Do Patients with Congenital Insensitivity to Pain Need Anesthetics and Postoperative Opioids?
Katarina Bojanic MD
Toby N. Weingarten MD
Juraj Sprung MD, PhD
HEREDITARY SENSORY AND AUTONOMIC NEUROPATHY
Congenital hyposensitivity to pain, hereditary sensory and autonomic neuropathy (HSAN), is a group of rare genetic disorders characterized by varying degrees of sensory loss, including nociceptive hyposensitivity, loss of other types of sensation, and various degrees of autonomic dysfunction. Sensory loss, especially the loss of pain sensation, is associated with selfmutilation that may require frequent surgery (Fig. 168.1). Little is known regarding whether or how much these patients require anesthesia for surgery or opioids postoperatively. Furthermore, because of various degrees of autonomic dysfunction, these patients may be at increased risk of perioperative anesthetic complications.
CLASSIFICATION OF CONGENITAL HYPOSENSITIVITY TO PAIN
Congenital hyposensitivity to pain disorders were categorized by Dyck et al. into five different types of HSANs (I-V). Different expressions of sensory loss are possible within each HSAN category, and some patients may have variable pain sensation. The types of HSAN are distinguished by the mode of inheritance, clinical features, degree of autonomic nervous system abnormalities, loss or degeneration of sensory fibers, and increasingly specific molecular genetic abnormalities:
HSAN I is the only autosomal dominant disorder. It is characterized by onset later in life and a sensory deficit that is more pronounced in the legs than in the hands. In HSAN I, sensory deficits overshadow autonomic dysfunction.
HSAN II patients tend to have pain hyposensitivity of the upper and lower limbs. Many have defective tactile sensation, whereas a minority may have areas of normal trunk sensation. Relevant autonomic dysfunction may include episodic hyperthermia and swallowing deficiencies.
HSAN III, also known as Riley-Day syndrome or familial dysautonomia, has a higher prevalence in Ashkenazi Jews. These patients typically present in infancy with a profound dysautonomia (poor feeding with repeated vomiting, failure to thrive, and temperature and vasomotor dysregulation
associated with hypertension or hypotension), recurrent pulmonary infections, diminished peripheral pain and temperature sensation, and absence of vibratory perception.
HSAN IV, also known as congenital insensitivity to pain with anhidrosis, is characterized by hyposensitivity to superficial and deep visceral pain, mild to moderate mental retardation, and recurrent episodes of hyperpyrexia due to absence of sweating (no innervation of sweat glands).
HSAN V, also known as congenital insensitivity to pain without anhidrosis, resembles HSAN IV but is associated with a selective absence of small sensory myelinated fibers (Aδ fibers), which are important for sensing the sharp, well-localized, and prickling sensations of pain. These patients typically respond to tactile, vibratory, and thermal stimuli.
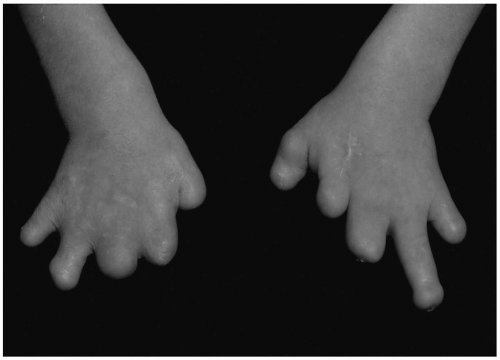 FIGURE 168.1. The hands of a 12-year-old boy with hereditary sensory and autonomic neuropathy (HSAN) II showing acromutilation. This type of self-mutilation may be found in all types of recessively inherited HSANs and is attributed to loss of pain sensation, neglect of injury, excessive surgery, and indifferent personality. (From Weingarten TN, Sprung J, Ackerman JD, et al. Anesthesia and patients with congenital hyposensitivity to pain. Anesthesiology. 2006;105:338-345. Used with permission.)
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|
