Links: CO2/bicarb | Sodium (Na) | Magnesium (Mg) | Potassium (K) | Calcium (Ca) | Phosphate (P) | Fluids | Chloride | See Intensive Glucose Control & GIK |
 Always repeat to r/o artifact (laboma). Laboratory errors are common. Results should be double-checked when the clinical picture and the lab data conflict. When altered, fluids and electrolytes should generally be corrected in the following order: (1) volume; (2) pH; (3) potassium, calcium, magnesium; and (4) sodium and chloride. Re-establishment of tissue perfusion often re-equilibrates the fluid-electrolyte and acid-base balance. Because the osmolarity of normal saline matches that of the serum, it is an excellent fluid for volume replacement. Abnormalities should be corrected at the same rate they developed; however, slower correction is usually safe unless the condition warrants rapid and/or early intervention (ie, hypoglycemia, hyperkalemia).
Always repeat to r/o artifact (laboma). Laboratory errors are common. Results should be double-checked when the clinical picture and the lab data conflict. When altered, fluids and electrolytes should generally be corrected in the following order: (1) volume; (2) pH; (3) potassium, calcium, magnesium; and (4) sodium and chloride. Re-establishment of tissue perfusion often re-equilibrates the fluid-electrolyte and acid-base balance. Because the osmolarity of normal saline matches that of the serum, it is an excellent fluid for volume replacement. Abnormalities should be corrected at the same rate they developed; however, slower correction is usually safe unless the condition warrants rapid and/or early intervention (ie, hypoglycemia, hyperkalemia).
ICD-9 Codes:
269.3 Mineral deficiency, not elsewhere classified
276.9 Electrolyte and fluid d/o’s not elsewhere classified – chloride
995.20 A drug adverse effect.
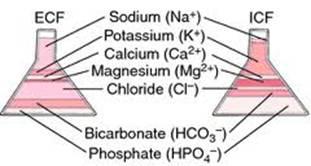
Bicarbonate: Major extracellular anion with Cl.
Basic Science: The kidneys and lungs maintain daily acidbase balance. Bicarbonate and carbonic acid constitute the major buffer pair in body fluids. Carbonic acid dissociates into hydrogen ion and bicarbonate with a dissociation constant of 7.95 x 107. Carbonic acid also maintains an equilibrium with H2O and CO2. We produce ~1 mEq/kg daily of hydrogen ions (derived from metabolism of proteins primarily). The kidney normally excretes this daily acid load. Failure of excretion forces the reaction of H+ and HCO3, resulting in a decrease of bicarbonate concentration.
Serum Total Carbon Dioxide: Measururing serum total CO2 content rather than just serum bicarbonate includes the serum bicarbonate as well as available forms of carbon dioxide (i.e., dissolved CO2 and carbonic acid). Generally, the serum bicarbonate comprises about 95% of the total CO2 content; thus we can use this measurement as an excellent estimator of serum bicarbonate. The total CO2 content normally equals 23 to 30 mEq/L of serum. Arterial blood gas (ABG) reports generally include a bicarbonate value. The blood gas machine measures pH and pCO2 and then calculates a bicarbonate value using the HendersonHasselbalch equation. Generally, a concurrent venous total CO2 content will exceed this value by < 2 to 4 mEq/L, of which 1 to 2 mEq/L represents the difference between venous and arterial blood; the remaining difference comes from dissolved CO2.
Sodium Bicarb: [325 mg (3.8 mEq), 650 mg (7.6 mEq) tabs. Powder: 120, 480 g. Injection: 4.2% (0.5 mEq/mL) (10 mL), 7.5% (0.89 mEq/mL), 8.4% (1 mEq/mL) (10, 50 mL). Injection, premixed: 5% (0.6 mEq/mL) (500 mL)] Each 1 mEq bicarbonate provides 1 mEq Na+. One g sodium bicarbonate provides 11.9 mEq each of sodium and bicarbonate. An alkalinizing agent and electrolyte.
Correction of metabolic acidosis: Calculate pt’s dose with the following formulas.
Adult: HCO3– (mEq) = 0.2 x weight (kg) x base deficit (mEq/L), OR HCO3– (mEq) = 0.5 x weight (kg) x [24 – serum HCO3– (mEq/L)].
Neonate, infant, and child: HCO3– (mEq) = 0.3 x weight (kg) x base deficit (mEq/L), OR HCO3– (mEq) = 0.5 x weight (kg) x [24 – serum HCO3– (mEq/L)].
Urinary alkalinization (titrate dose accordingly to urine pH): Child @ 84–840 mg (1–10 mEq)/kg/24 hr PO divided QID. Adult @ 4 g (48 mEq) x 1 followed by 1–2 g (12–24 mEq) PO Q4 hr. Doses up to 16 g (192 mEq)/24 hr have been used.
Info: Contra in respiratory alkalosis, hypochloremia, and inadequate ventilation during cardiac arrest. Use with caution in CHF, renal impairment, cirrhosis, hypocalcemia, hypertension, and concurrent corticosteroids. Maintain high urine output. Monitor acid-base balance and serum electrolytes. May cause hypernatremia (contains sodium), hypokalemia, hypomagnesemia, hypocalcemia, hyperreflexia, edema, and tissue necrosis (extravasation). Oral route of administration may cause GI discomfort and gastric rupture from gas production. For direct IV administration (cardiac arrest) in neonates and infants, use the 0.5 mEq/mL (4.2%) concentration or dilute the 1 mEq/mL (8.4%) concentration 1:1 with sterile water for injection and infuse at a rate no >10 mEq/min. The 1 mEq/mL (8.4%) concentration may be used in children and adults for direct IV administration. For IV infusions (for all ages), dilute to a maximum concentration of 0.5 mEq/mL in dextrose or sterile water for injection and infuse over 2 hr using a maximum rate of 1 mEq/kg/hr. Sodium bicarbonate should not be mixed with or be in contact with calcium, norepinephrine, or dobutamine.
Cardiac arrest: Bicarbonate administration in this situation may be detrimental. Administer according to results of arterial blood pH and PaCO2 and calculation of base deficit. Flush IV lines before and after use.
Adults – A rapid IV dose of 200 to 300 mEq of bicarbonate, given as a 7.5% or 8.4% solution.
Infants (2 years of age or younger) – 4.2% solution for IV administration at a rate not to exceed 8 mEq/kg/day to guard against the possibility of producing hypernatremia, decreasing CSF pressure, and inducing intracranial hemorrhage.
Initial dose – 1 to 2 mEq/kg/min given over 1 to 2 minutes followed by 1 mEq/kg every 10 minutes of arrest. If base deficit is known, give calculated dose of 0.3 × kg × base deficit. If only 7.5% or 8.4% sodium bicarbonate is available, dilute 1:1 with 5% dextrose in water before administration.
Severe metabolic acidosis: Administer 90 to 180 mEq/L (approximately 7.5 to 15 g) at a rate of 1 to 1.5 L during the first hour. Adjust to patient’s needs for further management.
Less urgent forms of metabolic acidosis: Sodium bicarbonate injection may be added to other IV fluids. The amount of bicarbonate to be given to older children and adults over a 4- to 8-hour period is approximately 2 to 5 mEq/kg, depending on the severity of the acidosis as judged by the lowering of total CO2 content, blood pH, and clinical condition. Initially, an infusion of 2 to 5 mEq/kg over 4 to 8 hours will produce improvement in the acid-base status of the blood.
Estimates of the initial dose of sodium bicarbonate may be based on the following equation:
0.5 (L/kg) × body weight (kg) × desired increase in serum HCO3- (mEq/L) = bicarbonate dose (mEq) or 0.5 (L/kg) × body weight (kg) × base deficit (mEq/L) = bicarbonate dose (mEq). The next step of therapy is dependent on the clinical response of the patient. If severe symptoms have abated, reduce frequency of administration and dose. If the CO2 plasma content is unknown, a safe average dose of sodium bicarbonate is 5 mEq (420 mg)/kg. It is unwise to attempt full correction of a low total CO2 content during the first 24 hours, because this may accompany an unrecognized alkalosis due to delayed readjustment of ventilation to normal. Thus, achieving total CO2 content of about 20 mEq/L at the end of the first day will usually be associated with a normal blood pH.
Neutralizing additive solution: One vial of neutralizing additive solution added to 1 L of any of the commonly used parenteral solutions including dextrose, sodium chloride, Ringer’s, etc, will increase the pH to a more physiologic range (specific pH may vary slightly). Some products such as amino acid solutions and multiple electrolyte solutions containing dextrose will not be brought to near physiologic pH by the addition of sodium bicarbonate neutralizing additive solution. This is due to the relatively high buffer capacity of these fluids. Avoid adding sodium bicarbonate to parenteral solutions containing calcium, except where compatibility is established; precipitation or haze may result. Norepinephrine, dopamine, and dobutamine are incompatible.








