Ear and Sinus Problems
Michelle Patrick RN, BSN, MSN, CPNP
Kenneth Steven Gottesman MD
Darsit K. Shah MD
PART 1 Ear and Sinus Problems for the Clinician
Michelle Patrick RN, BSN, MSN, CPNP
Kenneth Steven Gottesman MD
INTRODUCTION
Middle ear disease is one of the most important problems that primary care practitioners encounter. It is responsible for about 25% of infant visits to practitioners, and by kindergarten age, it may account for 40% of visits (Maxon & Yamauchi, 1996). Even when a child comes for a well visit, practitioners may diagnose otitis media in up to 10% of cases, especially if an upper respiratory infection (URI) is involved.
The accurate diagnosis of middle ear disease is not simple. Ear canals can be small and inevitably occluded by cerumen. Pediatric patients are often uncooperative and screaming. Bright red tympanic membranes (TM) often match the color of the angry toddler’s face but alone are not accurate predictors of the diagnosis.
The financial costs involved are immense. Even 20 years ago, the costs were approximately $2 billion for medical and surgical visits and procedures (Paradise & Rockette, 1997). Today, authorities estimate 30 million office visits and 23 million prescriptions are for otitis media in the United States alone (Klein, Marcy, & Paradise 1999).
OTITIS MEDIA
Anatomy, Physiology, and Pathology
The middle ear is a component of the upper respiratory passages. The other parts of this system are the nose, nasopharynx, eustachian tubes, paranasal sinuses, and mastoids. Respiratory mucosa lines all these structures. Researchers mostly agree that the eustachian tube is the key factor in the pathogenesis of middle ear disease. The structure and function of this conduit are almost inseparable when considering middle ear disease. The tube has three main functions:
Ventilation to allow pressure in the middle ear to equilibrate with atmospheric pressure and provide oxygen
Protection to keep nasopharyngeal secretions and sound pressure out of the middle ear
Drainage of secretions produced in the middle ear
The eustachian tube connects the middle ear to the nasopharynx. Its spatial relationship in the head is one important factor. In an adult, the tube is on an angle of 45 degrees in the horizontal plane. In an infant, the tube is on an angle of 10 degrees, is half the length of an adult tube, and has less cartilagenous support. Four muscles are around the eustachian tube. One of them, the tensor veli palatini, appears to be most actively involved in tube function. In the resting state, the eustachian tube is closed. Swallowing, yawning, or sneezing cause it to open, ventilating the middle ear. The tensor veli palatini appears to cause this dilatation.
Normally a slightly negative pressure is found in the middle ear. This pressure may become more negative when obstruction impairs the tube’s ventilatory function and the air in the middle ear is resorbed.
If at this point the eustachian tube opens, nasopharyngeal contents also may be aspirated into the middle ear, leading to infection. Another possible mechanism is reflux of nasopharyngeal contents, even in the absence of high negative middle ear pressure. This may occur if the tube is patulous due to abnormal muscular function. The shorter infant tube would promote both scenarios more readily, especially in the supine feeding position. A third mechanism might be insufflation of nasopharyngeal contents into the middle ear.
The tube also may be mechanically blocked. Extrinsic blockage may result from adenoidal hypertrophy or less commonly from a tumor. Intrinsic obstruction may occur due to inflammation, infection, or allergy. A classic study showed that in many cases, allergic rhinitis was contributory (Fireman, 1987). Because of immunoglobulin E (IgE) late phase reactants, frequent re-exposure to allergens may cause inflammation and secondary obstruction to persist for prolonged periods. (Intranasal challenge with house dust mites and histamine caused eustachian tube obstruction in patients with allergic rhinitis but not in normal controls). Less frequently, otitis media with effusion (OME) has been associated with immunodeficiencies, cleft palate (even post-repair), bifid uvulae (associated with a submucous cleft), and disorders affecting the normal clearance of nasopharyngeal secretions, ciliary dyskinesia, and immotile cilia syndrome.
The variety of bacterial pathogens isolated from the middle ear has remained unchanged over many years. When middle ear fluid is aspirated, bacteria are isolated in approximately two thirds of cases. Recently, the percentages of these isolates have changed, as have their resistance patterns. One must understand the concept of minimal inhibitory concentration (MIC) to understand how bacterial
resistance is measured. The MIC is the minimum amount of a drug that will inhibit bacterial growth in a test tube. It is the amount that one attempts to clinically deliver to the infection site for as long as possible between doses. If the antibiotic concentration exceeds the MIC for 30% to 40% of the time, organism eradication usually occurs. The ability to deliver high concentrations of antibiotic to an anatomic area depends on multiple factors, including route of administration, dose, absorption, blood supply to the target area, and metabolic clearance. In the middle ear, the relatively limited blood supply makes it difficult to achieve adequate MICs, especially in the context of emerging bacterial resistance.
resistance is measured. The MIC is the minimum amount of a drug that will inhibit bacterial growth in a test tube. It is the amount that one attempts to clinically deliver to the infection site for as long as possible between doses. If the antibiotic concentration exceeds the MIC for 30% to 40% of the time, organism eradication usually occurs. The ability to deliver high concentrations of antibiotic to an anatomic area depends on multiple factors, including route of administration, dose, absorption, blood supply to the target area, and metabolic clearance. In the middle ear, the relatively limited blood supply makes it difficult to achieve adequate MICs, especially in the context of emerging bacterial resistance.
Streptococcus pneumoniae (pneumococcus) is found in 40% to 50% of isolates. Although previously exquisitely sensitive to all penicillins, incidence of resistance has been increasing in the United States in the range of 34% (Dowell et al., 1999). The method of resistance relates to penicillin-binding proteins on the bacterial cell wall and creates a new classification of pnemococcus based on its susceptibility to penicillins. The MICs for penicillin are as follows:
Susceptible: less than or equal to 0.06 μg/mL
Intermediate: 0.12 to 1.0 μg/mL
Resistant: greater than 2 μg/mL
Approximately half of the resistant strains demonstrate absolute resistance and are now impervious to penicillin, however high the dose or MIC reached. The remaining half of intermediate or relatively resistant strains can be treated with higher than previously recommended doses of penicillin (Dowell et al., 1999). Factors associated with increasing pneumococcal resistance include antibiotic use within the past 3 months, age younger than 2 years, attendance in day care, recent hospitalization, and infection during the late winter or spring months (Pong & Harrison, 1998).
Haemophilus influenzae (H. flu) is found in 20% to 30% of isolates. These strains are almost all nontypeable. This organism may be more prevalent in older children and adults. Resistance is based on beta-lactam enzymes, which break down the lactam ring structure of penicillin. The percentage of lactamase producing H. flu varies by geographic locality and ranges between 30% and 90% (Dowell et al., 1999). The association of purulent conjunctivitis and otitis increases the likelihood of H. flu as an etiology (Bodor, 1982).
Moraxella catarrhalis (M. cat) is found in 10% to 15% of isolates. These are generally beta-lactamase producers and resistant to aminopenicillins in the range of 30% to 90% as well (Dowell et al., 1999).
Other bacteria may be occasionally isolated. These include group A streptococci, Staphylococcus aureus, and Pseudomonas aeruginosa. In the neonatal period, gram-negative enteric pathogens may be found; Chlamydia trachomatis also has been isolated in this age group. Bullous myringitis, characterized by TM blisters, is caused by the same pathogens as acute otitis media (AOM). Years ago, the etiology was thought to be Mycoplasma pneumoniae; however, this organism and Chlamydia pneumoniae may be etiologically implicated in association with disease of the lower respiratory tract.
More recently, viruses have been detected in approximately 30% to 40% of cases. The most common isolates are respiratory syncytial virus (74%), parainfluenza (52%), and influenzae virus (42%) (Heikkinen, Thint, & Chonmaitree, 1999). Some studies have found co-infection with viral and bacterial etiologies.
Epidemiology
With otitis media being one of the most common diagnoses pediatric practitioners make, one would expect many factors to be involved in its cause. This is certainly true, with genetic, familial, anatomic, allergic, and environmental components all contributing. Males have been found to have more acute and recurrent episodes in North America (Maxon & Yamauchi, 1996; Paradise & Rockette, 1997). An extremely high incidence is found in Native American and Eskimo populations. Children with Down syndrome and those with cleft palate also have a higher frequency, apparently as a result of the abnormal spatial relationship between the tensor veli palatini muscle and the eustachian tube seen in these conditions. Poor social conditions also predispose to a higher incidence of middle ear disease (Paradise & Rockette, 1997), suggesting that overcrowding, poor sanitation, and decreased access to medical care are contributing factors. Analogous to overcrowded conditions, children with older siblings and even more so, those in day care settings have a greater rate of occurrence because of their more frequent exposure to winter URIs. Infants who have their bottles propped or are fed in a supine position also have a higher incidence of MEE. Parental smoking and the use of pacifiers appear to be contributing factors as well (Niemela, Uhari, & Mottonen, 1995). Infants and children with respiratory allergies also may be at increased risk. Probably the most important determinant is a family history of middle ear disease. One important element that may help to protect against middle ear disease is if the infant is breastfed for at least 3 months (Paradise & Rockette, 1997).
History and Physical Examination
Forty percent to 50% of cases of AOM are associated with an ongoing URI, which on its own may cause irritability, fever, cough, decreased appetite, vomiting, and diarrhea.
• Clinical Pearl
Only half of patients with AOM have fever. Otalgia is the most specific symptom.
In the young infant, this is often represented by pulling on the ear, difficulty in swallowing, and discomfort when lying down. In the past several years, an association with purulent conjunctivitis has been noted, most often caused by nontypeable H. influenzae. A recent study from Finland confirmed that the most important symptom associated with AOM is otalgia (Kontiokari & Kolvunen, 1998). Sore throat and night restlessness were less strongly associated.
Being able to see the TM is not always easy. Many children do not like their ears to be examined. Cerumen is the bane of the practitioner’s existence. Providers often need to irrigate wax (a Water-Pik is very good for this procedure) or curette it out of the child’s ear canal (soft plastic-nylon disposable curettes are less traumatic than the older wire loop ones).
• Clinical Pearl
To assess the TM fully, one needs to consider its color, position, degree of translucency, and, most importantly, mobility. The diagnosis of middle ear disease cannot be made without some assessment of TM mobility.
Mobility assessment can only be accomplished with a pneumatic otoscope and insufflator or the use of tympanometry. The technique used in examining the patient depends on the child’s age and degree of cooperation. In the infant, having the child lie down, with the parent holding
the arms down at the patient’s side, is a reasonable technique. Another option is that the parent hold the child in the arms, with the head resting on the parent’s shoulder and cradled against the parent’s neck. Providers should always use the largest ear speculum possible. Pulling down slightly on the pinna will allow visualization of the TM. In the older child, providers may use the same technique but pulling straight back or up slightly on the pinna.
the arms down at the patient’s side, is a reasonable technique. Another option is that the parent hold the child in the arms, with the head resting on the parent’s shoulder and cradled against the parent’s neck. Providers should always use the largest ear speculum possible. Pulling down slightly on the pinna will allow visualization of the TM. In the older child, providers may use the same technique but pulling straight back or up slightly on the pinna.
The normal TM is grayish pink and translucent, with the characteristic cone of light progressing from the center of the drum in an anteroinferior direction. As the examiner looks at the drum, it is helpful to imagine one looking at the underside of an umbrella, with the center of the TM further away than the periphery. At the onset of AOM, the TM may be slightly retracted. As the process evolves, it becomes red, thickened, and may bulge outward. Slight redness of the upper part of the drum (pars flaccida) is usually normal, especially in the crying child. With resolution of the acute process, otitis media with effusion (OME), formerly referred to as serous otitis, commonly results and may persist for weeks. The TM is usually retracted, and fluid levels may be seen.
To evaluate mobility, one must use the insufflator by squeezing then releasing the bulb. A good example of a patient-centered technique is to gently squeeze the bulb against the child’s cheek, which serves in the dual role of reassurance and distraction before insufflating the TM. When normal, the TM will move inward when positive pressure is applied and move outward (return to its original position) when the bulb is released. Any fluid in the middle ear space will cause decreased mobility. If there is high negative pressure behind the drum (seen with eustachian tube dysfunction and resolving AOM), there will be no movement with positive insufflation, only on release of the bulb. With high positive pressure of the drum (eg, a bulging TM seen with AOM or severe OME), squeezing the bulb will either yield zero or diminished movement.
Often one sees an auditory canal filled with pus. This usually represents a perforated TM associated with AOM. Once the TM has perforated, the child usually feels better because the pressure in the middle ear has been relieved. In the child with tympanostomy tubes in place, this drainage also represents AOM.
The TM of the newborn requires special consideration. It is in a different position than the older child, being more horizontal. By about 1 month of age, it has moved into the position to which practitioners are accustomed.
Diagnostic Criteria
The diagnosis of AOM is based on criteria outlined in Table 33-1. Otalgia or evidence of otalgia in the young infant is the most important consideration. For differential diagnoses, providers should consider any condition that may cause otalgia. The most common conditions include the following:
Otitis externa (see separate section).
Pharyngitis; children often confuse throat and ear pain.
Eustachian tube dysfunction; this diagnosis may be appropriate for the child with a URI and a normal-looking TM, possibly with decreased mobility on pneumatic otoscopy.
Cervical adenitis.
Temporal-mandibular joint syndrome; the mandible forms one third of the auditory canal, and this pain therefore is easily referred to the ear.
Dental problems; teething, dental abscess, or postorthodontic adjustment may cause otalgia.
Diagnostic Studies
The following diagnostic studies may be used:
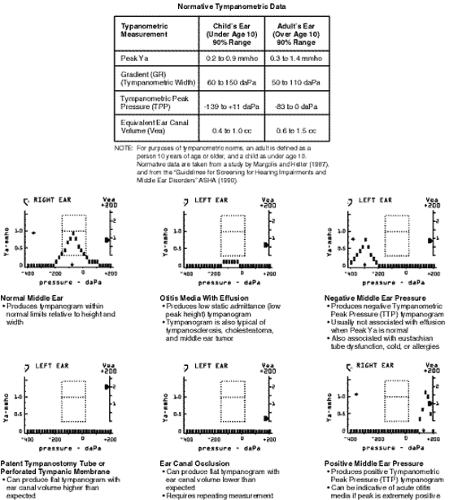
Tympanometry. This test uses an electroacoustic impedance bridge, which presents a tone through a small probe inserted at the opening of the external auditory canal. It measures the compliance of the TM while the pressure presented to the canal varies. It produces different patterns graphically. The mean tympanometric peak pressure (TPP) is usually normal between (–)150 to (+)11. A more negative TPP or a flat tympanogram is indicative of middle ear pathology. Most commonly, tympanograms are useful in the diagnosis of middle ear pathology or as an objective test in the follow-up of AOM or OME. They also are extremely useful in as-sessing TM integrity, as in perforations or patency of myringotomy tubes. In these situations, the measured ear canal volume would be abnormally high. Additionally, in the case of a child with cerumenous canals whose TMs are not able to be fully visualized, a normal tympanogram would be fairly conclusive evidence against AOM or OME. The reader is referred to Figure 33-1 for common typanogram patterns and their interpretations.
Tympanocentesis. Although usually thought of as a part of myringotomy and tubes (M&T), diagnostic tympanocentesis still has a place in the evaluation of AOM. The indications for this procedure are severe otalgia or toxic appearance, poor re-sponse to antibiotic therapy, AOM associated with suppurative complications, or the neonate or immunosuppressed patient, either of whom may harbor unusual organisms.
Management
Parents frequently have questions and concerns regarding the causes, treatment, and recurrence of otitis media. Caretakers are often unaware of preventive measures that may reduce their child’s risk of AOM and OME. Education also dispels some commonly held misconceptions. Parents frequently believe cerumen buildup contributes to OM. It is also not unusual for a parent to be concerned because their child is a little cranky and ear infections are “going around” at the day care or because their preverbal child is tugging on an ear. If physical examination reveals a relatively normal-looking TM with good mobility on pneumatic otoscopy, the provider has the opportunity to discuss with parents the true causes and more reliable signs and symptoms of AOM (ie, fever, prolonged cold symptoms, complaints of pain, or hearing loss in the verbal child). Some parents, especially
those whose child experiences of recurrent AOM, become familiar with their child’s “soft signs,” such as irritability, loss of appetite, and diarrhea, when concurrent with prolonged cold symptoms.
those whose child experiences of recurrent AOM, become familiar with their child’s “soft signs,” such as irritability, loss of appetite, and diarrhea, when concurrent with prolonged cold symptoms.
Another area of significant parental concern is that of hearing loss due to or associated with otitis media. Serosanguinous or purulent drainage from an ear canal, as well as the diagnosis of a perforated TM, can be alarming to parents. The image of a hole in the eardrum frequently causes fear of permanent hearing loss. Parents appreciate reassurance that the eardrum should heal, and the provider has a good opportunity to reinforce the importance of follow-up visits. OME may cause a transient conductive hearing loss. The older child with OME may complain of muffled sounds or tinnitus; the younger child may seem less responsive to parents’ voices. Reassurance that hearing loss is temporary and will last only as long as the effusion puts a parent’s mind at ease.
• Clinical Pearl
Parents need to know that OME is not an acute disease. Effusions commonly last up to 3 months following AOM.
Table 33-2 and Table 33-3 summarize parental instruction points regarding the nature and prevention of AOM/OME respectively.
Pharmacologic Treatment
Before the availability of antibiotics, AOM had potentially serious suppurative sequelae. Mastoiditis, brain abscess, epidural and subdural empyema, and meningitis were complications in up to 25% of cases. The use of antibiotics in the treatment of otitis media has decreased the rate of complications to less than 3% (Fliss, Leiberman, & Dagan, 1994). Recent emergence of penicillin-resistant S. pneumoniae strains, however, has prompted researchers and providers to reconsider the risks and benefits of liberal antibiotic use.
A 1998 literature review (Conrad) compared five small cohort studies (n < 280) that examined antibiotic treatment versus nontreatment of AOM. These studies showed that although antibiotic use provided relief of acute symptoms, they did not decrease the frequency of either long-term effusions (OME) or acute recurrences. A meta-analysis of 33 randomized trials involving 5400 children concluded that clinical symptoms of AOM resolved spontaneously in 81% of untreated cases (Rosenfeld et al., 1994). In 1994, Klein found a spontaneous cure rate of 60%. By examining middle ear fluid obtained by tympanocentesis, researchers have found that AOM due to M. catarrhalis and H. influenzae, as well as AOM of viral etiology, are far more likely to resolve spontaneously than AOM due to S. pneumoniae.
AOM remains a clinical diagnosis; it is impossible for the practitioner to determine the pathogens responsible based on findings at examination. Because tympanocentesis obviously cannot be performed on every child with AOM, antimicrobials continue to be the treatment of choice for all cases meeting diagnostic criteria.
Today, many cases of otitis media occur in children at risk for infection with a resistant organism. This problem prompted the issuance of a report on the treatment of otitis media in the era of pneumococcal resistance by the Drug-resistant Streptococcus pneumoniae Therapeutic Working Group (Dowell et al., 1999). This group emphasizes that when selecting a first-line drug for the treatment of AOM, efficacy against S. pneumoniae is paramount, because it is the most common bacterial cause. The other major pathogens, H. influenzae and M. catarrhalis, are more likely to produce disease with a high rate of spontaneous resolution. For these reasons, amoxicillin remains the best single choice for initial treatment of AOM (Dowell et al., 1999).
• Clinical Pearl
The child who is younger than 2 years, attends day care, or has been treated with antibiotics during the previous 3 months is at increased risk for infection with drug-resistant S. Pneumoniae (DRSP). For these children with AOM, amoxicillin 80 to 90 mg/kg/d (twice the usual recommended dose) should be the initial treatment.
The older child who does not have any other risk factors may be treated with what was previously considered the standard amoxicillin dose of 40 to 45 mg/kg/d (Dowell et al., 1999).
• Clinical Pearl
Treatment failure can be defined as a lack of clinical improvement in signs and symptoms, such as ear pain, fever, and TM findings (eg, redness, bulging, or otorrhea) after 3 days of treatment (Dowell et al., 1999).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree