Figure 16.1
Division of the gastrohepatic ligament (A caudate lobe, B right crus, C divided gastrohepatic ligament, D esophageal hiatus)
Figure 16.2
Esophageal mobilization from the abdomen. The upper picture demonstrates dissection along the pericardial plane anteriorly (A right crus, B pericardium, C distal esophagus) and the lower picture demonstrates dissection along the aortic plane posteriorly (D aortic plane, E left crus)

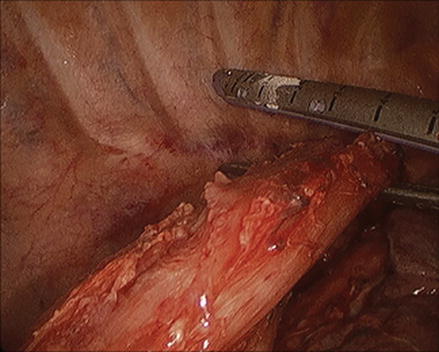
Figure 16.3
Right gastroepiploic arcade
Figure 16.4
Division of the left gastric pedicle (A left gastric pedicle, B divided left gastric pedicle, C esophageal hiatus)
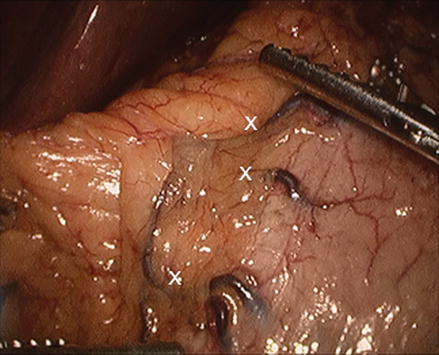
Figure 16.5
Branches of the right gastric artery along the lesser curve of the stomach
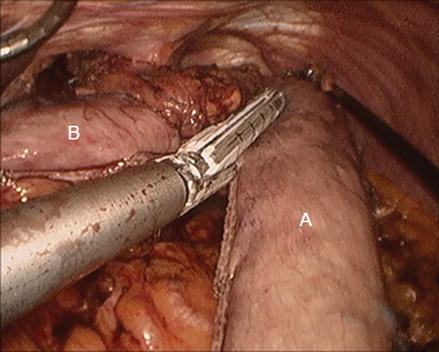
Figure 16.6
Creation of the gastric conduit (A gastric conduit, B specimen including proximal stomach and distal esophagus)
Figure 16.7
Laparoscopic jejunostomy tube placement. The upper picture demonstrates a loop of jejunum approximately 40 cm distal to the ligament of Treitz tacked up to the abdominal wall. A jejunostomy feeding tube is passed into the distal limb. The lower picture demonstrates completion of the jejunostomy tube with an anti-torsion stitch placed 3 cm from the tube entry site
Chest
A transthoracic approach is used for the Ivor Lewis, McKeown, and Minimally Invasive Esophagectomy (MIE) techniques. The basic principles for safe dissection are the same whether performed via thoracotomy, thoracoscopy or robotically. Esophageal mobilization and creation of an intrathoracic anastomosis is typically performed through the right chest. After the right lung has been isolated, the inferior pulmonary ligament is divided and the lung is retracted away. Esophageal mobilization is begun by opening the mediastinal pleura at the junction of the pleura and the lung, anterior to the esophagus, from the diaphragm proximally to the azygous vein. Periesophageal tissue is then swept off the avascular plane along the pericardium toward the esophagus (Fig. 16.8). Dissection is carried superiorly from the inferior pulmonary vein, keeping dissection on the posterior aspect of the pericardium, until the bronchus intermedius is encountered. The airway is then traced back to the right main stem bronchus and subcarinal lymph node packet, which is harvested en bloc. The left main stem bronchus should then come into view. Care must be taken to avoid excess use of energy in this area to minimize the risk of thermal injury to the airway; therefore bronchial arterial branches should be clipped and divided rather than cauterized. The vagus nerve is encountered as dissection is carried proximally, which is divided close the esophagus to avoid traction injury to the right recurrent laryngeal nerve (RLN). The azygous vein is divided as it crosses over the esophagus to empty into the superior vena cava (Fig. 16.9) to facilitate mobilization of the esophagus up to the thoracic inlet (Fig. 16.10). The mediastinal pleura overlying the posterior aspect of the esophagus is then opened from diaphragm to thoracic inlet. Posterior mobilization is carried out until the anterior/medial plane of dissection is met. Lymphatic and aortoesophageal branches along the posterior aspect of the esophagus should be clipped and divided. The posterior dissection should stay close to the esophagus to avoid injury to the main thoracic duct that lies within the fat posteriorly. Once the esophagus has been circumferentially mobilized, the conduit is retrieved from the abdomen and brought up into the chest. The esophagus is then transected proximal to the tumor to achieve appropriate margins. Intraoperative endoscopy may be performed to confirm the appropriate point of transection. The specimen is then removed and margins are checked by frozen section (Fig. 16.11). The esophagogastric intrathoracic anastomosis is then performed (discussed below). Drains and/or chest tubes are placed. If a cervical anastomosis is planned, the esophagus is not transected and only mobilization of the esophagus is carried out. The patient is then repositioned to perform the abdominal and cervical stages of the procedure.
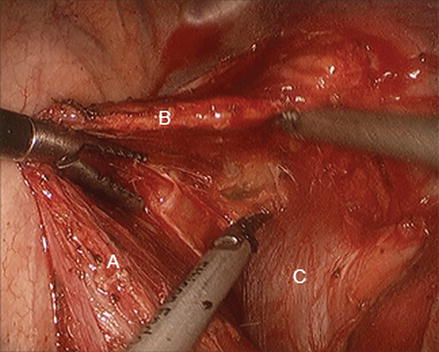
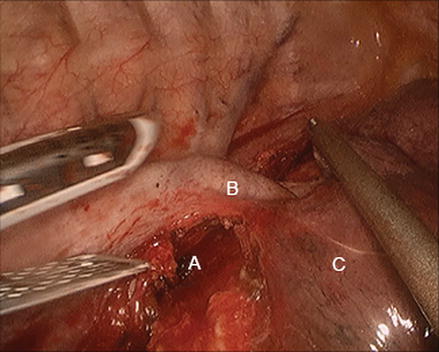
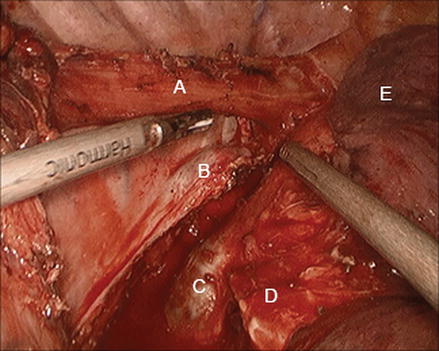
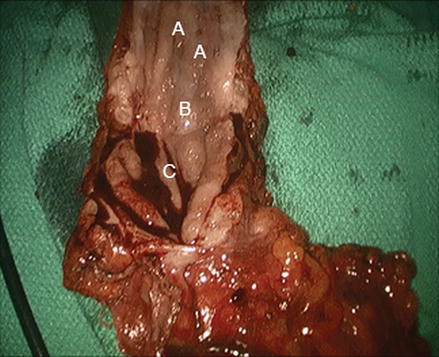
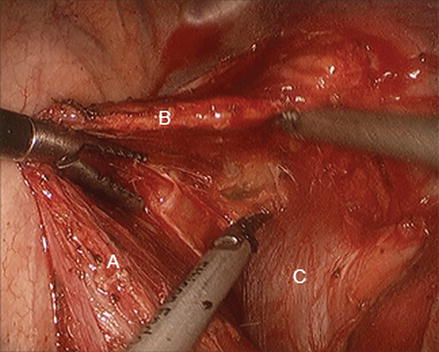
Figure 16.8
Mobilization of the intrathoracic esophagus along the pericardial plane (A esophagus, B periesophageal fat and lymph nodes, C pericardium)
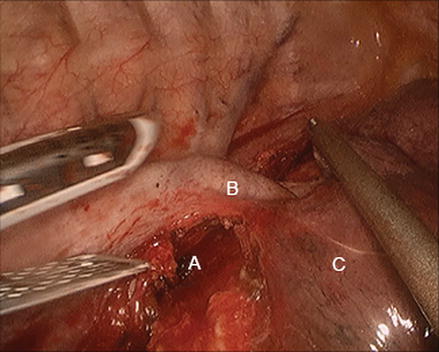
Figure 16.9
Division of the azygous vein as it arches over the esophagus (A esophagus, B azygous vein, C lung)
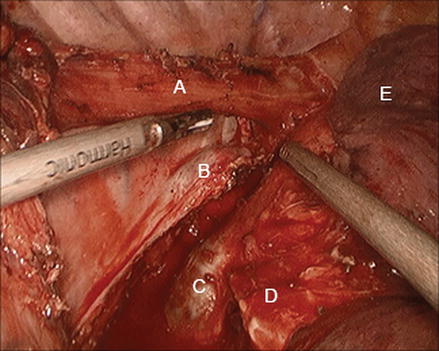
Figure 16.10
Mobilization of the intrathoracic esophagus up to the thoracic inlet (A esophagus, B divided azygous vein, C left main stem bronchus, D right main stem bronchus, E lung)
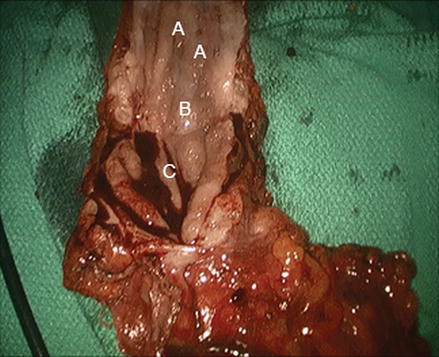
Figure 16.11
Esophagogastrectomy specimen opened on the back table to check gross margins prior to being sent for frozen section (A esophageal mucosa, B tumor, C gastric mucosa)
Neck
A cervical approach is used for the Transhiatal, Sweet, and McKeown techniques. The MIE may also be performed with a cervical anastomosis. The left neck is preferred because of the more reliable, vertical course of the left RLN and because the esophagus is slightly deviated to the left in the neck. Injury to the RLN occurs primarily by excessive traction or thermal injury from excessive electrocautery use. A 5–6 cm incision is made along the medial border of sternocleidomastoid muscle (SCM). The platysma is first divided and flaps are raised, followed by mobilization of the SCM laterally. Strap muscles are retracted medially. The anterior belly of the omohyoid muscle is typically divided. Dissection is continued medial to the internal jugular and carotid artery, retracting the vessels laterally with the SCM. The middle thyroid vein and inferior thyroid artery may be divided if needed for exposure. The thyroid and trachea are retracted medially and dissection is continued posteriorly down to the spine. The posterior aspect of the cervical esophagus is mobilized from the prevertebral fascia with blunt finger dissection until the esophagus can be hooked with the dissecting finger and retracted laterally into the wound (Fig. 16.12). The anterior aspect of the esophagus is carefully dissected away from the trachea, keeping dissection directly on the esophagus to avoid injury to the RLN in the tracheoesophageal groove. Circumferential mobilization of the esophagus is carried distally into the thoracic inlet until the distal plane of dissection performed from the chest or abdomen is met. The esophagus can then be transected and the specimen removed through the abdominal or neck wound. Once the conduit has been passed up from below, the anastomosis can then be created (discussed below). The neck is closed in layers and a closed suction drain is placed next to the anastomosis.
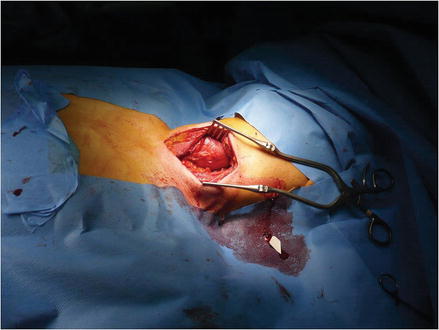
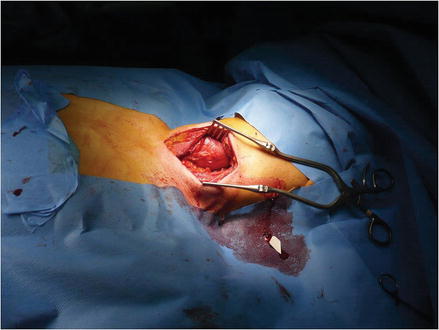
Figure 16.12
Left neck incision demonstrating exposure of the proximal esophagus
Esophagogastric Anastomosis
Numerous techniques have been described for creation of the esophagogastric anastomosis, including hand-sewn, stapled, and combined techniques. If the proximal extent of disease is above 25 cm, a cervical anastomosis is recommended to assure adequate margins. Either a cervical or intrathoracic anastomosis can be performed for disease distal to 25 cm. The gastric conduit must pull up easily into the neck or chest to reach the transected esophagus without tension. However, pulling up excessive conduit can result in a redundant conduit that empties poorly.
Hand-sewn Anastomosis
A hand-sewn technique may be used for either a cervical or intrathoracic anastomosis. Most favor a two-layered anastomosis when the hand-sewn technique is used. The tip of the gastric conduit is opened anteriorly approximately 2 cm from the stapled edge. Full-thickness corner stitches are placed at 3 and 9 o’clock to approximate the transected esophagus and gastrotomy. The anastomosis is then started with interrupted 3–0 or 4–0 absorbable suture, taking seromuscular bites on the stomach side and muscularis propria (longitudinal and circular layers) on the esophageal side to create the outer layer back row. The inner layer is then constructed by placing interrupted simple sutures around the entire circumference with full-thickness bites on the stomach side and only mucosa on the esophageal side. The anterior, outer layer is then performed to complete the anastomosis. The anastomosis may also be done with a continuous, running technique.
Linear Stapled Anastomosis
A side-to-side linear-stapled technique may also be used to create either a cervical or intrathoracic anastomosis. The conduit must have 4–5 cm of overlap with the proximal esophagus. A gastrotomy is made on the anterior aspect of the conduit, approximately 5 cm from the tip. The esophagus is transected with an oblique angle (anterior aspect left longer than the posterior). The esophagus is overlapped with the gastric conduit (esophagus anterior to the conduit). Stay sutures are placed at the anterior corner of the esophagus and another from the posterior corner of the esophagus to the superior corner of the gastrotomy. A 3 cm linear stapler is positioned with one jaw in the esophagus and the other in the conduit with the tip of the stapler directed cephalad, then fired. The remaining open portion is closed with two running full-thickness sutures followed by an outer interrupted, circumferential seromuscular layer.
EEA/End-to-Side Stapled Anastomosis
An end-to-side stapled technique may be used for creation of an intrathoracic anastomosis and is the authors’ favored technique [11]. The esophagus is divided at the desired level, typically superior to the divided azygous vein, with a linear stapler (Fig. 16.13). We prefer to use a 25-mm Orvil anvil (OrVil, Autosuture, Norwalk, CT, USA), which is a device that mounts the anvil on a 90-cm long polyvinyl chloride delivery tube. The delivery tube is passed transorally, similar to a nasogastric tube, and advanced into the remaining proximal esophagus. A small opening is made in the center of the staple line of the divided esophageal stump and the delivery tube is pulled distally until the anvil shaft protrudes through the esophagotomy and the anvil head is seated in the distal stump (Fig. 16.14). The delivery tube is detached by cutting the securing stich and the tube is removed. The gastric conduit is then pulled up further into the chest to assure that it will reach the proximal esophagus. The tip of the conduit is opened parallel to the staple line enough to allow the head of a 25-mm EEA stapler (EEA XL 25-mm with 4.8-mm staples, autosuture, Norwalk, CT, USA) to be inserted (Fig. 16.15). Once the stapler head has been inserted into the gastrotomy, the conduit is pulled onto the stapler for a few centimeters. It is important to avoid twisting of the conduit once the stapler head is inserted, keeping the staple line to the patient’s right (Fig. 16.15). The stapler pin is then brought out through the wall of the conduit opposite the staple line and docked with the anvil (Fig. 16.16). The stapler is fired after making sure surrounding tissue has been cleared. Once the stapler has been removed, two complete anastomotic rings (one from the esophagus side and the other from the gastric side) should be removed from the stapler. This creates an end (esophagus) to side (conduit) anastomosis, which avoids using the gastric conduit tip (which is usually slightly ischemic). The excess conduit is then resected with a linear stapler, making sure to avoid crossing of the staple lines (Fig. 16.17). The gastric conduit should appear well perfused and appropriately oriented with the staple line facing the surgeon (Fig. 16.18). Alternatively, the esophagus can be transected with scissors and a 25-mm or 28-mm EEA stapler anvil is placed into the esophagus and secured with two purse string sutures. All layers of the esophagus, including the mucosa, should be incorporated into the purse string. Once the anvil is secured, the end-to-side esophagogastric anastomosis is completed, as described above.