Evaluation of Hearing Loss
Neil Bhattacharyya
It is estimated that more than 10% of the population of the United States has a hearing problem. The problem is particularly common among the elderly and can impair quality of life. People with seriously impaired hearing often become withdrawn or appear confused. Subtle hearing loss may go unrecognized. Patients with hearing loss often can be greatly helped, particularly if the loss is due to a conductive problem. The primary physician has the responsibility to screen and detect hearing loss, to search for an etiology, and to decide when referral to an otolaryngologist is indicated.
Basic Mechanisms of Hearing and Their Impairment
Hearing impairment may result from an interference with the conduction of sound, its conversion to electrical impulses, or its transmission through the nervous system. Hearing involves an acoustic stage during which sound waves cause the tympanic membrane to vibrate. The tympanic membrane and the ossicles amplify the sound, and the oscillation of the footplate of the stapes in the oval window transmits the sound energy to the perilymph of the inner ear. The endolymph of the scala media (or cochlear duct) is wedged between the perilymph of the scala vestibuli and the scala tympani. Displacement of the basilar membrane stimulates the hair cells, converting sound waves to neural impulses, which are conveyed to the temporal lobes.
On the molecular level, during the reception of sound, potassium ions flow through the upper surface of the cochlear hair cells; the ions then recycle by flowing down to the base and supporting cells and into the endolymph. Connexin, the “gap protein” that allows small molecules to pass from one cell to the next, facilitates this potassium flow. It is synthesized by the cells surrounding the sensory hair cells of the cochlea and by the fibrocytes of the cochlear duct.
Interference with mechanical reception or amplification of sound, as occurs with disease of the auditory canal, tympanic membrane, or ossicles, creates conductive hearing loss. A conductive hearing loss is localizable to the external auditory canal or the middle ear in most cases. Degeneration or destruction of hair cells or the acoustic nerve produces sensorineural hearing loss, as do defects in the synthesis of connexin. Genetic studies have facilitated the uncovering of a molecular basis for hearing loss. Mutations in the gene that codes for connexin are associated with nonsyndromic hearing loss, both early in life and with aging (see later discussion). Congenital malformations of the inner ear, not necessarily hereditary, may also compromise hearing at the sensorineural level.
Conductive Hearing Loss
Conductive loss presents with diminished perception of sound, particularly for low-frequency tones and vowels. There is often
a history of previous ear disease. In the Weber test, a tuning fork placed against the frontal bone or the maxillary incisors is perceived more loudly in the ear with a conductive hearing loss. The Rinne test shows that bone conduction is better than air conduction. Obstruction of the auditory canal by severely impacted cerumen, a foreign body, exostoses, external otitis, otitis media with effusion, or scarring or perforation of the drum due to chronic otitis may be responsible for the conductive loss.
a history of previous ear disease. In the Weber test, a tuning fork placed against the frontal bone or the maxillary incisors is perceived more loudly in the ear with a conductive hearing loss. The Rinne test shows that bone conduction is better than air conduction. Obstruction of the auditory canal by severely impacted cerumen, a foreign body, exostoses, external otitis, otitis media with effusion, or scarring or perforation of the drum due to chronic otitis may be responsible for the conductive loss.
Otosclerosis
Otosclerosis, a surgically remediable cause of conductive hearing loss, is a disorder of the bony labyrinth that fixes the footplate of the stapes in the oval window. Clinical otosclerosis has an estimated prevalence of about 1% among whites and 0.1% among blacks. Two thirds of the cases are seen in women. There appears to be an association between pregnancy and progression of otosclerotic hearing loss. The condition is believed to be inherited in an autosomal dominant fashion, with varying clinical expressivity. It generally presents in the second or third decade of life.
Exostoses
Exostoses are bony excrescences of the external auditory canal. They are characteristically located in the anterior, posterior, and superior quadrants of the canal. Nearly always bilaterally symmetric, their occurrence seems to be related to repetitive exposure to cold water (e.g., as in ocean swimming). They can cause symptoms by blockage of the external auditory canal, resulting in conductive hearing loss, or by sequestration of debris and cerumen with subsequent infection.
Glomus Tumors
Glomus tumors or paragangliomas are rare benign, highly vascular tumors derived from normally occurring glomus formations of the middle ear and the jugular bulb. Presenting symptoms include conductive hearing loss (from middle ear mass effect), spontaneous hemorrhage from the canal, and paralysis of the ninth, tenth, and eleventh cranial nerves (the jugular foramen syndrome). Pulsatile tinnitus should raise suspicion for a glomus tumor. With progression, it may involve the intracranial space or cause bony destruction of the base of the skull.
Otitis Media with Effusion
Chronic otitis media with effusion is a rare diagnosis in adults. Causes include nasopharyngeal masses, viral upper respiratory infection, allergy, and, rarely, autoimmune conditions. Ninety percent of adult middle ear effusions resolve spontaneously within 3 months. A persistent middle ear effusion in an adult requires exclusion of nasopharyngeal carcinoma, typically by nasal endoscopy.
Sensorineural Hearing Loss
Sensorineural loss arises from dysfunction of the cochlear sensorineural elements and/or of the cochlear nerve. Patients may complain that they can hear people speaking but have difficulty deciphering words because speech discrimination is poor. Shouting may only exacerbate the problem. The patient with high-frequency loss may have difficulty hearing doorbells, telephones, fire alarms, or a ticking watch and may note more difficulty in hearing the higher-pitched female or child’s voice. Recruitment—an abnormally rapid increase in perceived loudness with increased sound intensity—may be present and indicates cochlear dysfunction. With Rinne testing, air conduction is perceived better than bone conduction. Tinnitus of varying degrees and intensity is often a concomitant complaint.
Presbycusis
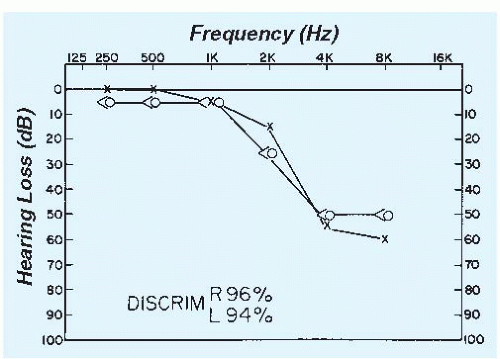
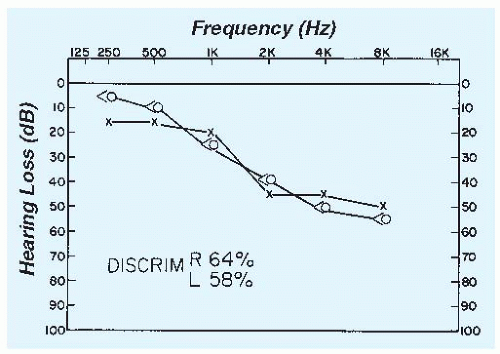
Presbycusis is hearing loss associated with aging and is the most common cause of diminished hearing in the elderly. There are four types of presbycusis, distinguished according to the correlated pathologic changes in the cochlea. Hair cell loss and cochlear neuron degeneration are the most widely recognized changes. The hearing loss is bilaterally symmetric and gradual in onset. Most cases begin with a loss of the high frequencies with slow progression. Eventually, middle- and low-frequency sounds also become difficult to perceive (Figs. 212-1 and 212-2).
Noise-Induced Hearing Loss
Noise-induced hearing loss is of major epidemiologic and economic significance. Chronic exposure to sound levels in excess of 85 to 90 dB causes hearing loss, particularly in the frequency range around 4,000 Hz. The patient may be unaware of the problem because the speech frequencies (500 to 4,000 Hz) are initially unaffected. At first, there may be a temporary threshold shift in which there is a reversible elevation in the threshold for sound
perception. The ear may feel full, or the patient may complain of a sense of pressure. If loud noise exposure ceases at this point, hearing returns to its previous level. If exposure persists, however, a permanent threshold shift ensues. The term acoustic trauma more specifically relates to a particular single noise event (e.g., a shotgun blast) that induces an immediate irreversible hearing loss.
perception. The ear may feel full, or the patient may complain of a sense of pressure. If loud noise exposure ceases at this point, hearing returns to its previous level. If exposure persists, however, a permanent threshold shift ensues. The term acoustic trauma more specifically relates to a particular single noise event (e.g., a shotgun blast) that induces an immediate irreversible hearing loss.
Drug-Induced Hearing Loss
The aminoglycoside antibiotics, such as gentamicin, are representative of ototoxic drugs. An early sign of gentamicin ototoxicity is disequilibrium. Monitoring antibiotic blood levels is the best, but not perfect, way to avoid such problems, adjusting dose according to peak serum levels. Restricting dosing to once daily and duration of therapy to less than 1 week also helps to reduce risk. Other potentially ototoxic drugs, including those causing symmetric sensorineural hearing loss, include furosemide, ethacrynic acid, cisplatin, quinidine, and aspirin. Aspirin doses averaging 6 to 8 g/d predictably cause tinnitus and completely reversible hearing impairment.
Ménière Disease
Ménière disease manifests most commonly with a unilateral, fluctuating, low-frequency, sensorineural hearing loss, usually associated with tinnitus, a sensation of fullness in the ear, and intermittent episodes of vertigo each lasting hours to 1 to 2 days. Vertigo may be the presenting symptom of Ménière disease, with later onset of fluctuating hearing loss. Progression of hearing loss may occur, eventually encompassing the higher frequencies as well.
Acoustic Neuromas
Acoustic neuromas—benign tumors of the eighth cranial nerve—are rare but important considerations in the evaluation of asymmetric sensorineural hearing loss, often in conjunction with disequilibrium (see Chapter 166). Speech discrimination is much worse than predicted by the pure-tone hearing loss. Symptoms progress in relentless progressive fashion.
Sudden Sensorineural Hearing Loss
Sudden sensorineural hearing loss (defined as occurring over no more than a 72-hour period with a subjective sensation of hearing impairment in one or both ears) can appear with or without obvious cause or warning. Often the cause is not evident even after assessment, but schwannoma (acoustic neuroma), stroke, and malignancy need to be ruled out in cases of sudden unilateral hearing loss. Cases without evident cause after workup are designated idiopathic sudden sensorineural hearing loss. The etiology of the idiopathic variant is a matter of debate, but viral infection and vascular insufficiency are among the postulated mechanisms. Men and women are equally affected, with frequency greatest between ages 43 and 53. Up to half present with transient vestibular symptoms. Recovery correlates with pattern of hearing loss, age (>40 years or <40 years), presence or absence of vertigo (those without vertigo fare better), and electronystagmogram pattern. Over a third of patients recover spontaneously and some may never come for care.
Hereditary Sensorineural Hearing Loss
Hereditary sensorineural hearing loss is generally bilaterally symmetric. Many syndromes have been identified in which hereditary hearing loss is associated with anomalies in other organ systems, but nonsyndromic hereditary hearing loss is also recognized. Among persons with isolated (“nonsyndromic”) hearing loss, there is a high frequency of mutations in the gene GJB2, which codes for the synthesis of connexin. Mutations in this gene are found not only among congenitally nonsyndromic deaf children, who are usually homozygous for the mutation, but also in the carrier state among adults with late-onset isolated hearing loss. The frequency can be as high as 3% across many different populations. It is suspected that the carrier state may predispose to hearing loss later in life and account for some, if not many, cases of age-related hearing loss that are commonly encountered. More work is needed to confirm these intriguing and potentially important findings. Although screening for mutations of this gene is not difficult, the degree of hearing loss and its time of onset cannot yet be predicted. A small number of patients may exhibit a unilateral, genetically programmed sensorineural hearing loss later in life. Family history is important.
Injury
Injury to the inner ear or cochlear nerve may produce an asymmetric sensorineural hearing loss. Skull fracture, meningitis, and mumps are major etiologic factors. Trauma may also cause conductive hearing loss, for example, hemotympanum, tympanic membrane perforation, or ossicular dislocation.
Other Etiologies
Congenital Syphilis. Congenital syphilis may produce adultonset sensorineural hearing loss. One or both ears may be affected; the course can be variable, with remissions and exacerbations. Vertigo is sometimes present as well, producing a symptom complex mimicking Ménière disease.
Multiple Sclerosis. Multiple sclerosis should be considered when a young woman shows discrimination scores reduced out of proportion to the pure-tone thresholds (similar to the pattern seen with acoustic neuromas). The site of the lesion is retrocochlear (often in the brainstem), and there may be an associated history of optic neuritis and/or vertigo.
Perilymph Leaks or Fistulas. Perilymph leaks or fistulas may cause hearing loss, with or without vertigo, in individuals who have had inner ear surgery (e.g., stapedectomy), have sustained head trauma, or have congenital inner ear anomalies. The round and/or oval windows may be involved, and it is theorized that there is intracochlear membrane rupture as well. Surgical repair may be required. Expeditious referral to an otolaryngologist should be considered.
DIFFERENTIAL DIAGNOSIS
The causes of hearing loss can be grouped according to whether the problem is conductive or sensorineural (Table 212-1). The categorization is of practical use because the conductive defects lend themselves to correction in many instances. The causes of sudden sensorineural hearing loss are particularly important to consider (Table 212-2).