Fig. 15.1
An electrocardiogram illustrating changes suggestive of myocardial ischemia (ST-segment depression in the anterolateral leads I, aVL, and V2–V6)
Questions
- 1.
- 2.
What are the electrocardiographic findings in myocardial ischemia and infarction?
- 3.
How are myocardial ischemia and infarction different?
- 4.
What is the management of perioperative myocardial ischemia and infarction?
- 5.
What is the prognosis of patients with myocardial ischemia or infarction following noncardiac surgery?
- 6.
Describe the role of preoperative cardiac evaluation in patient undergoing noncardiac surgery.
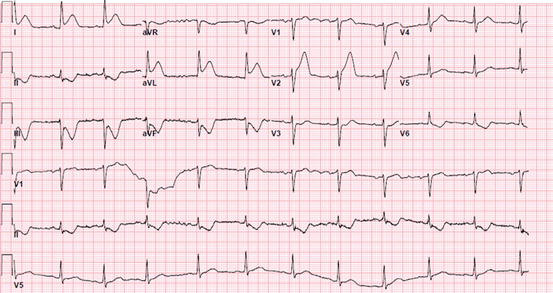
Fig. 15.2
An electrocardiogram illustrating changes suggestive of myocardial injury (ST-segment elevation in the lateral leads I and aVL)
Answers
- 1.
The figures represent electrocardiograms (ECGs) for patients presenting with chest pain. Figure 15.1 illustrates changes suggestive of myocardial ischemia (ST-segment depression in the anterolateral leads I, aVL, and V2–V6). The ECG shown in Fig. 15.2 depicts changes suggestive of myocardial injury (ST-segment elevation in the lateral leads I and aVL).
- 2.
ECG is considered to be an essential tool in the evaluation for myocardial ischemia or infarction. Changes to indicate myocardial ischemia or infarction include peaked or inverted T waves, ST-segment elevation or depression, and changes in the QRS complex [1]. ST-segment elevations present on the ECG accompanied by symptoms or signs concerning of myocardial infarction (including chest pain, dyspnea, or hemodynamic instability) are an emergency that require immediate attention. The threshold values for significant ST-segment elevation vary based on the gender and age of the individual [1]. For men 40 years of age or older, 2 mm elevation in leads V2 and V3 and 1 mm elevation in all other leads is considered to be significant. For men younger than 40 years old, a significant ST-segment elevation is 2.5 mm in leads V2 and V3. For women of all ages, ST-segment elevation of 1.5 mm in V2 or V3 and 1 mm in all other leads is considered to be significant.
- 3.
Myocardial ischemia results from an imbalance between myocardial oxygen demand and supply [2]. Myocardial oxygen demand is determined by the heart rate, myocardial contractility, preload (end-diastolic pressure or volume), afterload (arterial impedance), and muscle mass. Determinants of myocardial oxygen supply include coronary blood flow and arterial oxygen content [3]. Myocardial infarction (myocardial cell death) occurs if myocardial ischemia is prolonged (as little as 20 min or less). Myocardial infarction is characterized by myocyte necrosis as detected by elevated cardiac biomarkers (troponin-T, troponin-I (preferably), or CKMB) along with ischemia symptoms and ECG changes (as described above) [2].
- 4.
Perioperative management of patients with myocardial ischemia and infarction starts from early detection. Myocardial ischemia or infarction can be detected intraoperatively by ECG changes, ventricular arrhythmias, and hemodynamic instability [4, 5]. If myocardial ischemia or infarction is suspected, a 12-lead unfiltered ECG should be obtained promptly, and cardiac biomarkers should be sent. In addition, a transesophageal echocardiogram can be done (if readily available) to detect the ejection fraction and any new myocardial wall motion abnormalities. The surgeon should be informed to make a decision on completing versus aborting the surgery. If tachycardia along with normo- or hypertension is present, a beta-blocker (intravenous esmolol or metoprolol) or a non-dihydropyridine calcium channel blocker—if left ventricular ejection is normal—(intravenous diltiazem) should be administered [6]. Tachycardia along with hypotension is challenging. Evaluate and treat potential causes (e.g., hypovolemia or anemia). Vasopressors should be added to maintain mean adequate perfusion pressure (mean arterial blood pressure 65 mmHg or more). In cases of tachyarrhythmias (atrial flutter or fibrillation), direct current cardioversion may be necessary. If ST-segment elevations are present, an emergent cardiology consultation should be obtained to consider coronary angiography and revascularization. The management of patient with suspected myocardial infarction or ischemia in the postoperative period is as challenging given the limitations for the use of anticoagulants and antiplatelet agents. If based on symptoms, acute coronary syndrome is suspected, an ECG should be promptly obtained to assess for changes suggestive of ischemia or infarction. Oxygen should be administered if oxygen saturation is below 90%. Short-acting nitroglycerin (sublingual tablets or oral spray) should be administered to alleviate angina (avoid in hypotension). If there are no contraindications for antiplatelet agents, administer aspirin 162–324 mg oral [7]. Cardiology consult should be sought to direct further management. If changes suggestive of acute ST-segment myocardial infarction are present, cardiology should be contacted emergently. The decision to proceed with invasive coronary angiography should be decided based on the risk-benefit ratio analysis in any given patient weighing the risk of bleeding and the risk of ongoing myocardial ischemia.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






