Chapter 30 Envenomation
Australia is home to many venomous creatures. Australian animals that are important in causing envenoming in humans include snakes, spiders, octopuses, fish and other marine creatures. The distribution of venomous creatures is wide, and each region has its own pattern of envenomation. Local knowledge is very important and local expert knowledge can be invaluable.
SNAKEBITE
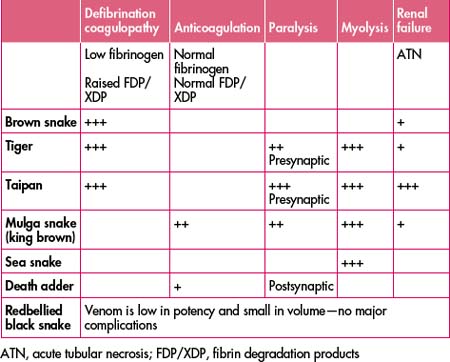
Australia is home to a number of the most venomous snakes in the world. Snake venom is a complex mixture of substances. Australian snakes produce venoms that have a range of clinical effects including neurotoxic (presenting as progressive paralysis), myotoxic (causing rhabdomyolysis and subsequent renal failure) or severe coagulation disturbances and haemolysis (Table 30.1).
First aid: the pressure-immobilisation technnique
Snake venom spreads via the lymphatics. The pressure-immobilisation method of first aid prevents spread of the venom via the lymphatics and can prevent clinical envenomation. It involves applying a firm broad bandage, commencing at the site of the bite, and then applying the bandage over the entire limb, extending both proximally and distally. The pressure is the same as that used for a sprained ankle. A splint is then applied to the limb, to immobilise the limb and reduce muscle contraction to further reduce lymphatic spread of the venom. The patient is then kept as still as possible and transported to hospital.
If a patient arrives with symptoms of envenomation and does not have a bandage applied, then one should be applied.
Table 30.2 Use of the pressure-immobilisation technique of first aid
| Pressure-immobilisation is recommended for | Do not use pressure-immobilisation first aid for |
|---|---|
| All Australian venomous snake bites, including sea snake bites | Redback spider bites |
| Funnel web spider bites | Other spider bites, including mouse spiders, white tailed spiders |
| Box jellyfish stings (if possible) | Bluebottle jellyfish stings |
| Bee, wasp and ant stings in allergic individuals | Other jellyfish stings |
| Blue-ringed octopus bites | Stonefish and other fish stings |
| Cone snail (cone shell) stings | Bee and wasp stings in non-allergic individuals |
| Australian paralysis tick envenomation | Bites or stings by scorpions, centipedes, beetles |
Adapted with permission of the Australian Venom Research Unit
Venom detection kit
The venom detection kit is used by trained laboratory staff and takes about 20 minutes to complete.
Antivenom
Antivenom is the definitive treatment for a patient with systemic envenomation. The administration of antivenom can reverse the clinical effects of envenomation. The treatment of envenomation following snakebite involves the administration of adequate quantities of the appropriate antivenom.