DIVERTICULITIS
CASE SCENARIO
A 47-year-old man presents to the emergency room with 3 days of abdominal pain. The pain is localized in the left lower quadrant and suprapubic area. He has a low-grade fever (100.5°F), decreased appetite, and diarrhea. His pain has progressively worsened over the past few days, and today he is having discomfort with walking and getting out of bed. He has no previous history of similar episodes.
On physical examination, he is an obese man in mild distress. He has a temperature of 100.5°F and heart rate of 100 beats per minute. He has left lower quadrant tenderness on examination with focal peritoneal signs. He has leukocytosis of 17.5 with 85% neutrophils.
EPIDEMIOLOGY
Diverticulosis, an outpouching in the colon, was first described in the 19th century and was considered to be a rare incidental finding. However, with an increased average population age and adoption of the Western diet in industrialized nations, rates of diverticulosis were noted to skyrocket to an estimated >80% by the age of 80 in the United States over past 30 years.1 Diverticulosis remains an asymptomatic condition, usually noted incidentally on imaging or colonoscopy. Only a small proportion of patients with diverticulosis will develop a problem—either diverticular bleeding or diverticulitis.
Although hard to estimate, approximately 10% to 20% of patients with diverticulosis will develop symptoms of diverticulitis. Of these patients, only 10% to 20% will be hospitalized, and less than half of hospitalized patients will require surgical intervention. This translates into roughly 1% of patients with diverticulosis who will need surgical resection.2
Diverticulitis can present in all age groups, but is most common in older patients (although in the Western world there has been a trend toward a younger age at presentation). Although younger patients tend to have higher rates of complicated diverticulitis and need for surgery, recent studies indicate that this is likely a function of age, rather than a different aspect of the disease. Men and women are affected equally, but men tend to present at a younger age and women tend to have a more fistulizing disease.
Diet is considered to be extremely important in the development of the disease, with a lifelong high-fiber diet being protective and a Western, low-fiber diet a risk factor. This is evident by increased rates of the diverticular disease in the population adapting a Western diet, as well as comparative studies between Western and Mediterranean type diets. There is no evidence, however, that adopting a high-fiber diet after development of diverticulosis (or a first attack of diverticulitis) decreases the chance of further diverticulitis. The use of opiates, nonsteroidal anti-inflammatory drugs (NSAIDs), cigarettes, and alcohol has also been proposed as risk factors; however, the data for this is not conclusive. Immunosuppression, meanwhile, is a very significant risk factor, correlated with higher rates of complicated disease, perforation, surgical intervention, and mortality.
PATHOPHYSIOLOGY
The cause of diverticulosis is thought to be high intraluminal pressures, predisposing to herniation of mucosa through muscular defects from penetrating blood vessels (vasa rectal brevia). Thus, most of the diverticuli seen are pseudo-diverticuli secondary to pulsion. This process explains why the sigmoid colon is the most common site of diverticulitis (90% of the disease)—it is the narrowest portion of the colon with the highest pressure. It is hypothesized that fiber protects against diverticular disease by bulking the stool and increasing the diameter of the sigmoid colon, thus decreasing the pressure. Functional abnormalities, e.g., cellular hypertrophy, slower muscle relaxation, and constipation have been noted in these patients. Additionally, patients with polycystic kidney disease have significantly higher rates of diverticulitis when compared to the general population, and so connective tissue problems may contribute to the development of the disease. Of note, diverticuli within the right colon are true diverticuli involving all layers of the colonic wall and usually represent a congenital process.
CLINICAL PRESENTATION
Diverticulitis can be divided into acute or chronic, as well as complicated or uncomplicated. Uncomplicated acute diverticulitis refers to localized inflammation confined to the colonic wall and surrounding tissues. It is usually accompanied by localized pain, cramping, fever, occasional diarrhea, and leukocytosis. Physical examination depends on the location of the disease, but usually involves localized abdominal pain, mostly left lower quadrant and suprapubic, with signs of local peritonitis, i.e., rebound and voluntary guarding. Occasionally the patient will present with isolated diverticular disease in a location other than the sigmoid colon, in which case symptoms will depend on location of the disease. Pain can radiate to the back if inflammation is mostly retroperitoneal or to the right in patients with redundant sigmoid.
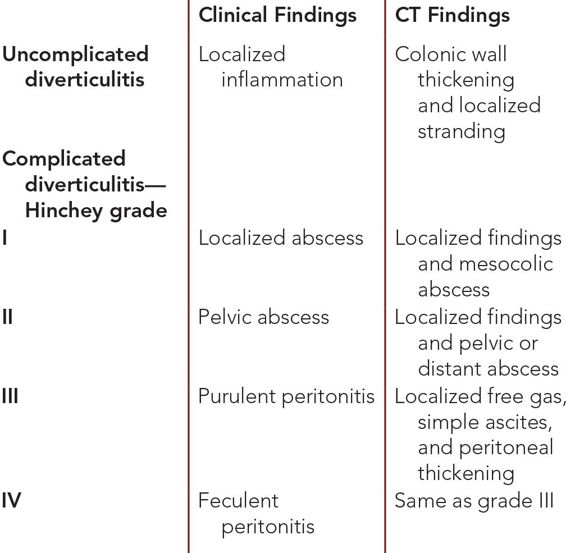
Acute complicated diverticulitis is classified by Hinchey criteria, first published in 1978 based on clinical findings (Table 8–1). Since that time, a number of new schemas have been proposed to incorporate radiological findings by computed tomography (CT). However, none have been shown to alter clinical care. Presentation will again vary from minimal symptoms to generalized peritonitis and septic shock. Some patients will be remarkably asymptomatic despite significant radiologic and clinical inflammatory findings. This is especially true for immunosuppressed patients who, despite minimal symptoms, may have significant disease that carries substantial morbidity and mortality if not recognized in a timely manner.
Chronic diverticulitis refers to persistence or frequent recurrence of symptoms despite standard treatment. This can include frequent attacks that improve with treatment, or patients who never completely return to baseline after an initial attack. Most of these patients will present on an outpatient basis, often with the diagnosis of multiple attacks. Thorough history should be taken to understand the true nature of their disease.
Complex diverticular disease refers to patients who develop sequelae of chronic inflammation, such as fistula, stricture, and obstruction. Fistulas are caused by a local inflammatory response or infection that involves nearby organs, and is seen in approximately 2% of patients. Colovesicular and colovaginal fistula are the most common types. In colovesicular fistula, patients often report passing gas and stool while urinating, frequent multibacterial urinary tract infections (UTIs), and, occasionally, pain. Colovaginal fistula patients, especially in women after hysterectomy (very rarely colouterine fistula), present with feculent discharge from the vagina, UTIs, and vaginal discomfort. Occasionally, patients will present with a colocutaneous fistula, either as a result of an abscess that eroded into the abdominal wall or at the site of an interventional radiology drain that never healed.
Stricture and obstruction are caused by frequent inflammation-scarring cycles. In addition to pain, these patients can present with nausea, vomiting, constipation, and large-bowel obstruction. In a few patients, large-bowel obstruction will be the first presenting symptom of diverticulitis. However, malignancy has to move up to the top of the differential diagnosis in these scenarios.
Bleeding is very rare with diverticulitis, and often indicates fistulization or another complicating process. Right-sided diverticulitis is a congenital condition and most often presents with signs and symptoms similar to appendicitis.
It is important to point out that the first episode of diverticulitis tends to be the most severe one, and is more likely to be associated with perforation. In addition, most of the patients with multiple attacks will have very similar presenting symptoms and can often anticipate the attack coming very early in its course.
DIFFERENTIAL DIAGNOSIS
Irritable bowel syndrome can be difficult to distinguish from diverticulitis. Symptoms will often be very similar to acute diverticulitis, but these patients are unlikely to have radiologic signs of inflammation or respond to standard medical treatment. However, there seems to be a significant overlap between these two diseases, and they may be on the continuum of the same process.3
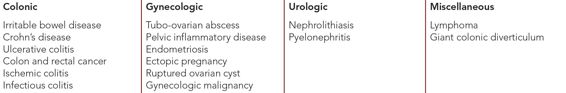
Malignancies, colonic as well as others, can present with signs and symptoms of diverticulitis, especially if they are associated with perforation and abscess. Imaging does not always provide the answer to this question, and a high index of suspicion should be used in the operating room to ensure proper surgical procedure (Table 8–2).
WORKUP AND CHOICE OF IMAGING
Once diverticulitis is suspected based on history and physical examination as well as laboratory studies, imaging should be performed. Diverticulitis is a radiologic diagnosis, with CT scan being a gold standard. In addition to helping differentiate between diverticulitis and other processes, CT can provide accurate localization as well as elucidate the severity of disease.
Plain abdominal radiographs are generally not very useful unless free perforation is suspected in unstable patients, and in these cases they can be quickly done to document pneumoperitoneum. Contrast studies (barium and water-soluble contrast) have been replaced by CT scans, but can still be useful in the evaluation of colonic obstruction and fistula.
Ultrasound has been shown to be reasonably accurate, especially in the rectosigmoid region if combined with transrectal ultrasound, but is very operator dependent, and can be limited in patients with pain. Thus, it has not gained widespread use.
Magnetic resonance imaging/magnetic resonance enterography (MRI/MRE) can also be extremely useful in patients with whom CT may not be possible, and when other problems such as gynecological malignancy and inflammatory bowel disease need to be ruled out. They can also be very useful in diagnosing fistulizing and stricturing disease.
Cystograms can be performed in patients with suspected colovesicular fistulas. Cystoscopy is rarely useful unless bladder malignancy is suspected.
Colonoscopy has been traditionally recommended to all patients who develop diverticulitis. However, it is not always needed. The main reasons to perform colonoscopy would be to rule out malignancy (although in cases of stricture this is not always possible) and to clear the rest of the colon. The rates of identifying polyps and malignancy in patients needing surgery for diverticulitis are not significantly different compared to the general population.4 For patients who are close to screening age, have risk factors, have an unclear presentation, or will be having surgery, colonoscopy, or another modality to interrogate the colon, should be entertained.
Since most subsequent attacks will have a very similar presentation, once diverticulitis is definitively diagnosed by CT scan, repeat imaging oftentimes can be avoided and the patient can be treated based on symptoms.
IMAGING FINDINGS
 CT Scan
CT Scan
The hallmark features of diverticulitis on CT scan include the presence of colonic diverticula as well as pericolonic inflammation. Specific findings indicative of inflammation include colonic wall thickening, pericolonic fat stranding (seen as gray haziness adjacent to the colonic wall), and free fluid. Free air is often present and is best appreciated on lung windows as black foci outside the bowel lumen. In focally perforated diverticulitis, free air is often localized to the colon, but in the setting of a free perforation with uncontrolled contamination of the abdominal cavity, air may be seen tracking in the upper abdomen and along the falciform ligament. Abscess can also be appreciated as fluid collections along the colonic wall, or adjacent to the colon and in the pelvis. In delayed presentations of complicated diverticulitis, these fluid collections can be rim enhancing (bright) (Table 8–3 and Figures 8–1 through 8–10).