The Nature of Chronic Pain
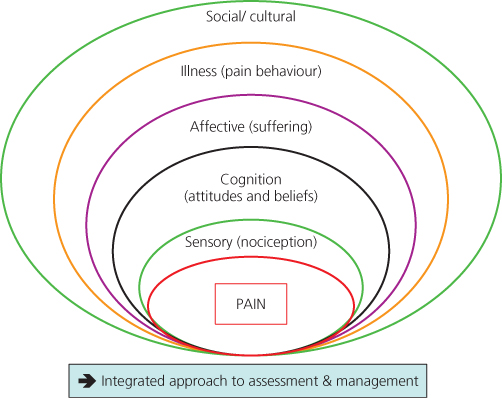
The exact pathophysiology underlying many common pain problems (e.g. back pain, headache) is largely unknown. Conversely, 30% of asymptomatic individuals who reveal structural abnormalities on imaging studies suggestive of pain do not report pain. These observations suggest factors other than detectable physical pathology contribute to the report of pain. Thus, comprehensive assessment of the patient with chronic pain requires examination of psychosocial and behavioural factors as well as physical pathology (Figure 3.1).
Figure 3.1 A biopsychosocial model of chronic pain. Many factors contribute to the pain experience and associated distress. These are closely inter-related: a dichotomous view of pain as being ‘physical’ or ‘psychological’ is not helpful.
The busy clinician may be concerned that a comprehensive assessment will require an excessive amount of time. There is no way around the problem. However, the assessment may be performed over several brief appointments and components involving patient completion of self-report questionnaires do not require clinician time beyond scoring and interpretation. The initial time for assessment may reduce the amount of time required throughout treatment.
Medical and Physical Evaluations
History and Physical Examination
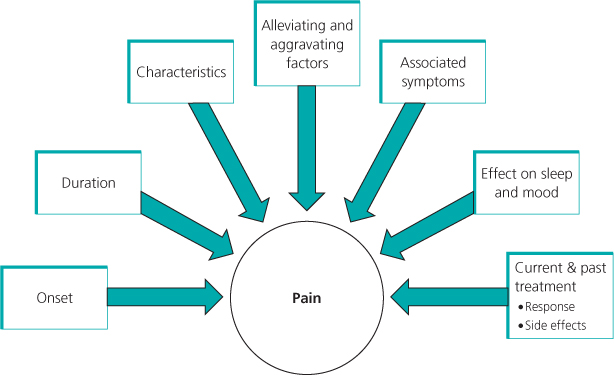
Medical assessment of a patient with persistent pain begins with a current and past history and physical examination. In addition to a general medical history, the healthcare provider should inquire in some detail about the pain (Figure 3.2). A physical examination should not only include a review of systems but also an assessment of physical functioning.
Laboratory testing and imaging procedures can rule out structural or biochemical abnormalities. However, physicians must not over-interpret either the presence or absence of objective findings unless they are consistent with the history and physical examination.
Psychological Assessment
The healthcare provider should consider and evaluate the ‘whole’ patient, not just reported symptoms. Regardless of a documented organic cause for pain, the evaluation process can be helpful in identifying how biopsychosocial factors interact to influence the nature, severity, persistence of pain and disability, and response to treatment. This assessment is also helpful in treatment planning and anticipation of responses to treatment. General assessment considerations are illustrated in Box 3.1.
Interviews
Semi-structured interviews can be used to assess the myriad of psychosocial factors related to pain and disability. Not all patients require a detailed psychosocial evaluation. Outlined in Box 3.2 is a range of points that can be used as pre-screening questions with patients who report chronic pain and as a basis for determining whether a more thorough psychological evaluation is warranted.
History of and current controlled- and illicit-substance use is important as some patients use opioid analgesics to manage their mood, and some have side effects that mimic the symptoms of depression (e.g. mood changes, altered sleep). Psychological dependence and aberrant behaviours related to prescribed pain-relieving medications and illicit drugs should be evaluated. A record of prescribed controlled substances and urine toxicology screening should be obtained and documented.
Referral for further evaluation may be indicated when the following are present:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree