CHAPTER 79
Epididymitis
Presentation
A male child, adolescent, or adult complains of dull to moderately severe unilateral scrotal pain developing gradually over a period of hours to days and possibly radiating to the ipsilateral lower abdomen or flank. In adult or adolescent males, there may be a history of recent urinary tract infection, urethritis, prostatitis, or prostatectomy (allowing ingress of bacteria), strain from lifting a heavy object, or sexual activity with a full bladder (allowing reflux of urine). Foley catheter drainage, intermittent catheterization, and other forms of urinary tract instrumentation predispose to infection and epididymitis. Drugs, such as amiodarone, also may cause epididymitis (chemical epididymitis), which affects the head of the epididymis only. There may be fever or urinary urgency or frequency. Nausea is unusual.
The epididymis is tender, swollen, warm, and difficult to separate from the firm, nontender testicle. Over time, increasing inflammation can extend up the spermatic cord and fill the entire scrotum, making examinations more difficult, with testicular tenderness, as well as producing frank prostatitis or cystitis. The rectal examination, therefore, may reveal a very tender, boggy prostate.
What To Do:
 The first priority is to rule out the possibility of testicular torsion. Key details to elicit on initial history include the onset and duration of the symptoms, including any previous such episodes. Testis torsion typically begins suddenly over a matter of minutes with intense pain, whereas epididymitis typically has a more gradual onset over a period of hours to days with more moderate pain. Associated symptoms, such as nausea and vomiting, seem to be more specific for torsion, whereas dysuria, urgency, and frequency point to an infectious or inflammatory cause, such as epididymitis.
The first priority is to rule out the possibility of testicular torsion. Key details to elicit on initial history include the onset and duration of the symptoms, including any previous such episodes. Testis torsion typically begins suddenly over a matter of minutes with intense pain, whereas epididymitis typically has a more gradual onset over a period of hours to days with more moderate pain. Associated symptoms, such as nausea and vomiting, seem to be more specific for torsion, whereas dysuria, urgency, and frequency point to an infectious or inflammatory cause, such as epididymitis.
 The age of the patient may also be helpful in the diagnosis, because testis torsion has a bimodal distribution, with peak incidence in early childhood and preadolescence. The incidence of acute epididymitis increases sharply during adolescence, correlating with increased sexual activity.
The age of the patient may also be helpful in the diagnosis, because testis torsion has a bimodal distribution, with peak incidence in early childhood and preadolescence. The incidence of acute epididymitis increases sharply during adolescence, correlating with increased sexual activity.
 The scrotum and its contents should be inspected and palpated. Patients with epididymitis typically appear more comfortable than those with torsion. The position, axis, and lie of the testis should all be documented. A torsed testis is typically enlarged (because of venous congestion) and lies high within the scrotum and may have rotated transversely, giving its axis a more horizontal appearance (Figure 79-1). Conversely, the testis has a normal lie and axis in acute epididymitis. After 24 hours, the scrotal appearance of testicular torsion may be identical to that of epididymitis.
The scrotum and its contents should be inspected and palpated. Patients with epididymitis typically appear more comfortable than those with torsion. The position, axis, and lie of the testis should all be documented. A torsed testis is typically enlarged (because of venous congestion) and lies high within the scrotum and may have rotated transversely, giving its axis a more horizontal appearance (Figure 79-1). Conversely, the testis has a normal lie and axis in acute epididymitis. After 24 hours, the scrotal appearance of testicular torsion may be identical to that of epididymitis.
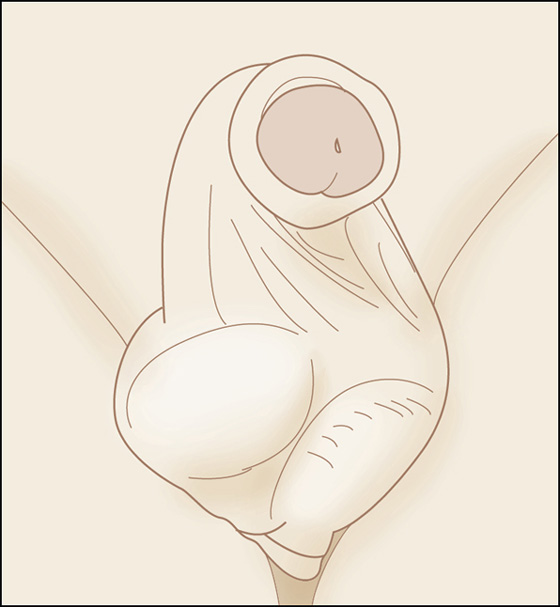
Figure 79-1 The acute scrotum with testicular torsion. Note the horizontal lie and elevated position of the right testis. (Adapted from Rosenstein D, McAninch JW: Urologic emergencies. Med Clin North Am 88:495-518, 2004.)
 Before palpation of the testicles, the cremasteric reflex should be assessed, beginning with the unaffected side. This reflex is elicited by lightly stroking the superomedial aspect of the thigh, causing brisk testicular retraction. Absence of the cremasteric reflex is highly sensitive for testis torsion.
Before palpation of the testicles, the cremasteric reflex should be assessed, beginning with the unaffected side. This reflex is elicited by lightly stroking the superomedial aspect of the thigh, causing brisk testicular retraction. Absence of the cremasteric reflex is highly sensitive for testis torsion.
 The testis and spermatic cord should next be gently palpated. A torsed testis is diffusely tender, whereas in acute epididymitis, the pain may be localized to the head of the epididymis and the superior pole of the testis.
The testis and spermatic cord should next be gently palpated. A torsed testis is diffusely tender, whereas in acute epididymitis, the pain may be localized to the head of the epididymis and the superior pole of the testis.
 Laboratory evaluation in acute scrotal pain should include obtaining a midstream urinalysis, Gram stain, and urine culture. Presence of pyuria or bacteriuria suggests epididymitis but does not confirm the diagnosis or rule out testicular torsion.
Laboratory evaluation in acute scrotal pain should include obtaining a midstream urinalysis, Gram stain, and urine culture. Presence of pyuria or bacteriuria suggests epididymitis but does not confirm the diagnosis or rule out testicular torsion.
 All patients suspected of epididymitis should have an appropriate specimen analyzed for gonococcal and nongonococcal urethritis. Culture, nucleic acid hybridization tests, and nucleic acid amplification tests (NAATs) are available. Culture and nucleic acid hybridization tests require a urethral swab, whereas NAATs can be performed on a urine sample.
All patients suspected of epididymitis should have an appropriate specimen analyzed for gonococcal and nongonococcal urethritis. Culture, nucleic acid hybridization tests, and nucleic acid amplification tests (NAATs) are available. Culture and nucleic acid hybridization tests require a urethral swab, whereas NAATs can be performed on a urine sample.
 If the clinical diagnosis strongly suggests testis torsion, there should be no delay in obtaining further testing. Urologic consultation should be obtained immediately to provide expeditious surgical exploration. Cooling of the affected testicle with an ice pack while awaiting surgery may decrease the ischemic insult. Manual reduction of a torsed testis can be attempted with or without narcotic analgesia. Successful detorsion alleviates acute symptoms and may obviate emergent exploration; however, it is not a definitive treatment. Testes usually, but not always, torse in an inward direction. Manual detorsion should proceed with turning the testicle in an outward direction (as in “opening a book”) or in the direction that the clinician would supinate his hands when approaching the patient from the feet. With successful detorsion, there will be release and elongation of the cord, followed by a marked diminution in symptoms. If pain increases or the spermatic cord shortens, stop and attempt the maneuver in the reverse direction. As mentioned, successful manual reduction is not a definitive treatment and should soon be followed by elective orchidopexy.
If the clinical diagnosis strongly suggests testis torsion, there should be no delay in obtaining further testing. Urologic consultation should be obtained immediately to provide expeditious surgical exploration. Cooling of the affected testicle with an ice pack while awaiting surgery may decrease the ischemic insult. Manual reduction of a torsed testis can be attempted with or without narcotic analgesia. Successful detorsion alleviates acute symptoms and may obviate emergent exploration; however, it is not a definitive treatment. Testes usually, but not always, torse in an inward direction. Manual detorsion should proceed with turning the testicle in an outward direction (as in “opening a book”) or in the direction that the clinician would supinate his hands when approaching the patient from the feet. With successful detorsion, there will be release and elongation of the cord, followed by a marked diminution in symptoms. If pain increases or the spermatic cord shortens, stop and attempt the maneuver in the reverse direction. As mentioned, successful manual reduction is not a definitive treatment and should soon be followed by elective orchidopexy.
 If the testis has a normal lie, the epididymis is tender, and there is a positive cremasteric reflex, the most likely diagnosis is epididymitis. Testicular torsion is doubtful, and no further workup is indicated.
If the testis has a normal lie, the epididymis is tender, and there is a positive cremasteric reflex, the most likely diagnosis is epididymitis. Testicular torsion is doubtful, and no further workup is indicated.
 Patients may be treated with narcotic analgesics if needed (nonsteroidal anti-inflammatory drugs [NSAIDs] if not contraindicated) and antibiotics.
Patients may be treated with narcotic analgesics if needed (nonsteroidal anti-inflammatory drugs [NSAIDs] if not contraindicated) and antibiotics.
 Most pediatric urologists recommend amoxicillin or trimethoprim-sulfamethoxazole for the prepubertal male with epididymitis, even though the urine is usually sterile.
Most pediatric urologists recommend amoxicillin or trimethoprim-sulfamethoxazole for the prepubertal male with epididymitis, even though the urine is usually sterile.
 The sexually active male adolescent to 35-year-old should be treated for a presumed sexually transmitted disease. Prescribe ceftriaxone (Rocephin), 250 mg IM, in the clinic or emergency department, and a prescription for doxycycline (Vibramycin), 100 mg bid for 10 days, should eradicate Neisseria gonorrhoeae and Chlamydia trachomatis. An alternative treatment is ofloxacin (Floxin), 300 mg bid for 10 days.
The sexually active male adolescent to 35-year-old should be treated for a presumed sexually transmitted disease. Prescribe ceftriaxone (Rocephin), 250 mg IM, in the clinic or emergency department, and a prescription for doxycycline (Vibramycin), 100 mg bid for 10 days, should eradicate Neisseria gonorrhoeae and Chlamydia trachomatis. An alternative treatment is ofloxacin (Floxin), 300 mg bid for 10 days.
 In men older than 35 years of age who have suspected of epididymitis from enteric organisms, use levofloxacin (Levaquin), 500 mg qd for 10 days, or Ofloxacin, 300 mg bid for 10 days.
In men older than 35 years of age who have suspected of epididymitis from enteric organisms, use levofloxacin (Levaquin), 500 mg qd for 10 days, or Ofloxacin, 300 mg bid for 10 days.
 Epididymitis secondary to chronic use of amiodarone responds only to discontinuation or reduction of dosage.
Epididymitis secondary to chronic use of amiodarone responds only to discontinuation or reduction of dosage.
 Arrange for 2 to 3 days of strict bed rest with the scrotum elevated. The patient should use an athletic supporter when up, soak in warm tub baths, and obtain urologic follow-up within several days. For the first 72 hours, ice compresses may be helpful.
Arrange for 2 to 3 days of strict bed rest with the scrotum elevated. The patient should use an athletic supporter when up, soak in warm tub baths, and obtain urologic follow-up within several days. For the first 72 hours, ice compresses may be helpful.
 Always warn patients or parents of the possibility of intermittent torsion and the need to return immediately if severe or worsening pain develops.
Always warn patients or parents of the possibility of intermittent torsion and the need to return immediately if severe or worsening pain develops.
 All prepubertal males with confirmed epididymitis should have close follow-up and consideration for referral to a pediatric urologist because of the high incidence of an underlying anatomic abnormality.
All prepubertal males with confirmed epididymitis should have close follow-up and consideration for referral to a pediatric urologist because of the high incidence of an underlying anatomic abnormality.
 If there is any doubt about the diagnosis because of an atypical history and/or indistinct physical findings, perform an emergent testicular color Doppler ultrasound study. Epididymitis will show a normal or increased blood flow to the testis and epididymis, whereas torsion will show low or no flow.
If there is any doubt about the diagnosis because of an atypical history and/or indistinct physical findings, perform an emergent testicular color Doppler ultrasound study. Epididymitis will show a normal or increased blood flow to the testis and epididymis, whereas torsion will show low or no flow.
 One needs to keep in mind that the testicle may spontaneously detorse before ultrasonography is performed, yielding a normal study or one with postischemic increased flow in a patient still at risk for further episodes of torsion. When the study is nondiagnostic, urologic consultation is required. Unless you are absolutely certain that your patient does not have testicular torsion, you must insist that the urologist see him as soon as possible.
One needs to keep in mind that the testicle may spontaneously detorse before ultrasonography is performed, yielding a normal study or one with postischemic increased flow in a patient still at risk for further episodes of torsion. When the study is nondiagnostic, urologic consultation is required. Unless you are absolutely certain that your patient does not have testicular torsion, you must insist that the urologist see him as soon as possible.
 If the patient is toxic and febrile, have the patient admitted, give antibiotics intravenously, and suspect testicular and/or epididymal abscess.
If the patient is toxic and febrile, have the patient admitted, give antibiotics intravenously, and suspect testicular and/or epididymal abscess.
What Not To Do:
 Do not miss testicular torsion. It is far better to have the urologist explore the scrotum and find epididymitis than to delay and lose a testicle to ischemia (which can happen in only 4 to 6 hours). Half of symptomatic males describe previous similar transient episodes of scrotal pain, consistent with intermittent torsion/detorsion. When torsion is strongly suspected, do not delay the management of the case by waiting for the results of ancillary tests.
Do not miss testicular torsion. It is far better to have the urologist explore the scrotum and find epididymitis than to delay and lose a testicle to ischemia (which can happen in only 4 to 6 hours). Half of symptomatic males describe previous similar transient episodes of scrotal pain, consistent with intermittent torsion/detorsion. When torsion is strongly suspected, do not delay the management of the case by waiting for the results of ancillary tests.
 Do not perform an incomplete manual detorsion of a testicle with a twist greater than or equal to 720 degrees. Partial detorsion may relieve symptoms and improve the examination but not relieve the ischemia. Continue to rotate the testicle one to three turns until the patient is pain free with a normal testicular lie.
Do not perform an incomplete manual detorsion of a testicle with a twist greater than or equal to 720 degrees. Partial detorsion may relieve symptoms and improve the examination but not relieve the ischemia. Continue to rotate the testicle one to three turns until the patient is pain free with a normal testicular lie.
 Do not overlook the testicular examination in any male with abdominal pain. In some instances of testicular torsion, a gradual onset of testicular and abdominal pain is the primary complaint.
Do not overlook the testicular examination in any male with abdominal pain. In some instances of testicular torsion, a gradual onset of testicular and abdominal pain is the primary complaint.
 Do not rely on white blood cell counts and urinalysis to help make the diagnosis of acute epididymitis. Although a urinalysis should be performed in all patients with suspected epididymitis, most patients with epididymitis have normal urinalysis.
Do not rely on white blood cell counts and urinalysis to help make the diagnosis of acute epididymitis. Although a urinalysis should be performed in all patients with suspected epididymitis, most patients with epididymitis have normal urinalysis.
Discussion
Epididymitis is the most common cause of acute scrotum in adolescent boys and adults. Sexually transmitted C. trachomatis and N. gonorrhoeae are common pathogens in men younger than 35 years. In prepubertal boys and men older than 35 years of age, the disease is most frequently caused by Escherichia coli and Proteus mirabilis.
Prehn described the clinical differentiation of scrotal pain associated with epididymitis and acute torsion. Pain is relieved when the testicles are elevated over the symphysis pubis in epididymitis, but the scrotal pain associated with testicular torsion is not lessened with this maneuver (the Prehn sign). Unfortunately, although a positive sign supports the diagnosis of epididymitis, it in no way excludes the diagnosis of torsion.
Epididymitis first affects the tail of the epididymis and then spreads to involve its body and head. Orchitis develops in 20% to 40% of cases by direct spread of infection, thereby leading to testicular swelling and tenderness similar to that seen with testicular torsion.
Unlike testicular torsion, torsion of an appendage testis is a self-resolving, benign process and is usually much less painful than epididymitis or testicular torsion, but it is often confused with these two entities. Although appendices can be found on the testicle, epididymis, or spermatic cord, it is usually the appendix found on the testicle (appendix testis) that is prone to torsion.
The most important aspect of the physical examination is pain and tenderness localized to the region of the appendix testis (usually superior lateral testis). Every attempt should be made to have the patient localize the pain. If only a part of the testis is tender, testicular torsion is doubtful. If the epididymis is not tender, epididymitis is also doubtful. The classic “blue dot sign” of an infarcted appendage may be seen through thin scrotal skin if there is a minimal amount of edema and erythema. These cases are managed conservatively, with attention given to pain management. The pain usually resolves in 2 to 3 days with atrophy of the appendix that may calcify. The role of sonographic examination in torsion of the testicular appendages is to exclude testicular torsion.
Testicular torsion causes venous engorgement that results in edema, hemorrhage, and subsequent arterial compromise, which results in testicular ischemia. The extent of testicular ischemia depends on the degree of torsion, which ranges from 180 degrees to 720 degrees or more. Experimental studies indicate that 720-degree torsion is required to occlude the testicular artery. When torsion is 180 degrees or less, diminished flow is seen. The testicular salvage rate depends on the degree of torsion and the duration of ischemia. A nearly 100% salvage rate exists within the first 6 hours after onset of symptoms, a 70% rate within 6 to 12 hours, and a 20% rate within 12 to 24 hours.
The role of color Doppler and power Doppler sonography in the diagnosis of acute testicular torsion is well established. Torsion may be complete, incomplete, or transient. Cases that show partial or transient torsion present a diagnostic challenge. The ability of color Doppler imaging to diagnose incomplete torsion accurately remains undetermined. The presence of a color or power Doppler signal in a patient with the clinical presentation of torsion does not exclude torsion. Testicular imaging studies have a 10% to 15% false-negative rate.
Because of overlapping symptoms, historical findings may be of little use in differentiating epididymitis, testicular torsion, and torsion appendix testis. Physical examination findings are helpful. Patients with testicular torsion are much more likely to have a tender testicle, an abnormal testicular lie, and/or an absent cremasteric reflex when compared with patients with epididymitis. The presence of the cremasteric reflex is the most valuable clinical finding in ruling out testicular torsion. Color Doppler ultrasonography is extremely helpful in diagnosing the etiology of an acute scrotum, although, at times, diagnostic surgical exploration will be required for making a definitive diagnosis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


