Chapter 2 Establishing the Diagnosis of Discogenic Back Pain
An Evidence-Based Algorithmic Approach
 The predictive value of modalities used to diagnose discogenic pain depends directly on the pretest probability of the disease.
The predictive value of modalities used to diagnose discogenic pain depends directly on the pretest probability of the disease. With proper patient selection and standardized diagnostic criteria, discography has a high degree of predictive value for discogenic pain.
With proper patient selection and standardized diagnostic criteria, discography has a high degree of predictive value for discogenic pain. Educate the patient in advance about the nature and process of the diagnostic intervention that he or she is going to have.
Educate the patient in advance about the nature and process of the diagnostic intervention that he or she is going to have. Educate the patient in advance on the proper use of the numerical rating scale (NRS) by providing specific examples of mild, moderate, and severe pain ratings.
Educate the patient in advance on the proper use of the numerical rating scale (NRS) by providing specific examples of mild, moderate, and severe pain ratings. Avoid excessive sedation when performing diagnostic interventions because it may lead to increased false-negative or false-positive responses and an increased complication rate.
Avoid excessive sedation when performing diagnostic interventions because it may lead to increased false-negative or false-positive responses and an increased complication rate.Discogenic Pain: A Diagnostic Challenge
The concept of pain arising from the intervertebral disc (IVD) dates back to the 1940s.1 Discogenic pain is among the most common and most challenging of the diagnoses that the pain physician must confront. This premise remains as true today as it did in 1970 when Crock2 first described internal disc disruption (IDD) characterized by radial fissures or tears through the annulus fibrosis (AF) despite a normal or near-normal disc contour. The term discogenic pain refers to pain arising from the disc itself in contrast to nerve root pain caused by disc protrusion.
General Principles of Diagnostic Testing
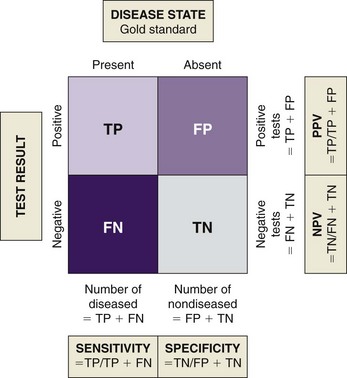
Sensitivity and specificity are parameters used to describe accuracy. Sensitivity is a measure of false-negative rates. Specificity is a measure of false-positive rates. Fig. 2-1 demonstrates the relationship among the parameters used to measure accuracy of laboratory tests. A test that is 100% sensitive would detect all cases in which the disease may be present. A test that is 100% specific would detect only those cases in which the disease is certain to be present and exclude all cases in which the disease is absent. In reality, diagnostic medical tests never reach this ideal level of accuracy, leaving some degree of uncertainty regarding the diagnostic information.3
Principles of Medical Decision Making
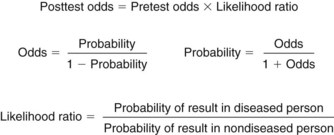
Despite the limitations in determining their accuracy, diagnostic tests and interventions serve a valuable purpose. When viewed from the perspective of probability, these tests and interventions help the clinician deal with the inherent uncertainty of clinical decision making.4–6 The probability that the results of a diagnostic test are valid may be influenced by factors inherent to the test such as sensitivity and specificity and the clinical setting in which the test is applied. Bayes’ theorem is a mathematical expression of conditional probability and a governing principle of diagnostic testing (Fig. 2-2). According to Bayes’ theorem, the posttest odds of a test result are directly proportional to the pretest odds multiplied by the likelihood ratio for the test result, which is a function of the prevalence of the disease. In clinical terms the prevalence of a disease process directly affects the degree of meaning of the test results. When the prevalence is high, there is a higher probability that a positive result indicates the presence of the disease.7 Conversely, interpretation of a test result in a population in which the prevalence is low has limited value.
The positive predictive value (PPV) is the proportion of patients with positive test results who are correctly diagnosed.8 PPV indicates the probability that a positive test reflects the underlying condition being tested for and is the most important measure of a diagnostic method. However, its value does depend on the prevalence of the disease, which may vary. Therefore results of diagnostic tests are not absolute. They must be interpreted in the context of the specific clinical conditions where the test is applied.
The various measures of accuracy and reliability of diagnostic tests may be expressed in terms of validity or the soundness of diagnostic interventions. Many types of validity have been described, but the terms are not necessarily defined in a consistent manner among all practitioners. Concept validity examines the theoretical basis of a test such as the anatomical or physiological basis of an intervention. Diagnostic blocks have concept validity because a pain generator may be identified based on anatomical and physiological basis. In effect, the structure may be anesthetized, resulting in pain relief. Content validity requires that a test or intervention be clearly and accurately defined. For an intervention to have content validity the clinician must adhere to the accepted definition. This allows for a valid comparison of results both within and between various samples. Face validity requires that an intervention actually achieves its intended goal on an anatomical and physiological basis. Face validity may be established on a statistical basis using a large-scale study by demonstrating that, if content validity is achieved, a specific result may be expected by all practitioners. Face validity may also be demonstrated on an individual basis. For example, in case of diagnostic blocks, administration of contrast medium under fluoroscopic imaging may demonstrate selective spread of contrast at the target site and avoidance of spread to adjacent structures. Construct validity measures the extent to which a test correctly distinguishes the presence or absence of the condition that the test is designed to detect. Construct validity is measured using the principles of diagnostic testing and clinical decision making described previously. Face validity and construct validity are critical features of any diagnostic intervention. Finally, predictive validity is a measure of the ability of a diagnostic intervention to predict successful treatment outcome. This constitutes the therapeutic use of the diagnostic intervention.9
Sources of Pain in the Spine
Because of the multiple pain-producing structures in the spine, it may be difficult to determine the exact source of back pain (Box 2-1). Often discogenic pain is a diagnosis of exclusion when other areas of the spine have been ruled out as potential causes. Many structures in the spine are known or have a high likelihood of producing pain. This section discusses the different pain-producing structures implicated in the production of spine pain to aid in the differential diagnosis (Box 2-2).
Zygapophyseal Joint Pain
Morphological studies on humans10–12 have demonstrated neuropeptides and nerve endings in the facet joint capsule. Although it remains controversial, pathology within these joints appears to result in significant back pain, which should be ruled out before diagnosing discogenic pain.
Sacroiliac Joint
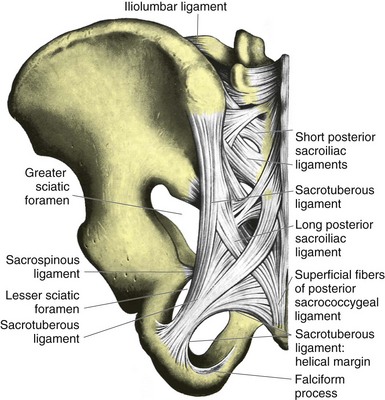
As with the facet joint, there has been controversy about the sacroiliac joint (SIJ) (Fig. 2-3) as a cause of low back pain (LBP). However, many clinicians believe that the potential for this joint to cause pain is underestimated.13–17 The SIJ is classified as a diarthrodial joint; however, with age the joint develops fibrous adhesions, which restrict movement.18,19 This restriction of movement decreases the buffering capacity of the joint, which may lead to chronic pain. Like the facet joints, the SIJ is richly innervated with both free nerve endings and mechanoreceptors. The innervation has been extensively described and supports the belief that this joint is a pain-sensitive structure.20–22
Intervertebral Disc
Nerve endings capable of transmitting pain impulses are abundant in the outer one third of the AF in the IVD.23–26 In addition, nerves within the IVD contain neuropeptides, which are involved in pain transmission.27 Injuries in the AF may result in pain while the external appearance of the disc remains normal, with no direct or obvious nerve root involvement. 28
Ligaments of the Spine
Many ligamentous structures in the spine are innervated with free nerve endings. However, the density of this innervation varies. Of all of the ligamentous structures, the posterior longitudinal ligament appears to be the most heavily innervated with free nerve endings,29–31 and the ligamentum flavum the least innervated.32
Degenerative changes within these ligaments may result in sensitization of free nerve endings, leading to chronic pain. In addition, the close proximity of the anterior and posterior longitudinal ligaments to the discs makes these structures susceptible to exposure to the disc contents in the event of disc rupture (see Chapter 1, Fig. 1-5). The disc contents may induce an inflammatory process in these ligaments, leading to pain.
Nerve Root
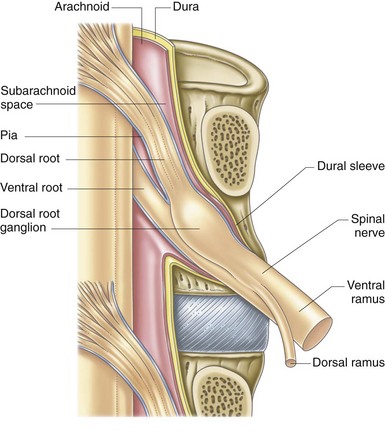
The nerve root is innervated by the sinuvertebral nerve, which branches from the segmental nerve and travels backward into the neural foramen. The arachnoidal covering of the nerve root is heavily innervated and a source of pain (Fig. 2-4). Mechanical compression or irritation of these structures can lead to pain in the extremities that is associated with neurological changes. The nerve root may be stimulated mechanically by disc herniation, osteophyte formation, foraminal narrowing caused by degenerative disc disease (DDD), or tumor invasion. In addition, it has been postulated that both the disc and facet joint contents may induce an arachnoiditis; however, Haughton, Nguyen, and Ho33 showed this only to be true for the disc contents.
Clinical Evaluation of the Patient with Discogenic Pain
Targeted History
History and physical examination have limited specificity for discogenic pain. However, they serve two critical functions that make the clinical evaluation the foundation for establishing the diagnosis of discogenic pain. The first and most important role of the clinical evaluation is identification of “red flags” that may indicate presence of sinister pathology. Second, it is through a careful and detailed history and physical evaluation that the clinician identifies the population of patients with a high pretest probability for discogenic pain. Red flags that require immediate attention include recent trauma, mild trauma or strain with a history of osteoporosis, unexplained weight loss, history of cancer, fever, pain worse at night, bowel or bladder dysfunction, intravenous drug use, and pain that is not relieved in the supine position or that awakens the patient from sleep.34
The history should look for signs of nondiscogenic pain. Although the signs taken in isolation are not very valuable, together with the physical examination and diagnostic testing they can prove to be helpful. Lumbar facet pain is worse in the morning and with inactivity and is aggravated by extension, rotation, and side bending of the spine to the diseased side. Pain from the SIJ is usually referred to the buttocks, groin, posterior thigh, and occasionally below the knee.35–38 The pain worsens with bending and prolonged sitting and improves with walking or standing.35,39
Symptoms that tend to be more associated with discogenic pain include increased pain with sitting, flexion, coughing, sneezing, or activities that increase intradiscal pressure such as straining. A case report of a subject demonstrated that disc pressures progressively increased with the following positions: supine < lateral decubitus < standing < sitting < standing with forward flexion < sitting with forward flexion < standing with forward flexion against resistance < sitting with forward flexion against resistance.40 There are no studies that correlate these positions with the diagnosis of discogenic pain. The symptoms described in the history should not be taken at face value but rather used as a whole with physical findings and diagnostic tests.
Physical Examination
Lumbar facet pain rarely produces true radicular pain into the extremity; but, because of the close association of the facet joint with the nerve root, true radicular symptoms can occur with facet joint disease (i.e., synovial cysts, facet hypertrophy, or osteophytes).41 Therefore a neurological examination should be performed, especially for pain radiating below the knee, to look for nerve root compression. If side bending results in pain on the opposite side, soft tissue pain should be entertained. Because of the anatomical location of the facet joints, the physical examination of facet pain appears to be nonspecific, and the diagnosis relies more on symptomatology and diagnostic blockade.
Because of the anatomical location of the SIJ, this structure is difficult to examine; and many of the provocative tests may result in false-positive responses and inter-tester variability.42,43 However, there are several provocation tests that are easy to interpret and reliable.44,45 Gillet’s test notes the change in relationship of the upper sacral spinous process and the posterior superior iliac spine (PSIS). When the patient is standing, these processes are located on the same plane. When the patient is asked to lift one leg, under normal conditions the ipsilateral PSIS moves inferiorly relative to the spinous process. In a patient with sacroiliac dysfunction the PSIS remains at the same level or moves superiorly. Patrick’s test is performed with the patient in the supine position. The patient is asked to cross one leg with the ankle placed just above the opposite knee. The examiner then pushes the knee of the crossed leg toward the floor. This test stresses the hip and the SIJ. If hip pathology is present, pain is produced in the lateral hip and groin. If SIJ pathology is present, pain is produced over the sacroiliac junction. Gaenslen’s test is performed with the patient in the supine position. This test is performed by maximally flexing the hip on one side and maximally extending the hip on the opposite side. This test stresses both joints simultaneously and is positive if pain is produced over the sacroiliac junction. Yeoman’s test is performed with the patient in the prone position. The hip is maximally extended by lifting it off the table. A positive test produces pain over the sacroiliac junction. This test may also stress the lumbar facet joints, and pain produced over the lower back is positive for facet pain. The sacroiliac shear test is performed with the patient in the prone position. The palm of the hand is placed over the posterior part of the ilium and thrust anteriorly. If positive, this test produces pain over the sacroiliac junction. The hip rotation test evaluates the integrity of the musculature surrounding the SIJ. If SIJ pain is present, reflex muscle spasms may limit its mobility. Under normal conditions external rotation of the leg lengthens the leg, and internal rotation shortens the leg. If SIJ pain is present, this lengthening and shortening does not occur.
Two additional examinations have been proposed to be more specific for detection of discogenic pain: centralization phenomenon (CP) and the bony vibration test (BVT). CP is the report of migration of pain toward the midline of the spine with repeated maneuvers of the spine in flexion-extension or side bending. This pain pattern is thought to arise because of the central location of the disc, which is perceived as midline pain when stressed, compared to facet and SIJ pain, which tend to cause more lateral pain. The specificity of this test has been reported to range from 70% to 100% with a sensitivity of 64%.46–49 However, the time and training required for proper performance of this test limits its usefulness in most clinical settings and as a single physical examination maneuver; most experts agree that it is of low value and should be used together with diagnostic testing to make the diagnosis of discogenic pain. BVT involves applying a blunt electric vibrator over the spinous processes of the vertebrae. If the patient reports pain, it suggests discogenic LBP. The sensitivity and specificity of this test are controversial; studies are inconclusive because of questionable patient selection.50–52 Nonetheless, like the CP, it should be used together with the patient’s history and diagnostic testing to make the diagnosis of discogenic LBP.
Imaging and Discogenic Pain
Imaging studies used in evaluation of painful spinal disorders may include plain radiographs, nuclear medicine scans, magnetic resonance imaging (MRI), computed tomography (CT), myelography, CT myelography, and single-photon emission computed tomography (SPECT). Plain radiographs may help detect spinal instability, bony malalignment or deformity, and the presence of degenerative disease. Nuclear medicine scans are useful in detection of tumors, fractures, and infection. SPECT scans may play a limited role in identifying a subset of patients with facet disease.53
Before advances in MRI, myelography and CT with and without myelography were commonly used, although not without controversy, in diagnosis and management of disc protrusion, stenotic lesions, and other deformities of the spine.54–56 Currently, however, MRI is the first line imaging of choice for painful spinal disorders, thanks to its high degree of spatial resolution and the best soft tissue contrast of all the imaging modalities. All of these imaging studies have a high degree of PPV when radiculopathy, nerve root compression, and spinal deformities are the target diagnoses. However, when diagnosing the causes of axial spinal pain, these imaging modalities fail to provide a reasonable PPV; rather their greatest value is to rule out sinister pathology.3,57–60