in pupil size is the same in bright illumination (A) and dim illumination (B).
TABLE 24.1
DIFFERENTIAL DIAGNOSIS OF UNEQUAL PUPILSa
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







