Links: Acute | Chronic | Bronchiectasis |
 Respiratory Bronchiolitis: associated with ILD, occurs exclusively in smokers, usually age 30-40yo. Presents with bibasilar rales, CXR with a bilateral reticulonodular interstitial infiltrate, usually basilar. Dx with open lung bx (Clin Chest Med 200;21:1).
Respiratory Bronchiolitis: associated with ILD, occurs exclusively in smokers, usually age 30-40yo. Presents with bibasilar rales, CXR with a bilateral reticulonodular interstitial infiltrate, usually basilar. Dx with open lung bx (Clin Chest Med 200;21:1).
Etiology: Acute bronchitis is largely due to viral pathogens and is less frequently caused by Mycoplasma pneumoniae and Chlamydophila pneumoniae. Bordetella pertussis should be considered in an adolescent or young adult with prominent cough. Direct fluorescent antibody testing has been replaced by nucleic acid amplification tests (NAATs) in combination with culture as the recommended tests of choice for B. pertussis detection. Currently, there is one FDA cleared platform for B. pertussis detection. Streptococcus pneumoniae and Haemophilus influenzae do not play an established role in acute bronchitis, but they, along with Moraxella catarrhalis, do figure prominently in cases of acute exacerbation of chronic bronchitis. Bronchiolitis is almost exclusively caused by viruses and M. pneumoniae. Several FDA-approved NAAT platforms are available for the detection of select respiratory viruses.
Ddx: hypersensitivity pneumonitis (less common in smokers, but more severe) or idiopathic ILD. Asthma. COPD and Emphysema. Pneumonia (Mycoplasma). Acute sinusitis. Aspiration. Bacterial tracheitis. Bronchiectasis. Cystic fibrosis. Influenza. Reactive airway disease. Retained foreign body. For children, consider bronchiolitis, croup, laryngotracheobronchitis, pertussis.
Acute Bronchitis (Tracheobronchitis):
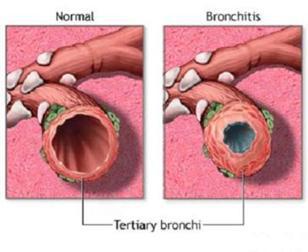
Inflammation of the tracheobronchial tree. Acute bronchitis affects about 5% of adults each year. Cough without pneumonia. The cough lasts up to 3 weeks and is only sometimes productive. The cause is usually infectious, but allergens and irritants can produce a similar clinical picture. Bronchitis typically occurs in the setting of an upper-respiratory illness and is therefore seen more frequently in the winter mo’s. Manifests as a severe or prolonged cough, can be clear or purulent sputum following infection by any of the respiratory viruses. Nearly always self-limited in the otherwise healthy individual, although it frequently results in absenteeism from work and school. Usually last 10 days, cough lasts 3 wks in 50%, 30days in 25%.
Triggers: Viruses (adeno, corona, coxsackie, entero, influenza, parainfluenza, RSV, rhinovirus), bacteria (B pertussis, Branhamella, H flu, S pneumo, atypical), yeast & fungi (Blastomyces, Candida, Coccidio, Cryptococcus, Histoplasma), Other (asthma, air pollution, ammonia, cannabis, tobacco, trace metals, other). In contrast to chronic bronchitis, acute bronchitis is a self-limited condition of the bronchi that is most often caused by viral infections in association with an URI or acute exposure to a nonspecific irritant such as ammonia. Acute bronchitis, however, may also occur as a transient complication of chronic bronchitis.
S/s: Seen in pt with acute URI that is manifested predominantly by cough, with or without sputum production, lasting <3 weeks, and no clinical or radiographic evidence of pneumonia, acute asthma, or an exacerbation of COPD. May have wheezing, rhonchi and prolonged expiratory phase. If suspect pneumonia get CXR and pulse Ox –> (mycoplasma/ chlamydia/ Bordetella, Viral). Purulent sputum does not signify a bacterial infection, it is primarily from sloughed off mucosal epithelial cells mixed with inflammatory cells from either viral or bacteria. >90% due to viral, non viral causes include Mycoplasma, Bordetella pertussis and C. pneumoniae (TWAR). A purulent cough is generally the defining presentation. May also have fever, malaise, rhinorrhea or nasal congestion, sore throat, wheezing, dyspnea, chest pain, myalgias or arthralgias. Occupational history may be important in determining whether irritants may play a role. The exam may include rhonchi or wheezes, but in most cases the examination is unremarkable. Bullous myringitis suggests Mycoplasma pneumoniae, although it is not specific. Conjunctivitis and adenopathy suggest adenovirus, although also not specific.
Tx: There is ample evidence that acute bronchitis should not be treated with antibiotics, except in patients with pertussis or significant underlying pulmonary disease. In healthy individuals, tell pt they have a “Chest Cold” when Abx do not appear indicated as pt’s have strong expectations for Abx associated with previous dx of bronchitis. –> Fluids, rest, cough suppression with Dextromethorphan (Robitussin DM)/ Codeine, vaporizers (use if low-humidity environment such as high altitude). + Bronchodilator (b-agonist) helpful if cough with evidence of airflow obstruction (wheezing), as may aid sx relief, but not change other outcomes (The Cochrane Library 2004;2).
Antibiotics: No need Abx if no prior h/o respiratory problems or underlying structural airway dz (See ENT module: Antibiotic & URI’s). Routine use of Abx is not recommended, regardless of duration of cough. Personalize the risks of unnecessary Abx use such as increasing the likelihood of carriage of and infection with antibiotic resistant bacteria, SE’s (GI, taste), risk of drug reaction. Finally explain to the pt that Abx resistance is a major public health concern and we need to be more selective in treating only those conditions for which a major clinical benefit is proven.
• Azithromycin no better than low-dose Vit-C (Lancet 2002;359:1648-54).
• Amoxicillin (1 g TID) was largely ineffective in patients with “acute bronchitis” (acute cough and sputum production) who had no evidence of pneumonia (Lancet Infect Dis 2013;13:123)(NNT = 30)…..At enrollment, 79% of participants produced sputum (discolored in about half); mean duration of illness was 9 days……With Abs, the duration of symptoms was not significantly difference between the antibiotic and placebo groups……the proportion of patients with new or worsening symptoms —was slightly lower in the amoxicillin group (16% vs. 19%; P=0.043; number needed to treat, 30). GI side effects were more common with amoxicillin (29% vs. 24%; P=0.025). Outcomes were similar in older and younger adults.
• Data from the UK General Practice Research Database suggest that failure to prescribe antibiotics when patients present with a lower respiratory tract infection may lead to higher rates of hospitalization and mortality (Chest 2009;135:1118-1120,1163-1172)….Of the 14% of the study cohort not treated with antibiotics on the day of presentation, 33% died…..question if we have gone too far in limiting antibiotic use in lower respiratory tract infections……They point out that the number of patients needed to treat to prevent death or hospital admission was well over 1000, so clearly, for most patients, antibiotics may not be necessary……”A cautious approach may be needed when deciding which patients should be treated, particularly in high-risk and vulnerable groups.”
• For patients with uncomplicated lower respiratory tract infection, amoxicillin (1 g TID x 7 days) does not reduce symptoms — and might cause “slight harms” (nausea, rash, and diarrhea) (Lancet Infectious Diseases. 2012;Early Online Publication, 19 Dec)….The authors conclude that “unless pneumonia is suspected, antibiotics should not be prescribed for patients with lower respiratory tract infection.”
• Data from 836 patients with a diagnosis of acute bronchitis from an ED in SanDiego found that 72% with no comorbid conditions were prescribed antibiotics (J Emerg Med 2012:Feb 16;e-pub ahead of print)…….Antibiotics were also prescribed to 81% with COPD; 76% with asthma……editorialist note that “A trial of bronchodilators is safe and reasonable and may satisfy patients’ desire for a prescription and warning patients that antibiotics carry significant risk of adverse effects and act throughout the body might help them realize that they are fortunate not to require antibiotics”.
Chronic Cough Due to Acute Bronchitis: Beta-2-agonist bronchodilators should not be routinely used to alleviate cough unless there is wheezing accompanying the cough. Antitussive agents are occasionally useful and can be offered for short-term symptomatic relief of coughing. Because there is no consistent favorable effect of mucokinetic agents on cough, they are not recommended (Evidence-based guidelines: Diagnosis and Management of Cough. Chest. 2006;129:1-25).
Kalwerbossis (Pelargonium sidoides, Geranium extract): 30 drops (11% aqueous extract of root) TID 30 minutes before or after a meal x 7 days may decreases overall sx’s, but no change in the resolution of the cough compared to placebo (Phytomedicine 2003;10:7-17). A RCT with 124 pt’s using pelargonium extract at a dose of 1.5 mL (30 drops) TID x 8 days found a significantly greater reduction in sx’s of acute bronchitis than placebo, and more pt’s were satisfied with tx (Explore 2005;1:437-45).
Links: Simple | Complicated | Bronchiectasis | COPD | See Obstructive |
Sputum production (usually AM) >3mo/yr X >2yrs. Seen in 30% of smokers. Persistent and irreversible inflammatory changes. Snoring may significantly increase susceptibility (25% risk) to chronic bronchitis (Arch Intern Med 2008;168:167-173)…..The combination of smoking and snoring almost tripled (68% risk) the likelihood of chronic bronchitis compared with those who did not smoke or snore. A key reason why some smokers develop chronic bronchitis and others don’t is that 40% of the risk for the condition is genetic, a study of twins here revealed (Am J Respir Crit Care Med 2008;177:486-490). …of 36,772 participants, chronic bronchitis was in 7.1% of the population, 8.08% of women versus 6.04% of men and 11.46% of current smokers versus 5.57% of never-smokers. Women in the Danish furniture industry with occupational exposure to wood dust have an increased risk of cough and bronchitis (Eur Respir J 2009;33:1268-1276).
Acute Exacerbation’s of Chronic Bronchitis (AECB): 60-65% bacterial (H. flu, S. pneumo, M. Cata, H. para), 30% viral (inf, parainf, rhino, corona, adeno, RSV), 5-10% atypical (Chlamydia, Mycoplasma pneumonia).
Chronic occult aspiration (mostly related to GERD) can lead to diffuse bronchiolar disease (Mayo Clin Proc 2006;81:172-176) (rather than the classic aspiration pneumonia or aspiration pneumonitis).
S/s exacerbation: dyspnea, incr sputum, purulent, worsening cough, malaise.
Vs Emphysema (Pink Puffer) –> incr sputum (mucopurulent) with persistent cough, starts younger (35 Vs 50yo), pt is stocky, has plethora, Incr HCT, ECG with RAD/ RVH/ P-pulmonale, +hypoxemia and hypercapnia.
ICD-9 Codes:
490 Bronchitis, not specified as acute or chronic
491.0 Simple chronic bronchitis
491.1 Mucopurulent chronic bronchitis
491.2 Obstructive chronic bronchitis
491.21 With acute exacerbation
492 Emphysema
Two types:
1. Simple Chronic / Usual COPD = <65yo, FEV1 >50%, <4 exacerbation’s/yr –> (Viral, H flu, Moraxella, strep pneumo)
Tx: chronic bronchitis should be offered ipratropium to control sx’s. May also benefit from the use of beta-agonists and theophylline. Smoke-free environment. For stable pt’s with chronic bronchitis and an FEV1 of < 50% predicted or for those pt’s with frequent exacerbations of chronic bronchitis, inhaled corticosteroid (ICS) therapy should be offered. Central cough suppressants such as codeine and dextromethorphan are recommended for short term symptomatic relief of coughing
If exacerbation, tx similar to COPD, #1 give Amoxicillin 500mg TID #2: Macrolides, Augmentin, TCN 500mg QID. Doxy 100mg BID. Minocycline, Quinolones or Septra DS BID. +0.5 mg/kg IV q6hr Methylprednisolone or PO Prednisone. + Atrovent and beta-agonist intensification therapy. For pt’s with acute bacterial exacerbations of chronic bronchitis, short-course (5-7days) therapy with cephalosporins, advanced generation macrolides/azalides/ketolides, and second-generation quinolones are all reasonable alternatives to the traditional therapies (Drugs 2003;63:2169-84). Older traditional Abx (amoxicillin or SMX-TMP) and newer broad-spectrum Abx (azithromycin) show no difference in outcome when used to treat AECB (South Med J 2003;96:986-991). For acute exacerbation, a short course (10 to 15 days) of systemic corticosteroid therapy should be given. Second-line Abx’s may be more effective than first-line Abx’s (amox, amp, doxy or TMP/SMX) for tx of AECB according to a meta-analysis (Chest. 2007;132:447-455)(clinical cure 2-fold better, but no significant differences in mortality, diarrhea, or overall adverse effects)….likely relatively resistant bacterial species as the etiologic agents among pt’s with impairment of lung function.
No benefit: Postural drainage and chest percussion have not been proven, and they are not recommended. There is no evidence that the currently available expectorants are effective and therefore they should not be used (Evidence-based guidelines: Diagnosis and Management of Cough. Chest. 2006;129:1-25).
2. Complicated COPD: >65yo, FEV1 <50%, >4 exac/yr or bronchiectasis –> (As above, plus G- rods & Pseudomonas).
Tx: Cefuroxime (Ceftin, Zinacef, Kefurox) 500mg BID. Cefprozil, Ceftibuten (Cedax) 400mg qd x10, costs $80. Cefixime (Suprax) 400mg qd x7 ~$58. Clarithromycin (Biaxin) 500mg BID, costs ~$72/10d. Augmentin 500mg BID,
Quinolone: Levaquin (Levofloxacin): 500mg qd X 7-14d, for CAP, chronic bronchitis, have low resistance to S. pneumo as requires mutation in 2 unlinked genes. Moxifloxacin (Avelox): 400mg PO qd. X5 days for chronic bronchitis. Cipro 750mg BID. Ofloxacin (Floxin) 400mg BID. All 2nd line Abx.
See Abx abd COPD Exacerbations |
**Ref: (Acute bronchitis. Lippincotts Prim Care Pract 1998;2:643-6) (Tx of acute bronchitis in adults without underlying lung disease. J Gen Intern Med 1996;11:557-62) (Diagnosis of Diseases of the Chest, 4th ed., 1999, WB Saunders) (Principles of appropriate antibiotic use for tx of acute bronchitis in adults. Ann Intern Med 2001;134:6) (Outpatient management of chronic bronchitis in the elderly. Am Fam Phys 1993;48:841-8) (Diagnosis of Diseases of the Chest, 4th ed., 1999, WB Saunders) (Postgrad Med 1996;99:4) (Acute bronchitis. NEJM 2006;355:2125-30)
Links: PP | S/s, Well’s Score | Labs | ECG | CXR | Dx & W/u | D-dimer | VQ | CT | Ddx | Tx |
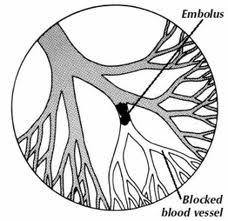
PE is the third most common acute cardiovascular disease after myocardial infarction and stroke. An estimated 650,000/yr. The dx of PE is frequently missed, the mortality is 20-30% in undiagnosed cases, however 60-90% deaths in 1st hr (with tx it has a 8-15% mortality). 80% of cases originate from leg DVT. 20% from pelvic/ arms/ R-heart. Even isolated greater saphenous vein thrombosis (superficial thrombophlebitis of the thigh) can embolize. 40-50% risk of PE with proven DVT of LE Vs 15% if UE (subclavian) DVT. Only 30-45% of those who died of PE had the correct antemortem dx (Chest 2001;120:791–5). Yet, 2/3 of those worked up for PE don’t have it. Roughly a third of 1665 patients (32%) with DVT have an asymptomatic PE according to a systematic review (Am J Med. 2010;123:426-431)…..lead author suggests a perfusion lung scan when chest x-ray is “nearly normal” or a ventilation/perfusion scan for an abnormal chest x-ray……Routine screening would provide a baseline if the patient later becomes symptomatic, and would prevent a misdiagnosis of failed therapy, the authors write.
PP: A partial or complete occlusion of pulmonary vasculature secondary to thrombus that usually originates from DVT of lower ext. Thrombus may be de novo in pulmonary circulation, right heart, or left heart via intracardiac shunt. There is a incr in the RV afterload when ~25% of the total pulmonary blood flow is acutely obstructed. When the pulmonary vasculature is obstructed 75%, the mean PA pressure approaches the max a normal RV can generate (40-45mmHg), this incr leads to incr RA pressure and decreased the cardiac index. This increases the afterload on the leading to failure and shock. Death occurs from circulatory obstruction, causing right heart failure, systemic shock, and hypoperfusion. Septic (bacterial) emboli may arise from tricuspid valve (IVDA), infected pelvic veins, infected shunts, or infected cardiac pacemakers. Incidence of PE rose dramatically (81% increase) after computed tomographic pulmonary angiography (CTPA) was introduced in 1998, but PE mortality did not decrease concomitantly (Arch Intern Med 2011;171:831)…..suggests substantial overdiagnosis of clinically unimportant PE…..given a 71% increase in anticoagulation complications illustrates how overdiagnosis leads to adverse outcomes — in this case, without apparent matching benefits……editorialist call for a randomized clinical trial to evaluate whether treating — versus observing — clinically stable patients with small PEs yields significant benefits.
Other sources: air, fat, amniotic fluid, cancer cells, Fb (wire tip).
Central location of PE (saddle or at least one main pulmonary artery vs lobar or distal = segmental or subsegmental arteries) increases the likelihood of poor outcomes (Chest 2012:May 24;e-pub ahead of print)….among 516 patients who were initially hemodynamically stable, central location of emboli was an independent predictor of all-cause death or clinical deterioration (HR, 8.3), as were age >75 years (HR, 2.6) and right ventricular dilatation measured by echocardiography (HR, 2.4)…..In hemodynamically stable patients, distal location of emboli was inversely associated with these outcomes (HR, 0.12)…..The degree of obstruction was greater in patients with right ventricular dilatation but did not predict poor outcome……The combination of multidetector CTA and echocardiography for determining location of the emboli and measuring right ventricular dilatation may lead to better management decisions for these patients.
Posttraumatic: Pulmonary Embolism can occur early after trauma (J Trauma 2007;63:620)…15% occurred within 48 hours after injury….Of 94 trauma pt’s with pulmonary embolism, 92.6% had one or more of tachypnea, tachycardia, or hypoxia…the average time to diagnosis was 11.8 days, 37% within 4 days, areas of injury included the thorax (37%), lower leg or femur (38%), pelvis (22%), and spinal cord (30%, with neurologic deficit in 54%).









