Chapter 11 ENT problems
Introduction
The vast majority of ENT (ear, nose and throat) problems that present in the pre-hospital setting are minor in nature. However, occasionally innocuous symptoms can develop into life-threatening conditions which require immediate assessment and treatment. The objectives of this chapter are outlined in Box 11.1.
Box 11.1 Chapter objectives
 To identify any patients who have a normal primary survey but have an obvious need for hospital admission
To identify any patients who have a normal primary survey but have an obvious need for hospital admission To undertake a secondary survey (full assessment) including history and examination targeted to the presenting symptom
To undertake a secondary survey (full assessment) including history and examination targeted to the presenting symptom Discuss treatment based on the likely diagnosis(es) and whether home management or hospital admission is appropriate
Discuss treatment based on the likely diagnosis(es) and whether home management or hospital admission is appropriatePrimary survey
The primary survey (Box 11.2) is a rapid assessment tool which uses the ABC principles to look for an immediately life-threatening condition.
Box 11.2 Primary survey
If any observations below are present treat immediately and transfer to hospital:
ENT conditions can be immediately life-threatening by causing an A, B or C problem:
 A Airway obstruction/compromise – inhaled foreign body, epiglottitis, quinsy, anaphylaxis/angio-oedema, croup, facial fractures
A Airway obstruction/compromise – inhaled foreign body, epiglottitis, quinsy, anaphylaxis/angio-oedema, croup, facial fractures C Circulatory compromise – haemorrhage, e.g. epistaxis, from facial fracture, secondary haemorrhage following ENT surgery, e.g. post-tonsillectomy.
C Circulatory compromise – haemorrhage, e.g. epistaxis, from facial fracture, secondary haemorrhage following ENT surgery, e.g. post-tonsillectomy.Patients with a normal primary survey but with obvious need for hospital admission
Patients with all of the above conditions can show a spectrum of severity of symptoms and signs, which can deteriorate. It is essential to remember that in the early stages of these conditions, patients may not have significant abnormal physical signs. The recognition of developing airway obstruction is critical and management of the condition may require the use of airway adjuncts to maintain adequate oxygenation. If there is complete airway obstruction and airway adjuncts have failed, prompt insertion of a surgical airway may be required as a last resort. It is important to monitor patients with respiratory distress for deterioration and exhaustion. In the case of haemorrhage the body will initially compensate. Therefore cases leading to hypovolaemia should be treated by arresting the haemorrhage and administering fluid to maintain a radial pulse.
should be admitted to hospital for further investigation and management. However, not all cases of croup or epistaxis will require hospital admission. Management of the individual conditions is discussed below or in other chapters of this book.
Secondary survey
Patients still remaining after the primary survey require a thorough assessment to determine optimal treatment and discharge (see Chapter 2).
 History and examination. Should be targeted to the presenting symptom and associated systems. Examination of the respiratory and cardiovascular systems is always necessary. This should be supplemented with abdominal assessment when glandular fever is suspected, looking for hepatosplenomegaly, and examination of the central nervous system if vertigo or facial weakness is the presenting symptom.
History and examination. Should be targeted to the presenting symptom and associated systems. Examination of the respiratory and cardiovascular systems is always necessary. This should be supplemented with abdominal assessment when glandular fever is suspected, looking for hepatosplenomegaly, and examination of the central nervous system if vertigo or facial weakness is the presenting symptom. Vital signs. Unless you are transporting the patient immediately, then always measure a full set of vital signs.
Vital signs. Unless you are transporting the patient immediately, then always measure a full set of vital signs.Differential diagnosis
Table 11.1 shows details of the differential diagnoses classified by presenting symptom.
Table 11.1 Differential diagnoses classified by presenting symptom
| Presenting symptom | ENT diagnoses | Other differential diagnoses |
|---|---|---|
| Nose bleed | Anterior bleed Posterior bleed Traumatic Post surgery | Underlying bleeding disorder |
| Sore throat | Tonsillitis Pharyngitis Glandular fever Candida Quinsy Stevens–Johnson syndrome Ramsey–Hunt syndrome | Angina Gastro-oesophageal reflux Tobacco usage Occupational irritants |
| Sore ears | Otitis externa Viral otitis media Bacterial otitis media Perforated tympanic membrane Eustachian tube dysfunction Mastoiditis Ramsey–Hunt syndrome | Temporomandibular joint dysfunction Upper GI and airway neoplasms Dental Cervical spondylosis |
| Foreign body | Ears Nose Airway | |
| Difficult/noisy breathing | Foreign body Epiglottitis Croup Anaphylaxis Bacterial tracheitis Smoke inhalation | Asthma COPD |
| Vertigo | Vestibular neuronitis Meniere’s Benign paroxysmal positional vertigo | Cerebellar CVA Other central causes |
| Facial/tooth pain | Sinusitis Dental abscess | Shingles Trigeminal neuralgia |
| Facial weakness | Bells palsy Ramsey–Hunt syndrome | CVA |
| Sudden hearing loss | Wax impaction Perforated TM | CVA |
| Trauma | Facial fractures Perforated TM |
Presenting symptoms, history, examination and treatment
Nose bleed
The following points in the history are important for the management of a patient with a nose bleed:
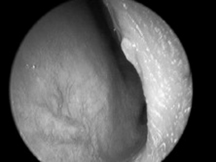
When examining the patient try to locate the side of the bleeding, look at the linearity of the nose (if asymmetrical, is this due to recent trauma?); check the appearance of the septum and Little’s area. The latter is the area of the septum seen through the nostrils when the nasal tip is tilted upwards (Fig. 11.1). Blood vessels in Little’s area are prone to bleeding. Check the throat for blood running down the nasopharynx. Ensure you get a set of vital signs and examine the cardiovascular system looking for any indication of shock.
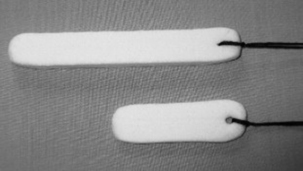
If the bleeding fails to respond to simple first aid measures packing should be applied to the nasal cavity from which the bleed is suspected to have originated. The simplest pack and the easiest to insert is the nasal tampon (Fig. 11.2). However, the nose can be packed with ribbon gauze if available and the healthcare professional is competent at the procedure. Nasal tampons are supplied small and flat but expand and take on the contours of the cavity when they are hydrated with either blood or saline. The leading edge of the nasal tampon should be lubricated prior to insertion. It should then be inserted in a horizontal plane into the nasal cavity. If the nasal tampon does not expand with the blood in the nose, saline should be dripped onto the external end of the nasal tampon until it expands and causes compression. The thread of the tampon should be secured with tape and a nasal sling may be applied to soak up any excess blood.
If anterior packing fails to stop the bleeding after 15 minutes a posterior bleed should be suspected (approx. 5% of bleeds). These require packing using a long nasal tampon, an epistaxis balloon or a Foley catheter with an anterior pack depending on what is available (Fig. 11.3). Long (posterior) nasal tampons are inserted in the same way as an anterior tampon. Some epistaxis balloons have an anterior and posterior balloon. The balloon is lubricated with saline and inserted, again in a horizontal plane. The posterior balloon is inflated to the recommended volume, gentle traction is applied to position the balloon in the posterior nasal space and then the anterior balloon is inflated to the recommended volume. Foley catheters and single balloon epistaxis catheters are inserted in the same way but do not have an anterior balloon and therefore an anterior pack is necessary. The Foley catheter must be secured with care taken to prevent pressure necrosis of the nasal tissues. All patients with a posterior bleed require admission (Box 11.3). If a large volume of blood has been lost, oxygen, venous access and fluid resuscitation may be necessary.
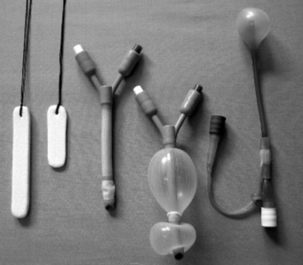
Fig. 11.3 Posterior and anterior nasal tampons, deflated and inflated double balloon epistaxis catheters and single posterior space epistaxis balloon catheter (reproduced with permission of BASICS Scotland).
Box 11.3 Patients with a nose bleed – who needs to go to hospital?
 All patients with a posterior pack must be admitted to hospital. They require analgesia and close monitoring particularly of vital signs and O2 saturations
All patients with a posterior pack must be admitted to hospital. They require analgesia and close monitoring particularly of vital signs and O2 saturations Patients with a history of recent nasal surgery should be discussed with the appropriate surgical team
Patients with a history of recent nasal surgery should be discussed with the appropriate surgical team Patients taking anticoagulants may be treated in the community if a recent INR is known and over-anticoagulation is not suspected
Patients taking anticoagulants may be treated in the community if a recent INR is known and over-anticoagulation is not suspected Patients with an anterior pack and significant other medical illness such as angina or COPD should be considered for admission for close monitoring depending on severity of co-morbid conditions. By packing the patient’s nose we cause respiratory compromise that may lead to exacerbations of pre-existing illnesses
Patients with an anterior pack and significant other medical illness such as angina or COPD should be considered for admission for close monitoring depending on severity of co-morbid conditions. By packing the patient’s nose we cause respiratory compromise that may lead to exacerbations of pre-existing illnesses