- •
Epidural block can be performed in cervical, thoracic, and lumbar regions of the vertebral column.
- •
Paramedian approach is the preferred technique for thoracic epidural, while median and paramedian approaches are suitable for lumbar epidural.
- •
T5–T6 interspace is the preferred position for thoracic epidural catheter insertion.
- •
The ligamentum flavum is congenitally absent in the midline in some people, which makes them prone to the dural puncture during epidural block.
- •
Checking for the coagulation status of the patients is very crucial before attempting the epidural block.
- •
Early diagnosis and management for epidural hematoma are crucial to avoid permanent neural damage.
Perspective
Epidural anesthesia is the second primary method of neuraxial block. In contrast to spinal anesthesia, epidural block requires pharmacologic doses of local anesthetics, making systemic toxicity a concern. In skilled hands, the incidence of postdural puncture headache should be lower with epidural anesthesia than with spinal anesthesia. Nevertheless, as outlined in Chapter 40 , Spinal Block, I do not believe this should be the major differentiating point between the two techniques. Spinal anesthesia is typically a single-shot technique, whereas frequently intermittent injections are given through an epidural catheter, thus allowing reinjection and prolongation of epidural block. Another difference is that epidural block allows production of segmental anesthesia. Thus if a thoracic injection is made and an appropriate amount of local anesthetic is injected, a band of anesthesia that does not block the lower extremities can be produced.
Patient Selection. Epidural block is appropriate for virtually the same patients who are candidates for spinal anesthesia, except that epidural anesthesia can be used in the cervical and thoracic areas as well—levels at which spinal anesthesia is not advised. As with spinal anesthesia, if epidural block is to be used for intraabdominal procedures involving the upper abdomen, it is advisable to combine this technique with a light general anesthetic because diaphragmatic irritation can make the patient, surgeon, and anesthesiologist uncomfortable. Other candidates for epidural anesthesia are patients in whom a continuous technique has increasingly been found to be helpful in providing epidural local anesthesia or opioid analgesia after major surgical procedures. This clinical application likely explains the increased interest in epidural block over the last 20 years.
Pharmacologic Choice. To use epidural local anesthetics effectively, one must combine an understanding of the potency and duration of local anesthetics with estimates of the length of the operation and the postoperative analgesia requirements. Drugs available for epidural use can be categorized as short-acting, intermediate-acting, and long-acting agents; with the addition of epinephrine to these agents, surgical anesthesia ranging from 45–240 minutes after a single injection is possible.
Chloroprocaine, an amino ester local anesthetic, is a short-acting agent that allows efficient matching of the length of the surgical procedure and the duration of epidural analgesia, even in outpatients. 2-Chloroprocaine is available in 2% and 3% concentrations; the latter is preferable for surgical anesthesia and the former for techniques not requiring muscle relaxation.
Lidocaine is the prototypical amino amide local anesthetic and is used in 1.5% and 2% concentrations epidurally. Concentrations of mepivacaine necessary for epidural anesthesia are similar to those of lidocaine; however, mepivacaine lasts from 15–30 minutes longer at equivalent dosages. Epinephrine significantly prolongs (i.e., by approximately 50%) the duration of surgical anesthesia with 2-chloroprocaine and either lidocaine and mepivacaine. Plain lidocaine produces surgical anesthesia that lasts from 60–100 minutes.
Bupivacaine, an amino amide, is a widely used long-acting local anesthetic for epidural anesthesia. It is used in 0.5% and 0.75% concentrations, but analgesic techniques can be performed with concentrations ranging from 0.125%–0.25%. Its duration of action is not prolonged as consistently by the addition of epinephrine, although up to 240 minutes of surgical anesthesia can be obtained when epinephrine is added.
Ropivacaine, another long-acting amino amide, is also used for regional and epidural anesthesia. For surgical anesthesia, it is used in 0.5%, 0.75%, and 1% concentrations. Analgesia can be obtained with concentrations of 0.2%. Its duration of action is slightly less than that of bupivacaine in the epidural technique, and it appears to produce slightly less motor blockade than a comparable concentration of bupivacaine.
In addition to the use of epinephrine as an epidural additive, some anesthesiologists recommend modifying epidural local anesthetic solutions to increase both the speed of onset and the quality of the block produced. One recommendation is to alkalinize the local anesthetic solution by adding bicarbonate to it to achieve both these purposes. Nevertheless, the clinical advisability of routinely adding bicarbonate to local anesthetic solutions should be determined by local practice protocols.
Placement
Anatomy. As with spinal anesthesia, the key to carrying out successful epidural anesthesia is understanding the three-dimensional midline neuraxial anatomy that underlies the palpating fingers ( Fig. 41.1 ). When a lumbar approach to the epidural space is used in adults, the depth from the skin to the ligamentum flavum is commonly near 4 cm; in 80% of patients the epidural space is cannulated at a distance of 3.5–6 cm from the skin. In a small number of patients the lumbar epidural space is as near as 2 cm from the skin. In the lumbar region, the ligamentum flavum is 5–6 mm thick in the midline, whereas in the thoracic region it is 3–5 mm thick. In the thoracic region, the depth from the skin to the epidural space depends on the degree of cephalad angulation used for the paramedian approach, as well as the body habitus of the patient ( Fig. 41.2 ). In the cervical region the depth to the ligamentum flavum is approximately the same as that in the lumbar region, 4–6 cm.

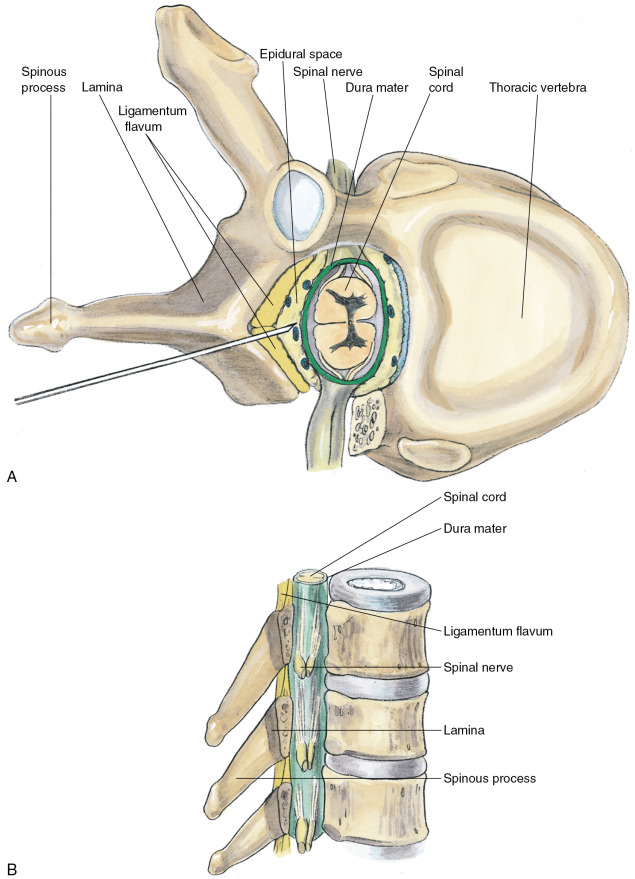
The ligamentum flavum will be perceived as a thicker ligament if the needle is kept in the midline than if the needle is inserted off the midline and enters the lateral extension of the ligamentum flavum. Fig. 41.3 illustrates how important it is to maintain the midline position of the epidural needle ( needle A ) during lumbar epidural techniques. If an oblique approach is taken, a “false release” can be produced (needle C) or the perception of a thin ligament can be reinforced (needle B) .

Position. Patient positioning for epidural anesthesia is similar to that for spinal anesthesia, with lateral decubitus, sitting, and prone jackknife positions all applicable. The lateral decubitus position is applicable for both lumbar and thoracic epidural techniques, and the sitting position allows the administration of lumbar, thoracic, and cervical epidural anesthetics. The prone jackknife position allows access to the caudal epidural space.
Needle Puncture: Lumbar Epidural. A technique similar to that used for spinal anesthesia should be carried out to identify the midline structures; and the bony landmarks should be used to determine the vertebral level appropriate for needle insertion ( Fig. 41.4 ). When choosing a needle for epidural anesthesia, one must decide whether a continuous or single-shot technique is desired. This is the principal determinant of needle selection. If a single-shot epidural technique is chosen, a Crawford needle is appropriate; if a continuous catheter technique is indicated, a Tuohy or other needle with a lateral-facing opening is chosen.











