Extremity Trauma
FRACTURES: GENERAL PRINCIPLES
The emergency physician must be thoroughly familiar with a variety of descriptive orthopaedic terms, which, when appropriately used, will greatly facilitate the care and disposition of patients with fractures. Because most significant bony injuries should be discussed with the orthopaedic surgeon and such discussion and any recommendations documented, the importance of precise anatomic location and description of the fracture cannot be overemphasized.
It is important for the emergency physician to communicate to what extent, if any, the previously normal appearance of the bone is now distorted by the fracture. This is performed by describing the position of the distal fragment in relation to the proximal fragment.
Fractures are said to be complete when both cortices are broken; incomplete fractures involve only one cortex.
Comminution occurs when more than two bony fragments are produced.
Fractures must always be defined as closed or open.
Two terms are used to describe any abnormalities noted: displacement and angulation.
Displacement occurs when the distal fragment moves laterally away from the proximal fragment but maintains alignment along the long axis. The extent of displacement is described in terms of the percent or fractional diameter of the distal fragment.
Angulation occurs when normal orientation of the long axis of the bone is deranged. With the patient in the anatomic position, the axis of the distal fragment with respect to the proximal fragment is noted. The amount of angulation, expressed in degrees, and the direction with respect to the proximal fragment are described.
It is important to note whether fractures enter the joint or involve the articular surface. If so, precise or anatomic reduction is usually required, and consultation should be obtained before disposition.
“Greenstick” and buckle (or “torus”) fractures, both of which are particularly common in children, are examples of incomplete fractures. A greenstick fracture occurs when stress is applied to a long bone in such a way that bowing or angulation persists in association with cortical disruption or breakage on one side. Such fractures often require manipulation, including fracture of the contralateral cortex, to restore normal realignment; consultation is therefore indicated in all patients.
Buckle (or “torus”) fractures are extremely common and, because of often subtle radiologic and physical findings, are often unrecognized in the emergency department (ED). If all cortical contours of the involved area are carefully examined, then point irregularity, notching, discrete wrinkling, or a subtle abnormality will be detected in patients with such fractures.
Fractures are described as transverse when cortical disruption occurs perpendicular to the long axis of the bone.
Spiral fractures occur in association with rotational stress and are seen to spiral down the shaft of the long bone.
Open or compound fractures occur when any actual or potential communication, however subtle, exists between the fracture and the outside environment.
Avulsion fractures imply that the bony attachment of ligaments or tendons has been pulled off as a result of excessive force applied to that attachment.
Impaction occurs when bone collapses into or onto bone. The proximal humerus is the bone most often described as impacted; however, depression of the tibial plateau and compression of vertebral bodies are other examples of impaction-type injuries.
In patients who may require manipulation or operative reduction, the patient’s history of allergies and anesthesia; the presence of other injuries, particularly involving the head, neck, chest, or abdomen; when the patient last ate; and whether religious or other reasons might prevent treatment in the usual manner are significant historic facts that should be obtained before orthopaedic consultation.
Common Errors in the Management of Patients with Fractures
Failure to provide treatment “as if a fracture were present” in patients with significant physical findings but “normal” x-ray results
Failure to immobilize the fracture with a sling or splint or to provide or recommend crutches to patients with significant soft-tissue injuries
Failure to arrange and document appropriate follow-up at an appropriate interval
Failure to examine and document neurovascular status in patients with proximal fractures
Failure to diagnose “clinical fracture of the navicular” in the presence of appropriate clinical findings but normal roentgenograms
Failure to diagnose “clinical fracture of the radial head” in the presence of appropriate clinical findings but normal roentgenograms
Failure to appreciate by physical examination subluxation of the radial head in children with normal roentgenograms
Failure to diagnose posterior dislocation of the shoulder
Failure to diagnose tibial plateau fracture
Failure to diagnose fractures of the fibula in patients with unimpressive histories and subtle findings
Consultation and Documentation
Because management differs significantly for a number of common fractures, we generally recommend orthopaedic consultation in fractures seen in the ED.
This ensures that the initial management and follow-up interval will be consistent with the wishes of the individual physician who will be responsible for the long-term care of the patient.
Neurovascular Status
Normal neurovascular status (specifically a statement noting the presence of normal motor, sensory, and vascular integrity) should be demonstrated and documented in all patients with proximal fractures.
If compromise of these functions is suspected or diagnosed, then immediate orthopaedic, neurosurgical, or vascular consultation should be obtained.
Open or Compound Fractures
Open fractures occur when a potential or actual communication exists between the fracture and the external environment.
Treatment must be individualized according to the bone involved, the nature of the fracture, and the extent of contamination; orthopaedic consultation should be obtained and documented in all such patients.
Many open fractures will be best treated in the operating room; these generally include proximal fractures; fractures with significant contamination; fractures entering joints; fractures requiring manipulation, reduction, or both; and fractures associated with tendinous or neurovascular injury.
Patients should not be allowed to eat or drink until the orthopaedic surgeon has determined whether definitive operating room, general anesthetic care will be required.
Open wounds, including protruding bone, should be covered with a sterile saline dressing. When operating room care will be required, irrigation should generally not be undertaken in the ED because surface organisms may be introduced further into the wound and adjacent tissues.
Protruding tissues, including bone, should be covered and left in place.
Externalized material should not be placed back into the wound because contamination has probably occurred and intraoperative debridement will be necessary.
Neurovascular status should be assessed and documented.
Patients with any compromise should be immediately discussed with the appropriate subspecialist.
Prophylactic antibiotic therapy is recommended in all patients with open fractures and should be instituted early and intravenously.
Establishment of bactericidal antibiotic levels in the fracture hematoma is the goal of prophylactic therapy.
Administer cefazolin (alternative: clindamycin 900 mg), 1 g, in the ED; an alternative is nafcillin, 1 g intravenous. Gentamicin, 1.5 mg/kg, should be added in contaminated open fractures.
Antitetanus prophylaxis should be administered as appropriate.
Analgesics should be administered in the ED unless a compelling contraindication (i.e., altered mentation) exists.
Stress Fractures
Stress fractures are frequently misdiagnosed as shin splints or soft-tissue injury.
The practitioner must recognize that stress fractures occur in the absence of significant trauma, frequently produce more chronic and less impressive symptoms, and often produce no radiologic abnormalities when the patient is first seen in the ED.
Definitive diagnosis is therefore extremely difficult; however, an appropriate history should provide grounds for a tentative or clinical diagnosis and the institution of appropriate therapy.
Most stress fractures occur in the lower extremity and under circumstances of recently initiated or accelerated activity.
A runner, for example, may have recently increased his or her distance or reinstituted an exercise program after a period of relative inactivity.
Common locations include the distal fibula, tibia, the metatarsals, and the femoral neck.
Discomfort with palpation over the fracture site is often present; however, swelling, if noted, is minimal.
Roentgenograms are initially normal, but if repeated 8 to 10 days after the onset of symptoms, they will often show evidence of periosteal reaction and bony sclerosis adjacent to the fracture site.
A radionuclide bone scan will be positive at 4 to 6 days and may be helpful in selected patients to confirm the diagnosis somewhat earlier.
Patients with suspected fractures should be provided with crutches, and a provisional diagnosis of stress fracture should be made.
The use of the involved extremity should be minimized until a definitive diagnosis is clear.
Buckle and Greenstick Fractures
Buckle fractures are separately discussed to emphasize the often subtle radiologic and clinical findings seen with these fractures, most of which occur in children.
Such fractures are infrequently displaced or angulated and are diagnosed on the basis of subtle wrinkling or notching of one side of the cortex; treatment, when a single bone is involved, is most often symptomatic and supportive.
Greenstick fractures occur when stress is applied to a long bone in such a way to produce persistent bowing or angulation; cortical breakage on one side is noted.
Angulation, which may be significant, requires reduction.
Radiologic findings in both groups of patients, particularly those with buckle fractures, may be subtle and are frequently overlooked.
A careful tracking of the cortical outline, which should define a smooth, gentle, uninterrupted curve, will disclose the site of fracture.
Other Fractures in Children
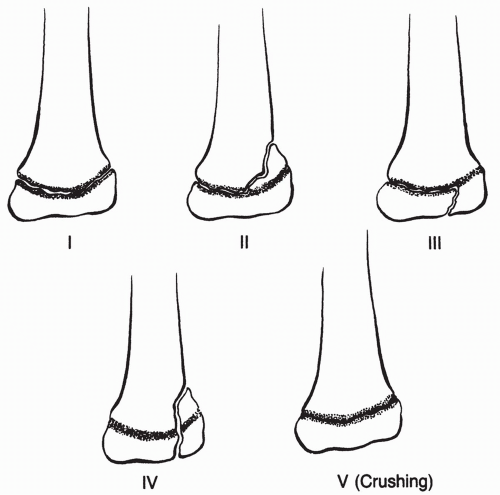
In addition to buckle and greenstick fractures, injuries involving the epiphysis, the cartilaginous, radiolucent area at or near the end of long bones from which future growth occurs, are common and must be accurately diagnosed (Fig. 10-1).
A high degree of suspicion regarding epiphyseal injury should be maintained, and when diagnosed, a conservative approach to treatment is appropriate; unfortunately, significant abnormalities of growth involving the injured epiphysis develop in approximately 10% of patients with epiphyseal fractures.
The most commonly involved areas, in decreasing order of frequency, are the distal radius, distal tibia, phalanges, and proximal humerus.
The peak age of occurrence is 12 years, and most patients are male.
Radiologic assessment of the involved area will allow a definitive diagnosis.
Salter and Harris have classified these fractures into five distinct categories:
Class 1: No bony disruption occurs, but slippage or separation of the epiphysis from the metaphysis is noted. Closed reduction is the treatment of choice.
Class 2: Separation through part of the epiphyseal plate occurs and a metaphyseal fracture is associated; treatment is by closed reduction.
Class 3: A fracture is noted extending from the joint space to the epiphyseal plate and then laterally to the periphery; treatment may be either open or closed reduction.
Class 4: These fractures extend from the articular surface through the epiphyseal plate and across the metaphysis; open reduction is usually required.
Class 5: These injuries involve severe crushing of the epiphyseal plate; displacement is unusual, and frequently these injuries are unappreciated. Growth disturbances are commonly associated with this type of fracture.
AMPUTATION AND REPLANTATION
Recent advances in replantation surgery dictate that most extremity amputations and thumb and multiple digit amputations are initially considered replantable and that attempts are made to preserve viable tissue.
The actual decision to proceed with replantation should be made after consultation by the emergency physician directly with the regional replantation team or surgeon.
Pertinent details include associated major injuries to the head, neck, chest, or abdomen; clear medical contraindications to transport or prolonged surgery; and whether fractures, extensive crushing, or other injuries involve the amputated part.
When these exist, when a single finger or the lower extremity is involved, when the patient is elderly, when extensive bacterial contamination is present, when a prolonged period of time between the injury and the institution of cooling has elapsed (i.e., more than 6 hours in the proximal arm and leg or more than 12 hours in distal amputations), or when severe degloving or avulsing is the mechanism of injury, the success of replantation is unlikely.
Conversely, patients with multiple digits amputated, particularly the thumb, amputations occurring in children, and those associated with a short period of warm ischemia, minimal bacterial contamination, minimal crushing of the amputated part, and no significant other major trauma are generally considered the best candidates for replantation.
These factors will be carefully considered by the transplant team. A general approach to initial treatment follows:
Initially, all amputations should be considered replantable and efforts made to preserve all tissue.
Given that bacterial contamination by hospital personnel is relatively common, sterile gloves should be worn when examining the patient and handling the amputated part.
Extensive bleeding, even with proximal amputations, is uncommon. Elevation of the stump and direct pressure, followed by a pressure dressing, are sufficient to arrest hemorrhage in virtually all patients. Blind clamping or ligating of vessels is to be avoided. When bleeding is extensive and uncontrolled by these measures, a proximal tourniquet or blood pressure cuff may be applied briefly.
Both wounds should be irrigated gently with Ringer lactate or normal saline solution; 250 mL to each site is adequate unless extensive contamination is present. More extensive irrigation and debridement should be deferred in most patients. The use of antiseptic solutions is discouraged.
The amputated part should be handled in a sterile manner and a sterile sponge dampened with Ringer lactate or normal saline solution applied to the wound. The part should then be wrapped in moist sterile towels and placed in a plastic bag; the bag should then be put in ice. Dry ice should never be used.
One gram of cefazolin, or a comparable agent, should be administered intravenously to adults and antitetanus prophylaxis should be administered if needed.
Analgesics may be administered, provided other injuries requiring frequent reassessments are not present.
Intravascular volume should be assessed and corrected if required.
A roentgenogram of the amputated part, particularly when crushing is the mechanism of injury, may be useful in estimating viability.
The replantation team should be contacted to discuss the feasibility of transport and replantation.
WRINGER-TYPE OR ROLLER-TYPE INJURIES
In the past, wringer washing machines accounted for the majority of wringer-type or roller-type injuries; however, today, machinery using closely approximated rollers is responsible for most such accidents.
Classically, the hands or fingers are involved and, importantly, the true extent of the injury is frequently underestimated at the time of presentation.
A conservative approach to the disposition and treatment of these patients is therefore warranted.
A variety of mechanisms may be associated with wringer-type trauma; these include heat injury, contusion, shearing or separation of tissue and tissue planes resulting in deep hematoma formation, peripheral nerve damage, avulsing or degloving of soft tissues, and fracture.
Information should be obtained as to the temperature of the machine, the mechanism of extrication, the actual width between the rollers, and the duration of contact.
Complete sensory and motor testing of the involved extremity should be undertaken initially.
Although sensory abnormalities are frequently neuropraxic in type and therefore recovery is expected, they cannot be assumed to be so at presentation.
Enhancement of discomfort or elicitation of pain with passive extension of the fingers or toes suggests injury to deep tissues and may represent or predict a future compartment syndrome.
Roentgenograms should be obtained to exclude associated fracture.
The treatment of patients with suspected or evolving significant injuries consists of in-hospital observation for 24 to 48 hours, meticulous irrigation and cleansing of open areas, strict elevation of the extremity, and early drainage in the operating room of subcutaneous or subfascial hematomas. Vascular status must be reassessed frequently to detect evolving ischemia.
Administer antitetanus prophylaxis as needed, and if injuries are open and extensive or if bacterial contamination is likely, then prophylactic antibiotics should be administered.
An appropriate antibacterial ointment may be applied to abraded areas.
Grafting should usually be deferred until local swelling has resolved.
PRESSURE OR GREASE GUN INJURIES
Devices generating high pressures to expel paint, grease, or other materials are now commonly used in the industry and may result in injury.
The hand is often involved, and the extent of injury is often underestimated at the time of presentation.
This occurs because the entry site associated with such injuries is often minor, and at presentation, patients may be minimally symptomatic.
Occasionally, if the material is radiopaque, a radiograph may demonstrate tracking of the material along the fascial planes.
Admission is recommended for observation, elevation, and early operative exploration and irrigation.
Patients presenting with established swelling, tenderness, or erythema along the tendon sheaths or fascial planes are candidates for admission, intravenous antibiotics, and early exploration and irrigation.
COMPARTMENT SYNDROMES
Crushing or penetration of tissues with resultant local hemorrhage and swelling may result in compromise of neural and vascular function; this may occur in open and closed injuries, although it is more common in the latter, in which case intact fascial planes operate to prevent expansion or decompression.
Most commonly, compartment syndromes occur in the forearm and the lower leg; however, the hand, fingers, and foot may become involved as well.
Penetrating injuries may result in compartment syndromes secondary to progressive hemorrhage that remains similarly confined.
Compartment syndromes are diagnosed on the basis of a high degree of suspicion and frequent reassessment of distal vascular and neural function.
Importantly, even in patients with evolving ischemia, distal pedal pulses may be present, and this must therefore not be used to exclude compartment syndrome; similarly, determination of flow by Doppler analysis does not exclude evolving vascular compromise.
The diagnosis is definitively made by directly measuring the pressure of the affected compartment.
There are many methods to accomplish this, but basically, a catheter and a pressure transducer are introduced into the suspected compartment, and measurements are made directly from this.
A resting pressure of 30 mm Hg is diagnostic of compartment syndrome.
When a significant proximal injury is associated with distal symptoms suggestive of neural ischemia (numbness, paresthesias, or pain) or when clinical evidence of vascular insufficiency exists (i.e., coolness, pallor, or reduced capillary filling), measures must be immediately undertaken to reduce local pressures.
A workup for rhabdomyolysis should be considered, especially if larger muscle compartments are involved.
Any restricting devices, such as wraps, casts, or splints, must be removed immediately; the extremity elevated; and emergency general or vascular surgical consultation for fasciotomy obtained.
If it is not immediately available and if ischemia is severe, then fasciotomy in the ED may be required to prevent necrosis.
SPECIFIC INJURIES OF THE UPPER EXTREMITY
Clavicle Fracture
Most clavicle injuries occur from a direct fall on the lateral shoulder or onto an outstretched hand.
Very young children who are unable to localize their discomfort are brought to the ED by parents because the child will not or cannot use the involved extremity.
The treatment of clavicular fractures is determined by the location of the fracture and, in the case of distal fractures, whether displacement is noted.
Fractures are of three types:
Group 1: Fractures involving the medial third of the clavicle
Group 2: Fractures involving the distal third of the clavicle
Group 3: Fractures involving the proximal third of the clavicle
Each group is made up of multiple subtypes depending on the fracture pattern.
Treatment
Treatment for group 1 and 2 clavicle injuries includes a simple sling for support and analgesics for comfort. Figure-of-eight slings are no longer widely employed for these fractures.
Patients with group 3 fractures may require operative reduction and internal fixation; definitive treatment should be discussed with the orthopaedic surgeon at the time of presentation.
Importantly, all patients receiving a sling should be instructed to remove the sling once each day and to fully rotate and extend the elbow; this is particularly true in elderly patients.
Sternoclavicular Injuries
Injury to the sternoclavicular joint may produce a simple sprain (first degree), subluxation (second degree), or actual dislocation (third degree).
Dislocation may be anterior or posterior and is associated with complete rupture of the sternoclavicular and costoclavicular ligaments.
Subluxation or second-degree sprain results from rupture of the sternoclavicular ligament; a partial tear of the costoclavicular ligament is also present in most patients.
Oblique views of the sternoclavicular area may demonstrate displacement in patients with subluxation or dislocation.
First-degree and second-degree sprains of the sternoclavicular joint require only supportive or symptomatic therapy and the avoidance of strenuous activity for 3 to 5 days.
Anterior dislocations should generally be treated conservatively initially, followed by resection in persistently symptomatic patients.
Posterior dislocations of the medial clavicle are important for the emergency physician to appreciate because they acutely require reduction if compression of the trachea, great vessels, or other vital mediastinal structures occurs.
In these patients, one or two sandbags or rolled towels should be placed in the middle of the back and the shoulders retracted posteriorly against the stretcher; this maneuver allows the medial clavicle to disengage itself from the sternum and move anteriorly. If reduction does not occur, then while the shoulders remain retracted, the lateral end of the clavicle must be pushed posteriorly in an attempt to lever the medial clavicle anteriorly. If this is unsuccessful, then after locally anesthetizing the overlying skin and medial clavicle (including the periosteum), the bone should be grasped with a towel clip and elevated into position; a figure-of-eight splint should then be applied, followed by orthopaedic consultation.
Patients without life-threatening symptoms related to mediastinal compression should be discussed with the orthopaedic surgeon, who may elect either operative or nonoperative reduction.
Acromioclavicular (AC) Injuries
Most such injuries occur when force is applied to the lateral or superior aspect of the acromion.
Injuries are graded as type I to VI.
Types IV to VI are rare and will not be discussed in detail.
Standard shoulder radiographs are usually adequate in confirming the diagnosis, but weight-bearing views should be employed in questionable cases.
Type I injuries are caused by a sprained AC and coracoclavicular (CC) ligaments and are diagnosed on the basis of tenderness over the AC joint. Minor swelling may be noted as well. Weight-bearing views of both AC joints are normal and symmetric.
Type II injuries are caused by torn AC ligaments but the CC is intact. They are diagnosed on the basis of tenderness, significant swelling, and mild deformity at the AC joint. If needed, weight-bearing views will demonstrate upward displacement of the lateral clavicle by not more than the diameter of the clavicle at that point.
Type III injuries are diagnosed on the basis of tenderness, swelling, and an obvious deformity at the AC joint; radiologically, weight bearing produces marked upward displacement of the lateral clavicle and an increased distance between the coracoid process and the clavicle.
Type I and II should be treated conservatively with a sling and analgesics as required. In these patients, early orthopaedic referral is recommended, primarily to institute a physical therapy program and to assess the patient’s progress. Patients may remove the sling for bathing and at night if symptoms are not excessive.
Type III injuries should be discussed with the consultant at the time of presentation because open reduction and internal fixation are often required for definitive repair.
Fractures of the Scapula
The scapula is fractured by direct blows and major torso trauma; thus, significant force has been exerted to the back, and concomitant injuries to the shoulder, neck, kidney, lung, and mediastinal structures must be considered.
Liberal use of chest CT (with fine cuts through the scapula to aid in surgical operative planning) is warranted.
Treatment depends on the severity of the fracture and ranges from a sling, analgesics as required, and early referral to institute a program of shoulder mobilization exercises to operative fixation.
Orthopaedic consultation in the ED is required.
Fractures of the Proximal Humerus and Shaft
Most fractures of the proximal humerus occur in elderly patients and are nondisplaced or minimally displaced fractures of the neck.
These may easily be treated, after orthopaedic consultation and demonstration of normal neurovascular function, with a simple sling, Velpeau bandage, or a commercial collar cuff and swathe. Analgesics and early orthopaedic to institute range-of-motion exercises are advised.
Patients with displaced or comminuted fractures, fracture dislocations, fractures involving the articular surface, and fractures occurring in the younger patient require consultation at the time of presentation because operative treatment may be elected.
Shaft fractures, particularly those that are distal, must be evaluated carefully because injury to the radial nerve may be associated. The patient should be evaluated for evidence of wrist drop, that is, inability to extend the wrist, fingers, or thumb.
Dislocation of the Shoulder
Ninety to ninety-five percent of glenohumeral dislocations are anterior, present with severe pain and immobility of the shoulder, and may be easily reduced by the emergency provider.
Posterior dislocations are uncommon; they occur in association with direct trauma, seizure, or electrocution; and present similarly to anterior dislocations.
Inferior dislocations (luxatio erecta) are extremely uncommon and present with the patient’s arm in full abduction with the humeral head against the axillary rib cage. This entity needs immediate orthopaedic consultation.
Because of deceptively normal anteroposterior views of the shoulder, posterior dislocations are undiagnosed in the ED in approximately 50% of patients. This is readily explained because pure posterior movement of the humeral head, if unassociated with displacement in any other direction, will appear relatively normal on routine anteroposterior views. However, slight lateral displacement of the humeral head, which radiologically produces less than the expected amount of overlap between the humeral head and the posterior rim of the glenoid fossa, is a clue to the presence of a posterior dislocation.
For this reason, anteroposterior, lateral, and axillary views of the shoulder are always indicated in patients with suspected shoulder dislocations.
Prereduction radiographs may not be needed if the patient has experienced repeated dislocations.
Radiographs should be done with adequate analgesics as acquiring these films can be quite painful. If severe pain and immobility persist, despite normal-appearing radiographs, a CT of the shoulder will disclose occult dislocations.
Shoulder dislocations are associated with severe discomfort, and most patients resist any movement of the extremity, particularly abduction.
Anterior dislocations typically produce a “square” shoulder when viewed from an anteroposterior perspective and a palpable, but often not visible, “step-off” below the now more prominent acromion.
Posterior dislocations produce palpable emptiness of the anterior compartment of the shoulder and a fullness posteriorly with prominence of the coracoid process.
The treatment of anterior dislocations follows; posterior and inferior dislocations may require reduction under general anesthesia, and therefore, prompt orthopaedic consultation is appropriate.
Coexistent fractures of the humeral head or glenoid are not uncommon and should be excluded radiologically before any attempt at reduction is made. When present, orthopaedic referral should be obtained.
Assessment and documentation of neurovascular status are important and should be performed before and after reduction in all patients.
Axillary nerve function should be evaluated in particular.
The treatment of anterior dislocations with respect to the method of reduction is highly variable.
Most reductions require procedural sedation for the patient to tolerate.
Traction-countertraction is the most widely employed technique but is falling out of favor for less traumatic reduction techniques. A sheet is placed around the supine patient’s thorax and held by one practitioner. A second practitioner grasps the affected slightly abducted arm with the elbow held in 90 degrees of flexion while providing traction and internal or external rotation until a clunk is felt as the shoulder is reduced.
The Stimson technique requires that the patient be placed prone while holding a 10-lb. weight. Reduction may take up to 30 minutes.
An increasingly popular variation of the Stimson technique is called scapular manipulation. This calls for the same weight-bearing, arm-hanging technique as in the Stimson’s, while a practitioner gently rotates the tip of the scapula medially using his or her thumbs.
External rotation is a technique employed with the patient in the supine position with the affected arm fully adducted. The elbow is flexed to 90 degrees and the arm is slowly externally rotated without traction.
If reduction is not successful, orthopaedic evaluation is mandatory.
Occasionally, general anesthesia will be required to achieve sufficient sedation and pain relief to overcome local muscle spasm and effect reduction.
A postreduction roentgenogram should be obtained and neurovascular function reassessed.
Significant tears of the rotator cuff may complicate dislocation; initiation of abduction should be demonstrated after reduction to exclude this injury.
Post-reduction treatment includes a sling and swathe, a short course of analgesics, and early orthopaedic follow-up in approximately 3 to 5 days to institute range-of-motion exercises.
Tears of the Rotator Cuff
The rotator cuff is made up of four muscles, which attach to the greater and lesser tuberosities of the humerus.
These include the supraspinatus (the most frequently torn of the muscles), subscapularis, infraspinatus, and teres minor.
Typical mechanisms that result in this injury include a fall on the outstretched arm, direct fall on the shoulder, or heavy lifting.
On examination, there is tenderness to palpation at the tuberosities, and abduction of the arm, particularly its initiation, is weak and elicits discomfort.
Roentgenograms are normal or may rarely demonstrate an avulsion-type injury to the tuberosity.
Definitive diagnosis is made by MRI.
Treatment is somewhat dependent on the patient’s age, lifestyle, and extent of disability present.
In the young patient with a large tear or an associated avulsion fracture, the threshold for early repair is reduced, whereas a period of observation is generally elected for the older patient.
Orthopaedic outpatient follow-up is appropriate for such patients.
Radial Nerve Palsy
Penetrating trauma to the axilla, dislocation of the shoulder, humerus fracture, and pressure neuropathies may all produce radial nerve palsy.
Pressure neuropathies may result from crutches that are too long for the patient, placing undue pressure in the axilla. The so-called Saturday night palsy results from the arm being hung over a chair during alcohol-induced sleep.
The radial nerve can also be injured when medications are injected into the posterior portion of the upper arm.
Signs of radial nerve impairment include loss of wrist extension, loss of finger and thumb extension, and weakness of both elbow flexion, caused by brachioradialis impairment, and supination.
Very proximal lesions may also produce loss of elbow extension secondary to triceps paralysis.
Sensory loss is most consistently noted to involve the dorsal aspect of the hand.
Treatment includes orthopaedic or neurologic referral, physical therapy, and the application of a wrist splint in the position of function.
Biceps Brachii Rupture
Rupture of the biceps may occur distally in the biceps tendon, in the bulk of the muscle, or in the tendon of the long head of the biceps.
Most ruptures occur traumatically when excessive or sudden stress is applied across the bicep.
The diagnosis is based on this history, and most patients report an audible or palpable “snap” or the sudden sensation that the muscle has given way or is weakened at the time of rupture.
This sensation is followed by local discomfort, a palpable defect or step-off along the bicep, or a proximally bulging or “Popeye-”type muscle.
An acute rupture of the distal tendon is treated surgically, whereas muscle and long tendon ruptures are most often treated conservatively with an initial period of cold application, analgesics as required, and restriction of activity.
A sling is recommended for several days, to be removed at night, and orthopaedic follow-up in 3 to 5 days is advised.
Injuries to the Elbow
To the nonradiologist, the bones of the elbow, particularly in the child with incomplete ossification, represent an extremely difficult area.
Because of this and because some fractures may not be apparent on initial views, a very conservative approach to the treatment of elbow injuries, particularly in children, is warranted.
A relatively low threshold for obtaining consultation or requesting contralateral views of the uninjured elbow for comparison should be maintained.
Fractures
Proximal Radial Head and Neck
Patients with fractures involving the radial head or neck, often occurring as a result of trivial trauma, present with often poorly localized discomfort to the area of the proximal radius.
Because initial roentgenograms may be normal despite the presence of a fracture, the physician must be aware of the important clinical signs suggesting this injury; these include accentuation of discomfort with rotation of the forearm and with hyperflexion and hyperextension of the elbow.
When these signs are present despite a normal initial study, a diagnosis of “clinical or occult fracture of the radial head or neck” is justified.
The diagnosis is further suggested when the so-called posterior fat-pad sign is present; this is seen as a radiolucent area posterior to the distal humerus on the lateral view of the elbow and suggests intra-articular bleeding.
The anterior fat-pad sign, or sail sign, is not as diagnostic of injury when small, because this can be a normal finding.
When an occult or clinical fracture is diagnosed on the basis of clinical signs (and negative x-rays), patients should understand that although a possible fracture exists, it cannot be definitely diagnosed until a healing line is noted in approximately 10 to 12 days.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree