Eye Problems
Michele McLeod MD
INTRODUCTION
Children with acute ocular problems frequently present with irritated eyes and nonspecific symptoms. The eye’s anatomic considerations and the limited resources available to respond to ocular insult account for the sometimes frustratingly similar appearances of disparate entities. Therefore, the clinician must take a good history, elicit appropriate signs and symptoms, and form a reasonable differential diagnosis to separate minor eye problems from serious ocular processes that may lead to permanent visual disability. This chapter is intended to guide the reader toward the clinical signs and symptoms that, along with a careful history and physical examination, differentiate the two. When in doubt, providers immediately should refer patients to specialists. Reference to texts on pediatric ophthalmology for further detailed information is encouraged (Nelson, 1998; Taylor, 1997; Wright, 1995).
ANATOMY, PHYSIOLOGY, AND PATHOLOGY
Despite its relatively small size, the eye is one of the most complex organs of the human body. It is derived from neural crest cells, neuroectoderm, surface ectoderm, and mesoderm. The white tissue of the eye, the sclera, is a rigid connective tissue that encloses intraocular contents except at the anterior and posterior poles, where it meets the cornea and optic nerve respectively.
Conjunctiva, a diaphanous tissue that lines the inner aspect of the eyelids (tarsal conjunctiva) and reflects in the fornices to cover the sclera (bulbar conjunctiva), consists of an outer epithelial layer and underlying loose connective tissue. As a result of its rich vascularization, the conjunctiva can demonstrate dramatic injection and edema (chemosis) in response to irritation, allergies, or infection. Goblet cells within the conjunctiva secrete the mucous component of the tear film.
The cornea (more specifically, the air-tear film interface) is responsible for approximately two thirds of the eye’s refractive power. Although like the sclera, the cornea is composed primarily of connective tissue (with outer epithelial and inner endothelial layers), it is transparent. This transparency is attributable to the unique characteristic arrangement of type I collagen fibrils in a regular array held in place by a proteoglycan ground substance. When damaged, corneal stroma undergoes further deposition of type I collagen; however, this secondary process occurs without fibrillar organization, and opacification (scarring) of corneal stroma occurs. When the cornea is not clear, this indicates that a pathologic event has occurred or is occurring.
Extraocular muscles attach to the globe underneath the conjunctiva and act as pulleys to effect ocular rotations. Each extraocular muscle is yoked with a muscle in the other eye, causing complementary binocular function. Strabismus (referred to in older literature as “squint” because of the tendency of individuals with strabismus to close one eye to suppress double vision) occurs when the two eyes no longer are acting in conjunction.
The eyelids and structures contained within it are derived primarily from surface ectoderm. A simplified schematic approach to eyelid anatomy would divide the eyelid into two segments (anterior/external and posterior/internal) separated by a thin fibrous structure, the orbital septum. The anatomic segments external to the septum consist of skin, loose subcutaneous connective tissue in which eyelash follicles originate, and orbicularis oculi muscle. Internal to the septum lie the levator muscle, tarsus, Müller’s muscle, and tarsal conjunctiva. The lax connective tissue of the eyelid creates the potential for impressive eyelid swelling in response to infection, inflammation, trauma, allergy, and so forth. The orbital septum is noteworthy because it divides superficial processes that involve primarily skin from deeper processes that involve the orbit, with potential for damage to the globe and spread through orbital fissures to the intracranial space.
Both segments of the eyelid contain sebaceous glands that contribute to the lipid component of the trilayered tear film. Zeis’ glands are associated with cilia (eyelashes), and meibomian glands located within tarsus excrete secretions through orifices in the inner eyelid margin.
The nasolacrimal system consists of inflow and outflow components. The lacrimal gland, a bilobed exocrine gland located under the temporal upper eyelid, produces aqueous secretions in response to reflex and psychogenic stimuli. Basal aqueous secretions are produced by the eccrine glands of Wolfring and Krause located adjacent to tarsus in the eyelids.
The nasolacrimal outflow tract originates at the inferior and superior puncta of the nasal aspect of the eyelids. They open into the superior and inferior canaliculi, which join to form a common canaliculus that opens into the lacrimal sac. The nasolacrimal duct exits the sac inferiorly and ends at the inferior meatus under the inferior turbinate within the nose. Tears (and topical medications) are eliminated through this canalicular and duct system. Richly vascularized nasal mucosa provides the route for systemic absorption (and possible systemic toxicity) of topical medications.
HISTORY AND PHYSICAL EXAMINATION
Primary care providers conduct pediatric eye examinations under two circumstances: during well child examinations and for episodic complaints. Primary care providers can glean information from a well child examination that point to the need for further evaluation, such as amblyopia, strabismus, and ocular pathology (ie, congenital cataracts or glaucoma).
An age-appropriate visual acuity is the essential first step in any eye examination (exception: chemical injury). Visual acuity should be checked separately for each eye. Objection to occlusion of one eye, but not the other, strongly suggests poor vision in the eye the child does not object to being covered. Children should be encouraged to read the chart despite faltering. Children with an amblyopic eye will frequently use the “occluded” contralateral eye by peeking through fingers or through extreme head positions to please the examiner. Children should be carefully monitored while reading the eye chart, because this is an excellent opportunity to pick up amblyopia.
Appropriate visual acuity varies with age. Infants up to 6 to 8 weeks of age typically avoid light. From the age of approximately 2 months, children should be able to fix and follow targets. Older children should demonstrate steady, central fixation on a target and maintain fixation with that eye when the other eye is uncovered (regardless of whether the occluded eye is straight or deviated). Some 2-year-old children may be able to read a picture chart, but by the age of 3 or 4 a child should be able to distinguish familiar pictures on the chart. Visual acuity of 20/30 is appropriate at this age. Asymmetric visual acuity or obvious disparity in ease while reading the chart is a clue to refractive error and possible amblyopia.
A penlight should be used to examine the eyelids, conjunctiva/sclera, cornea, anterior chamber, and iris. The eyes should appear symmetric; asymmetry suggests pathology. A penlight should also be used to assess the pupils both for afferent pupillary defect and similar size. The red reflex should be assessed in infants; in toddlers, the optic nerve and macula should be inspected with the direct ophthalmoscope. A white reflex is always pathologic and is associated with intraocular pathology (retinoblastoma, cataract, persistent hyperplastic primary vitreous, Coats’ disease, etc.). Asymmetric retinal reflex may be caused by strabismus or by intraocular pathology.
Extraocular movements (horizontal and vertical) should be full and nonpainful.
The Bruckner (retinal light reflex) and Hirschberg’s (corneal light reflex) tests may be used to screen for strabismus. Using a direct ophthalmoscope, the examiner can stand about a foot from the child and assess the red (retinal) reflex. If one red reflex is brighter than the other, either the eye with brighter reflex is deviating or intraocular pathology is present. A penlight directed at the child’s eyes from a similar distance should reveal a spot of light in the pupillary space (corneal reflex) displaced slightly temporally (because the child is accommodating and converging) and appearing symmetric in placement. Asymmetric corneal reflexes suggest that one eye is deviating. These tests and observation of the child usually are adequate to evaluate for alignment. However, strabismus may be intermittent or subtle and may be uncovered during a more comprehensive ophthalmologic examination under cycloplegia and using cover testing.
• Clinical Pearl
Parents are excellent observers. When they report strabismus, it would be prudent to refer the child to an ophthalmologist even if a child appears orthophoric by the testing described above.
When a child presents with a specific complaint (infection, injury), a more focused examination should be carried out, but the importance of always obtaining a visual acuity, carefully assessing the anterior segment and posterior pole, checking for full extraocular movements, and ruling out an acute strabismus cannot be stressed enough. These are the minimum components of an examination when pathology is suspected, and further components of the examination depending on presentation are addressed below.
MANAGEMENT
As a general rule, management of ocular complaints related by a parent through a phone conversation may be difficult because parents often have difficulty with a precise description of the eye’s appearance. If the decision is made to manage an ocular complaint over the phone, the child should be evaluated within a day, unless there is significant improvement. If a child’s ocular problem does not improve after several days of initial management by a primary care practitioner, referral to an ophthalmologist should follow.
Complaints of foreign body sensation, photophobia, or visual acuity impairment should be referred without delay to a pediatric or general ophthalmologist.
BLEPHARITIS
Pathology
Blepharitis is associated with staphylococcal colonization of the eyelids. Poor attention to eyelid hygiene contributes to the problem. Collarettes and accumulation of debris occur around the bases of eyelashes, secondary to inflammation or infection that involves the eyelid margins.
History and Physical Examination
Patients with blepharitis usually present with nonspecific complaints of irritated, itchy eyes; eyelids stuck closed in the morning; and white discharge. An examination shows crusting around eyelashes and injection of eyelid margins, and in chronic blepharitis, poliosis (whitening) or madarosis (loss) of cilia may occur. This usually is bilateral but may be asymmetric.
Blepharitis may be associated with conjunctivitis (blepharoconjunctivitis) or with a staphylococcal hypersensitivity reaction that causes tiny corneal stromal opacities. Blepharitis is often accompanied by meibomianitis, inflammation of meibomian glands, which causes meibomian dysfunction and plugging of meibomian pores along the eyelid margins. This secondarily impairs the basal lubrication of the globe and may contribute to dry eye symptoms.
Diagnostic Criteria
The diagnosis of blepharitis is made based on history of itchy eyes with morning crusting and examination of the eyelid margins. Unlike allergic conjunctivitis, blepharitis is not associated with significant eyelid edema after manipulation, patient history of atopy or asthma, and patient or family history of environmental allergies. Seasonal recurrences are useful in differentiating the two.
Management
Good lid hygiene is essential for treatment of this condition. This consists of mechanical and pharmacologic therapy. Parents should be instructed to apply frequent warm compresses to cleanse the eyelids and to gently run a moist cotton
applicator along eyelid margins to dislodge crusting around eyelashes and plugs on meibomian orifices. Erythromycin or bacitracin ophthalmic ointment can be applied to the eyelid margins twice a day. Blepharitis should improve with this therapy, and children who do not respond should be referred for further management to a pediatric ophthalmologist. Blepharitis is a chronic condition, and once the acute problem has resolved, continued daily use of warm compresses to cleanse the eyelid margins helps prevent flareups.
applicator along eyelid margins to dislodge crusting around eyelashes and plugs on meibomian orifices. Erythromycin or bacitracin ophthalmic ointment can be applied to the eyelid margins twice a day. Blepharitis should improve with this therapy, and children who do not respond should be referred for further management to a pediatric ophthalmologist. Blepharitis is a chronic condition, and once the acute problem has resolved, continued daily use of warm compresses to cleanse the eyelid margins helps prevent flareups.
CHALAZIA AND STYES
Pathology
The term hordeola refers to inflammatory or infectious blockage of pores of sebaceous glands in the eyelids. The term external hordeolum, often called by the lay term “stye,” is a blockage of Zeis glands associated with eyelash follicles. Internal hordeola, or chalazia, occur when the meibomian orifices, which line the inner aspect of the eyelid margins, become occluded. On histopathologic examination, chalazia consist of a lipogranulomatous reaction. Children with blepharitis and meibomianitis are particularly prone to developing chalazia and styes.
History and Physical Examination
The history will depend on chronicity. Typically, parents will either describe an acute discrete eyelid swelling or a nodule that has been present for weeks or months, which may be accompanied by periodic purulent discharge and changes in size. On examination, styes are swollen at the edge of the eyelid, while chalazia are discrete firm nodules adjacent to the eyelid margin. There may be focal “pointing” on the tarsal conjunctival aspect of the lesion. Both styes and chalazia may be inflamed and tender. If chronic, they may be associated with overlying skin changes. Multiple chalazia and styes may occur and can be impressive in size.
Diagnostic Criteria
As described previously, styes and chalazia are characteristic in appearance. They occur at the eyelid margin, and the swelling and inflammation are well demarcated. If these lesions are associated with diffuse or spreading eyelid warmth and inflammation or systemic symptoms, such as fever or malaise, it may indicate progression to a cellulitis (see below).
Management
Conservative therapy, consisting of frequent warm compresses, usually is effective in eradicating chalazia and styes. Recalcitrant chalazia can be treated by an ophthalmologist with incision and drainage. Although this simple office procedure is performed under local anesthesia in adults, most children cannot tolerate the injection of local anesthetic and lid clamping that the procedure requires. Because this procedure risks perforation of the globe in unsedated children, pediatric chalazion incision and drainage necessitates a trip to the operating room under general anesthesia. Therefore, committed conservative therapy by far is the best approach. Some children are predisposed to developing chalazia, and ongoing good lid hygiene should be encouraged. Because the eye itself usually is not involved, eyedrops are not helpful unless the eye is injected. If there is associated blepharitis, one may augment the warm compresses with erythromycin or bacitracin ophthalmic ointment, but parents should understand that the warm compresses, not the medication, will eliminate the hordeola.
Diffuse eyelid erythema, warmth, and tenderness indicate progression to a preseptal cellulitis that will require systemic antibiotics.
CELLULITIS (PRESEPTAL AND ORBITAL)
When cellulitis involves the periocular area, it is critical to distinguish infection limited to superficial skin tissues anterior to the orbital septum (preseptal, also referred to as periorbital, cellulitis) from the far more dangerous infection that involves orbital tissues deep to the septum (orbital cellulitis). The latter not only threatens vision, but also may threaten life.
Pathology
Children with a history of sinusitis, periorbital inflammation, trauma (blunt or penetrating, including insect bites), dacryocystitis, and dental abscess are at increased risk of developing preseptal and orbital cellulitis (Rumelt & Rubin, 1996). In children, the most frequent etiology of preseptal and orbital cellulitis is ethmoid sinusitis, which is radiographically present in 96% of orbital cases and 81% of preseptal cases (Barone & Aiuto, 1997). Eyelid lesions (traumatic or related to extension of localized inflammatory processes [ie, hordeola]) are the second most common cause of preseptal and orbital cellulitis in children, followed by dacryocystitis (infection of the nasolacrimal sac).
The causative organisms involved in cellulitis may be presumptively identified based on the origin of the infection. In the absence of a history of trauma, providers should suspect organisms responsible for sinusitis, such as Streptococcus pneumoniae, nontypable Haemophilus influenzae, and Moraxella catarrhalis and in children with a history of chronic sinusitis, anaerobes and Staphylococcus aureus (Barone & Aiuto, 1997). H. influenzae type B, once among the most common and aggressive organisms to cause both preseptal and orbital cellulitis through bacteremic seeding, has essentially been eliminated as a source of cellulitis as a result of vaccination (Barone & Aiuto, 1997; Donahue & Schwartz, 1998). In preseptal or orbital cellulitis related to skin infections or trauma, S. aureus and Streptococcus pyogenes are the most frequent pathogens.
History and Physical Examination
Parents may give a history of recurrent sinusitis or recent respiratory infection or describe an antecedent lesion related to trauma, insect bite, chalazion, or hordeolum. Frequently, they may not recall any precipitating event.
Children with preseptal cellulitis present with eyelids that are tender, swollen, tense, warm, and red. They may exhibit some degree of malaise and be febrile. The globe itself is quiet and uninvolved with normal pupillary reflex. Extraocular movements are full, and vision (if it can be elicited) is normal.
In orbital cellulitis, the findings of swollen, inflamed, and tender eyelids appear similar to those seen in preseptal cellulitis. In contrast, however, the globe itself is proptotic, injected, and chemotic. Ocular movements typically are both painful and restricted (secondary to inflamed orbital tissues
surrounding the globe); there may be papillitis (unilateral optic nerve swelling), an afferent pupillary defect, or decrease in vision secondary to swollen, infected tissues adjacent to the optic nerve. Children are febrile and appear quite ill.
surrounding the globe); there may be papillitis (unilateral optic nerve swelling), an afferent pupillary defect, or decrease in vision secondary to swollen, infected tissues adjacent to the optic nerve. Children are febrile and appear quite ill.
• Clinical Pearl
Decreased and painful extraocular movements and proptosis are the most clinically apparent differentiating features between orbital and preseptal (periorbital) cellulitis.
Diagnostic Criteria
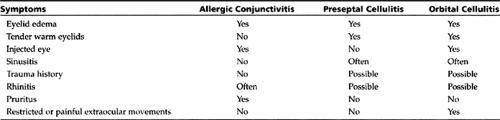
Eyelid swelling in the pediatric population typically is secondary to infection (cellulitis), trauma (with soft-tissue swelling), allergy, or infiltration. History, examination, and focal findings readily diagnose soft-tissue swelling secondary to trauma. While impressive eyelid swelling may occur secondary either to infection or allergy, infected tissues are warm and tender while allergies cause pruritus, often swell rapidly after manipulation, and are cool, nontender, and usually soft to palpation (Table 32-1).
Although infiltrative processes in children are rare, both metastatic neuroblastoma (the most common metastatic orbital tumor in children) and rhabdomyosarcoma (most common primary orbital tumor in children) cause eyelid swelling, ecchymosis, and rapidly progressive proptosis. Both may be mistaken for trauma or cellulitis.
Management
Treatment of Preseptal Cellulitis
Preseptal cellulitis can evolve rapidly into orbital cellulitis, particularly in young children. Thus, the clinician must decide whether to admit a child to the hospital for intravenous antibiotic therapy or treat as an outpatient with oral antibiotics. Among the factors guiding this management decision should be the child’s age. The younger the child, the more prudent it is to admit, and children younger than 2 years should always be admitted. The severity of the infection, reliability of the child’s caregivers in administering medication and noting deterioration, and the surety of close, daily follow-up examinations are important factors in deciding between inpatient versus outpatient management.
Older children with little or no fever, normal complete blood count (CBC), and who appear well may be candidates for outpatient management providing the conditions listed above are met. Patients should be closely monitored until it is clear that the infection has been controlled. In general, providers should have a low threshold for hospital admission and intravenous antibiotics.
Preseptal cellulitis should be treated with warm compresses and antibiotics tailored toward the probable source of the infection. If outpatient management is elected (see above), a broad-spectrum antibiotic, such as oral amoxicillin-clavulanate potassium, oral cefuroxime, or intramuscular ceftriaxone, would be appropriate (Donahue & Schwartz, 1998). The best choice for inpatient management would be combination of a third-generation cephalosporin (such as ceftriaxone or cefotaxime) with an antibiotic with gram-positive coverage, such as oxacillin. In patients with a history of chronic sinusitis, clindamycin should be substituted for oxacillin to provide coverage for anaerobes and gram-positive organisms (Barone & Aiuto, 1997).
Management of preseptal cellulitis should include an ophthalmologic examination if there is any doubt of the diagnosis or if the child does not rapidly improve within 24 hours on oral antibiotics. Similarly, an otolaryngology consultation should be obtained if chronic sinusitis is suspected. A computed tomography (CT) scan of the orbit and sinuses (axial and coronal views) should be ordered if there is any suspicion of orbital involvement.
Treatment of Orbital Cellulitis
Orbital cellulitis calls for immediate treatment and should be considered an emergency. Children must be admitted to a closely monitored pediatric setting. Cultures of blood (routine), purulent eye secretion if present, and abscess contents if surgical drainage is performed should be obtained. A spinal tap should be performed if central nervous system involvement is suspected (Uzcategui et al., 1998). Recent studies recommend that infants younger than 3 months undergo a full sepsis workup, including obtaining blood, cerebrospinal fluid, and catheterized or suprapubic urine cultures (Klassen & Rowe, 1992; Nozicka, 1995). After an expeditious fever workup, broad-spectrum intravenous antibiotics (ceftriaxone or cefotaxime and oxacillin or clindamycin) should be started. Axial and coronal CT scans of the orbits and sinuses should be obtained without delay both to delineate the extent of the process within the orbit and to identify the source of infection.
Both the ophthalmologic and otolaryngology services should be consulted immediately to evaluate fully children with orbital cellulitis. Further management should be guided by a multidisciplinary approach. Surgical drainage of an underlying abscess or ethmoiditis should be considered early in the course of treatment.
Orbital cellulitis can progress rapidly and may result in orbital abscess or permanent visual loss. Intracranial involvement occurs as a consequence of infection spreading through the superior orbital fissure. The devastating complications of orbital cellulitis include cavernous sinus thrombosis,
meningitis, and brain abscess. Therefore, aggressive therapy must be instituted without delay on presentation.
meningitis, and brain abscess. Therefore, aggressive therapy must be instituted without delay on presentation.
NASOLACRIMAL DUCT OBSTRUCTION AND DACRYOCYSTITIS
Pathology
Congenital nasolacrimal duct obstruction occurs in approximately 6% of healthy children (Campolattaro et al., 1997). By far the most frequent cause of epiphora during the first several years of life is nasolacrimal duct obstruction. At birth, a thin membrane frequently persists at Hasner’s valve, located at the junction of the nasolacrimal duct and the nasal mucosa, causing obstruction of the nasolacrimal system. When an intranasal duct cyst is present, this causes a more marked obstruction in the early perinatal period, causing congenital dacryocele (dilated lacrimal sac). Presence of a dacryocele frequently causes bouts of acute or chronic low-grade dacryocystitis.
History and Physical Examination
Epiphora secondary to nasolacrimal duct obstruction is often accompanied by an intermittent purulent discharge and crusted eyelids in the morning. Although a recent study contradicts the traditional teaching that newborns do not lacrimate at birth (Isenberg et al., 1998), symptoms usually do not manifest until 2 to 4 weeks of age. Symptoms of perinatal epiphora are usually related to a conjunctivitis (chemical or infectious). If the obstruction is above the nasolacrimal sac, only epiphora without purulent discharge may be noted. On examination, children have a prominent tear lake and may either have frank tearing or dried tear marks on their cheeks. Frequently pressure on the lacrimal sac causes expression of purulent material through the puncta.
Dacryocystitis may be either acute or chronic. In addition to epiphora and recurrent conjunctivitis as seen with simple nasolacrimal duct obstruction, dacryocystitis presents as an inflamed, tender mass over the lacrimal sac area, which may be associated with cellulitis.
Diagnostic Criteria
Epiphora is nonspecific, but the most common cause of chronic epiphora is nasolacrimal duct obstruction. This diagnosis is supported by a history of persistent tearing, recurrent conjunctivitis, and the findings on examination as described previously.
Other causes of epiphora fall under the category of overproduction of tears and occur much less frequently than obstruction. However, when evaluating for epiphora, one should inspect the eye for signs of irritation that might be the cause of excessive lacrimation, including eyelid malformations, malpositioning of eyelids or cilia, and foreign bodies.
Primary care providers should rule out congenital glaucoma in a child with epiphora. Classic symptoms of congenital glaucoma include epiphora, blepharospasm, enlarged cloudy cornea, and photophobia. Photophobia results from glare produced by corneal edema and is probably the most reliable sign of the triad. Intraocular pressure is elevated, and palpation of the globe through the eyelids reveals a firm globe and buphthalmos. Congenital glaucoma usually is bilateral. If congenital glaucoma is suspected, immediate referral to an ophthalmologist should be made. The treatment of congenital glaucoma is surgical, and medical therapy merely temporizes until the surgery can be performed.
Management
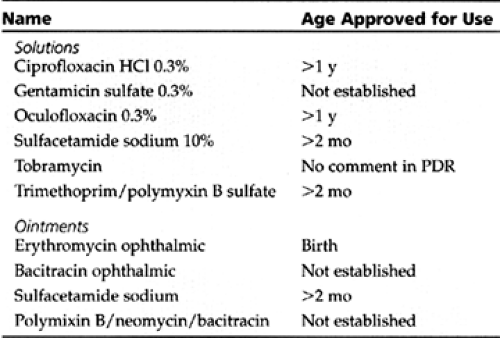
Initial treatment of nasolacrimal duct obstruction is conservative. With lacrimal sac massage and periodic topical antibiotics (Table 32-2) as needed to control discharge, a child may be observed up to 1 year of age unless symptoms are excessive. Most studies agree that by 1 year of age, 90% of cases have spontaneously resolved. Studies also have shown that spontaneous resolution of nasolacrimal duct obstruction after 1 year of age is unlikely (Nelson, 1998).
Primary care providers should teach nasolacrimal sac massage to parents. A finger should be firmly pressed on the sac (just below the medial canthus and under the orbital rim). Gentle pressure should then be exerted inferiorly to attempt to express lacrimal sac contents through the membrane at Hasner’s valve. A schedule easily remembered by parents, such as massage during each feeding period, should be recommended. Topical antibiotic drops or ointment (bacitracin ophthalmic ointment, erythromycin ophthalmic ointment, polysporin solution) should be prescribed whenever a child has purulent discharge.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree