Chapter 56 Disseminated Intravascular Coagulation
2 Why is DIC important?
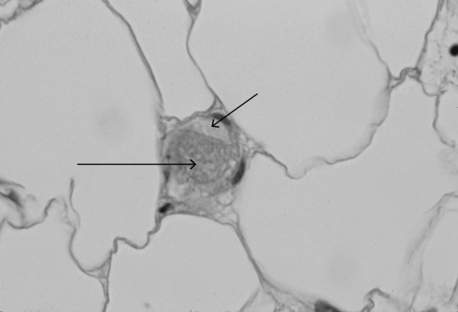
DIC is a common cause of concurrent thrombocytopenia and prolonged clotting times (activated partial thromboplastin time [aPTT] and prothrombin time [PT]) in hospitalized patients. It can also be an independent predictor of mortality. DIC leads to fibrin and platelet deposition in small vessels, which can cause tissue ischemia and result in organ dysfunction (Figure 56-1). The consumptive coagulopathy can also lead to clinically significant bleeding.
4 In critical care patients, what conditions are associated with DIC?
 Malignancy: adenocarcinoma, acute promyelocytic leukemia (incidence approaches 100%)
Malignancy: adenocarcinoma, acute promyelocytic leukemia (incidence approaches 100%)
 Obstetric: hemolysis, elevated liver enzymes, and low platelet count (HELLP) syndrome; retained uterine placental or fetal tissue; placental abruption or previa; amniotic fluid embolus
Obstetric: hemolysis, elevated liver enzymes, and low platelet count (HELLP) syndrome; retained uterine placental or fetal tissue; placental abruption or previa; amniotic fluid embolus
 Vascular: vasculitis, abdominal aortic aneurysm, cavernous hemangiomas
Vascular: vasculitis, abdominal aortic aneurysm, cavernous hemangiomas
 Miscellaneous: burns, anaphylaxis, transfusion reaction, snake bite, acute pancreatitis, transplant rejection, intravenous anti-D immunoglobulin
Miscellaneous: burns, anaphylaxis, transfusion reaction, snake bite, acute pancreatitis, transplant rejection, intravenous anti-D immunoglobulin
5 How does DIC present clinically?
In acutely ill hospitalized patients, DIC usually presents with prolongation of the PT and aPTT along with decreased fibrinogen and platelets; systemic bleeding may or may not be present. Typically, bleeding manifests as ecchymoses, purpura, petechiae; it also occurs at surgical incisions or insertion sites of vascular access catheters. Mucosal and urinary bleeding are common, whereas pulmonary, gastrointestinal, and central nervous system bleeding occur less frequently. Because of widespread intravascular coagulation, tissue ischemia can occur, resulting in cyanosis, delirium, oliguria, hypoxia, and frank tissue necrosis (Figure 56-2).
7 Is the peripheral blood smear useful in the diagnosis of DIC?
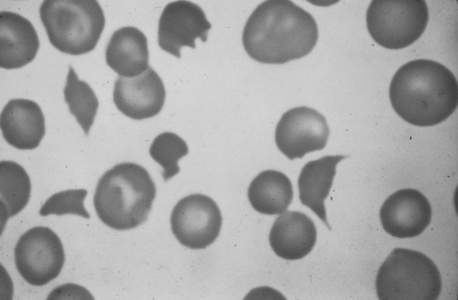
The peripheral blood smear from a patient typically shows mild to moderate thrombocytopenia. The finding of schistocytes (red blood cell fragments created by intravascular hemolysis) (Figure 56-3) is neither sensitive nor specific, and schistocytes are present in only 10% to 50% of cases of acute DIC. If present in DIC, there are usually only one to four per high-power field, in contrast to thrombotic thrombocytopenic purpura where they are much more abundant.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree