Key Clinical Questions
What are the underlying physiologic mechanisms that result in dyspnea?
How can a physician elicit a patient’s personal description of shortness of breath in order to gain insight into the underlying diagnosis?
What physical exam findings are concerning for impending respiratory failure?
What are the key diagnostic studies a physician should order to further elucidate the cause of a patient’s dyspnea?
How can the disease states associated with dyspnea be organized into a clinical framework?
INPATIENT A 63-year-old woman describes shortness of breath on postoperative day 3 after a hip replacement. At 3 AM, the patient starts complaining that she “can’t catch her breath” and feels as though she is suffocating. she appears in acute distress upright with rapid, shallow breathing and expiratory grunting. Her blood pressure is 210/95 mm Hg with a heart rate of 120 beats per minute and an oxygen saturation of 92% while using supplemental oxygen at 6 liters/min by nasal cannula. On physical exam, auscultation of the lungs reveals rales over the lower one-third of the lung fields with dullness at the bases, as well as significant peripheral pitting edema. Since the patient has been receiving intravenous normal saline at100 cc/hour since the surgery, she is likely suffering from pulmonary edema. A chest radiograph (CXR) demonstrates increased interstitial markings and bilateral costophrenic angle blunting, which explain her clinical presentation. Increased interstitial edema activates a variety of receptors that stimulate the respiratory controller and cause air hunger, while pleural eff usions cause an increase in work of breathing by affecting the body’s ventilatory pump. The history, exam findings of hypertension, orthopnea, and rales, and the CXR findings help to confirm the diagnosis of volume overload. Other potential causes of dyspnea in an older patient who has undergone major surgery include myocardial ischemia, aspiration, and pulmonary embolism. In addition to treating congestive heart failure (CHF), it is important to seek out any underlying error that may have caused the condition and effect a system change that can improve quality of care for future patients. In the above case, indiscriminant use of maintenance fluids was the culprit; focused provider education and adjustment of existing order sets may be needed. |
|
Introduction
Dyspnea, or “shortness of breath,” is a common problem affecting up to half of patients in acute, tertiary care hospitals and one quarter of ambulatory outpatients. This sensation of breathlessness can be associated with anxiety, fear, or depression and, thereby, cause substantial disability. The American Thoracic Society consensus statement on dyspnea describes it as “an uncomfortable sensation of breathing,” which encompasses several qualitatively distinct sensations that reflect the subjective nature of the experience as well as the psychological, social, and environmental factors that contribute to the symptoms. A solid understanding of these distinct sensations and the pathophysiologic mechanisms underlying them can help physicians better understand, diagnose, and treat their patients.
Mechanisms of Dyspnea
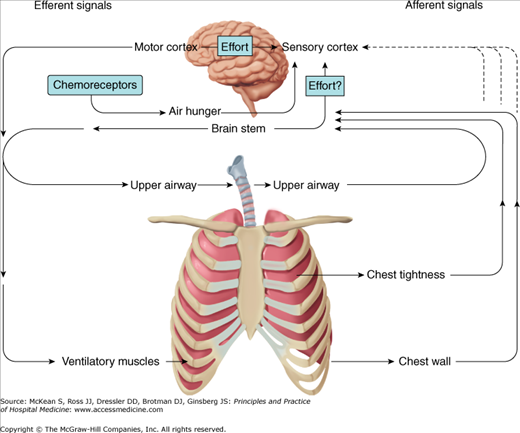
Similar to the feelings of thirst or hunger, the complex sensation of dyspnea is a visceral experience that integrates information from a number of sensory receptors and, in the case of dyspnea, is the consequence of a variety of pathophysiologic mechanisms. Dyspnea begins with a physiological impairment or stimulus that activates a range of sensory receptors that transmit incoming or afferent information to the cerebral cortex and to respiratory centers in the brainstem. Together, all the elements of the system that alter rate and depth of breathing can be considered the “respiratory controller”—akin to a thermostat—whose function is to set the rate and depth of each breath. Additionally, the brain sends efferent or outgoing neural messages to the muscles of ventilation, activating the “ventilatory pump.” Most often, a patient’s dyspnea can be attributed to abnormalities in one or both of these components of the respiratory system, and any additional mismatch between this motor feed-forward message and sensory feedback (ie, unsatiated air-hunger) increases the intensity of dyspnea (Figure 83-1).
Figure 83-1
The sense of respiratory effort is believed to arise from a signal transmitted from the motor cortex to the sensory cortex coincidently with the outgoing motor command to the ventilatory muscles. The arrow from the brain stem to the sensory cortex indicates that the motor output of the brain stem may also contribute to the sense of effort. The sense of air hunger is believed to arise, in part, from increased respiratory activity within the brain stem, and the sensation of chest tightness probably results from stimulation of vagal irritant receptors. Although afferent information from airway, lung, and chest-wall receptors most likely passes through the brain stem before reaching the sensory cortex, the dashed lines indicate uncertainty about whether some afferents bypass the brain stem and project directly to the sensory cortex.
Patients with disorders that affect the ventilatory pump experience an increased sense of “effort to breathe” or “work of breathing.” The ventilatory pump consists of peripheral nerves, muscles of ventilation, supporting skeleton, pleura, and airways; any disorder that affects these components can lead to an increased sense of the work of breathing. Hyperinflation causes dyspnea by placing the breathing muscles at a mechanical disadvantage and by forcing the patient to breathe at lung and chest wall volumes associated with reduced compliance, or greater stiffness of the respiratory system. The shortening of the inspiratory muscles that accompanies hyperinflation makes them less effective in generating tension. Furthermore, a change in the radius of the curvature of the diaphragm (it is relatively flat in patients who have hyperinflation) represents an additional load for the inspiratory muscles to overcome. In addition to hyperinflation, disorders such as chronic obstructive pulmonary disease (COPD) and asthma can also lead to increased airway resistance, further augmenting the work of breathing. Myopathies can cause muscular weakness, and kyphoscoliosis can lead to a stiff chest wall. Both of these conditions contribute to an increased sense of effort to breathe. Lastly, pleural effusions increase the work of breathing by expanding the chest wall and shortening inspiratory muscles, and may stimulate pulmonary receptors via associated atelectasis of regions of lung compressed by the fluid.
Patients with disorders that stimulate the respiratory controller experience the sensation of “air hunger.” Activation of receptors throughout the respiratory system—for example, irritant and stretch receptors in the airways and lung parenchyma, flow receptors in the central airways, and chemoreceptors in the carotid bodies and medulla—lead to stimulation of the control centers in the brainstem. We observe this as an increase in ventilatory drive (increased rate and depth of breathing, use of accessory muscles of ventilation, etc) and patients perceive a sense of an increased urge to breathe or air hunger. Interstitial edema activates J-receptors; inflammation activates C fibers; and acute changes in pulmonary artery pressure (eg, pulmonary emboli) activate C fibers in pulmonary vessels and pressure receptors in the pulmonary vasculature or right atrium. Changes in the metabolic rate during exercise affect metaboreceptors located in the skeletal muscle, which also contribute to uncomfortable breathing. Nondisease states, such as the hypoxemia associated with high altitude, pregnancy’s high progesterone state, and drugs such as aspirin, can also stimulate the respiratory controller and cause dyspnea. Furthermore, some receptors provide afferent input that leads to other sensations that can be interpreted as dyspnea. For example, bronchospasm stimulates mechanoreceptors in the lungs, which we believe leads to a sensation of chest tightness, which is sensed through vagal afferents, and may act as another stimulus for dyspnea (Table 83-1).
| Receptors | Disease States Causing Activation | Resulting Effect/Sensation |
|---|---|---|
| Chemoreceptors | Hypoxemia, acute hypercapnea, acidemia | Increase in ventilation; air hunger |
| J-receptors | Interstitial edema | Increase in ventilation; air hunger |
| C5 receptors | Inflammation | Increase in ventilation; air hunger |
| Pulmonary vascular receptors | Pulmonary embolism | Increase in ventilation; air hunger |
| Metaboreceptors | Exercise; increased metabolic rate | Increase in ventilation; air hunger |
| Mechanoreceptors Lung | Bronchospasm | Increase in ventilation; chest tightness |
| Mechanoreceptors Muscles | COPD, asthma, chest wall abnormalities | Sensation of increased work of breathing |
Some disorders, such as pneumonia, pulmonary edema, aspiration, pulmonary embolism, asthma, and COPD, not only contribute to dyspnea by the mechanisms outlined above, but also result in abnormalities in gas exchange. The hypoxemia, acute hypercapnea, and subsequent acidemia associated with these conditions activate chemoreceptors in the carotid bodies and medulla and cause an increase in ventilation to compensate for the ventilation/perfusion abnormalities, thereby contributing to the sensation of dyspnea.
EMERGENCY ROOM Recently diagnosed with asthma due complaints of intermittent dyspnea and occasional wheezing, a 54-year-old man presents with progressive shortness of breath for 2 days to the Emergency Department. He was recently given a diagnosis of asthma because of complaints of intermittent dyspnea and occasional wheezing. He states that breathing is a lot of work, he feels an increased urge to breathe, and sometimes he cannot get a full breath. His symptoms are worse with exertion. He denies problems when he goes out in cold air, but does have a chronic cough productive of small amounts of gray sputum. Although he initially claimed to have quit smoking a year ago (he has a 30 pack-year history of cigarette smoking), further questioning reveals that he has continued to smoke up to 1 pack of cigarettes a day, but has been trying to hide this from his wife. His blood pressure and heart rate are unremarkable, but his oxygen saturation is 88% on room air. On physical exam, auscultation of the lungs reveals distant breath sounds and intermittent expiratory wheezing. A CXR demonstrates hyperinflation with no evidence of infiltrates or effusions; heart size is normal. Physiologically, the patient is experiencing activation of his airway receptors and chemoreceptors, which stimulate the respiratory controller and increase his urge to breathe. Chronic hypoxemia, and potentially acute hypercapnea, may also be contributing to his sensation of dyspnea. Hyperinflation, which affects the efficacy of the ventilator pump and leads to reduced inspiratory capacity, contributes to the sensation of an unsatisfying breath (with increasing end-expiratory lung volume, the patient’s inspiratory capacity may literally be constrained by the limits of his lungs and chest wall to expand, ie, total lung capacity). Lastly, this patient may have dynamic airway compression that is sensed through vagal afferents as another stimulus for dyspnea. These physiologic mechanisms, coupled with the physical exam and radiographic findings, are consistent with a diagnosis of COPD exacerbation. Additional potential etiologies of dyspnea and wheezing in an obese smoker include CHF/pulmonary edema, pulmonary embolism, and myocardial ischemia; acute onset of asthma in a 50-year-old patient would be unusual without an antecedent respiratory infection. This case highlights the risk of anchoring bias, or the tendency to place too much importance on one piece of information, eg, a prior diagnosis of asthma. It is important to know what history is available before you see the patient, but you must then be disciplined to evaluate the patient with fresh eyes. |
|
Approach to the Patient with Dyspnea
Dyspnea as a symptom must be differentiated from the physical signs associated with “respiratory distress,” such as tachypnea, use of accessory muscles of respiration, or intercostal retractions. In describing a patient’s dyspnea, one should be careful to elicit the patient’s own qualitative descriptors of their dyspnea, rather than use general terms that reflect the physical signs observed, such as “labored breathing.” Common to these individual descriptors is the concept of “discomfort in the act of breathing,” but it is the subtle differences in a patient’s descriptors that may help elucidate the underlying physiological mechanisms.
The descriptor, “shortness of breath,” reflects different sensations in patients with differing etiologies and mechanisms of their discomfort. The varied and overlapping vocabulary chosen by patients to describe their dyspnea relate to the different physiologic factors that produce each particular form of dyspnea (Table 83-2).
| Qualitative Descriptor | Pathophysiologic Mechanism (Disease States) |
|---|---|
| Chest tightness or constriction | Bronchoconstriction (asthma), interstitial edema (myocardial infarction) |
| Increased work of breathing, effort to breathe | Airway obstruction (COPD, moderate to severe asthma), neuromuscular disease (myopathy), chest wall disease (kyphoscoliosis) |
| Air hunger, need to breathe, urge to breathe |